Abstract
Introduction
Arthroscopic management of the hip capsule has become a topic of debate in recent literature. Few comparative studies exist to help establish clear treatment recommendations.
Methods
Utilizing the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, a systematic review of the literature was conducted using PubMed, CINAHL, EMBASE, sportDiscus (EBSCO) and Cochrane Central Register of Controlled Trials databases by two independent investigators. Comparative studies evaluating outcomes after two or more distinct treatment approaches to capsule management were included.
Results
The review yielded 7 articles that met inclusion criteria. Outcomes included in the review include patient reported outcome measures (mHHS, HOS, NASH) in 5 articles, return to sport in 1 article, and formation of postoperative heterotopic ossification (HO) in 1 article. In two articles evaluating the outcomes of revision hip arthroscopy, plication was associated with > 10 point improvements in HOS-ADL and mHHS scores when compared to no plication. The literature is inconclusive regarding routine hip capsule closure in primary arthroscopy, with one study supporting the practice, and one study showing no difference; capsular closure may help accelerate return to sports and improve outcomes while decreasing revisions in cases of borderline dysplasia. Closure does not influence HO rates after surgery.
Conclusion
There is insufficient evidence in the present literature to suggest routine closure of inter-portal capsulotomies after primary hip arthroscopy impacts patient outcomes. Capsular closure or plication should be given strong consideration in revision cases. Complete closure or plication may influence outcomes in patients with borderline dysplasia, for athletes wishing to return to sport, and in cases of extensile capsulotomies, although the data are inconclusive. Prospective, high level studies are indicated to create evidence-based treatment recommendations for capsular management in hip arthroscopy.
Keywords: sports medicine, outcomes, illiofemoral ligament, hip capsule, hip arthroscopy
Introduction
Arthroscopic management of the hip capsule has gained significant interest and is a topic of much debate.1,2 Capsulotomy allows for improved arthroscopic access to the joint and facilitates better visualization and treatment of cam deformities, which is important as uncorrected deformity is the most common indication for revision hip arthroscopy.3-5
The hip capsule is an important soft tissue stabilizer of the femoroacetabular joint and is comprised of the iliofemoral, pubofemoral, and ischiofemoral ligaments. The zona orbicularis and iliocapsularis are intimately associated and play an important role in maintaining hip stability. From a biomechanical and anatomic prospective, the hip capsule has been extensively studied.6-9 A capsulotomy connecting the anterolateral portal to the anterior portal results in near-complete transection of the iliofemoral ligament (the thickest portion of the capsule), important in resisting anterior hip translation and external rotation.6,7 If these capsulotomies are repaired, cadaveric data suggest normal hip stability can be re-approximated6,8,9.
Outcomes following hip arthroscopy for femoroacetabular impingment (FAI) using inter-portal capsulotomies have historically been favorable without capsular closure.10 Despite this, the popularity of routine capsular closure has increased in the absence of high level evidence.1 There is significant debate in the literature regarding the influence capsular closure has, if any, on patient reported outcomes.11, 12 The purpose of this review was to systematically evaluate the available literature for comparative studies of different hip capsule management techniques (including plication, full, partial, or no closure) to determine if specific capsular management strategies influence outcome. We hypothesized that cases of borderline dysplasia would have improved outcomes with closure or plication and routine inter-portal closure of capsulotomies would not be associated with patient reported outcomes.
Methods
A systematic review of the literature was performed on December 2, 2016 by two independent reviewers (RWW and MCB) according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.13, 14 Databases queried included PubMed, CINAHL (EBSCO), Embase (Elsevier), Sport Discus (EBSCO), and Cochrane Central Register of Controlled Trials (Wiley). Searches were performed without filters for all public databases except for EMBASE where conference abstracts were excluded. In the event of a disagreement between reviewers, the lead author decided on paper inclusion.
Inclusion Criteria
English language studies published between 1980 and December 2016 on human subjects treated with hip arthroscopy were considered if they compared outcomes (patient reported outcomes (PROs), return to sport, heterotopic ossification, reoperation) between two different capsular management techniques. These include but were not limited to “complete versus partial closure”, “closure versus no closure” and “plication versus closure or no closure”.
Exclusion Criteria
Studies reporting outcomes after hip thermal capsulorrhaphy and those that did not compare outcomes between two different capsule management strategies in a given manuscript were excluded.
Quality Appraisal
Two independent non-blinded reviewers (RWW and MCB) assessed the quality of the included studies according to the modified Coleman Methodology Score (MCMS).15 The quality of studies was compared between groups with respect to the cohort studied (primary FAI, revision FAI, dysplasia, etc). Comparisons were made using 2-sample Student t tests; significance was set at p < 0.05.
Results
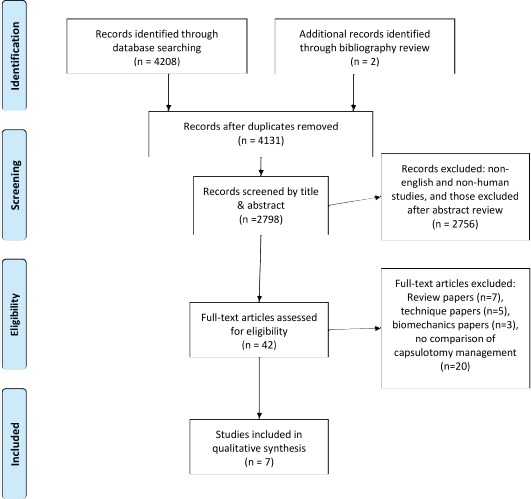
Seven studies met inclusion criteria after review.11, 12, 16-20 [Figure 1]. Validated patient reported outcome instruments were used to compare patients treated with different capsular management techniques in 5 studies; 11, 12, 18-20 of these, 2 studies focused on outcomes after primary hip arthroscopy for FAI,11, 12 2 studies evaluated the influence of capsular repair in revision FAI settings18, 20, and one studied capsular management in a dysplastic cohort.19 Other primary outcomes were the ability to return to sport17 and the development of heterotopic ossification after hip arthroscopy16.
Figure 1. Systematic Review flowchart. There were 4131 unique articles identified using our search criteria; after application of inclusion and exclusion criteria, 7 studies were included in the qualitative analysis.
Primary Hip Arthroscopy
Two studies evaluating cohorts undergoing primary hip arthroscopy were identified that compared complete capsular closure with either partial or no closure using revision rates and validated outcome instruments as outcomes.11, 12 Frank, et al., compared PROs between those who underwent partial closure (closure of the vertical aspect of the T capsulotomy) versus complete closure (including the horizontal component). They determined that there were more revision hip arthroscopies in the partial repair group (13%, 4/32) compared to the complete closure group (0%, 0/32), although it not stated whether the difference is statistically significant. There were statistically and clinically relevant differences in early outcomes (6 months and 1 year), with the complete closure group having superior hip outcome score sports specific subscale (HOS-SS) scores; however, no differences were observed in the modified Harris Hip Score (mHHS) or the hip outcome score activities of daily living subscale (HOS-ADL) scores at final follow-up. No multivariate analysis was used to control for patient factors contributing to these differences. Domb, et al., compared the outcomes of patients with no closure of an inter-portal capsulotomy to those who had between 50-100% of their capsulotomy closed. The authors performed a multivariate analysis and determined that capsular closure did not predict the outcome of patients using the instruments measured (HOS-ADL, HOS-SSS, and non-arthritic hip scores (NAHS)). [Table 1]
Table I.
Included studies and toucomes according to capsular management
| Author | Journal | Cohort | Year | Study Design | LOE | Number of Patients (Number of Hips) | Average Age (Years) | Females | Capsule Management Comparison (Number of Patients per Group) | Difference in Outcome | p value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Domb | JHPS | Athletes | 2016 | Retrospective Case Series | 4 | 148 (158) | 30.6 (range 13-61) | 61% | Capsular repair or plication (82) vs no closure (76) | a: 54 Patients (65.85%) with repair/plications returned to sports b: 39 Patients (51.31%) without repair/plications returned to sports |
a: 0.0635 b: 0.096 |
| Larson | AJSM | Dysplasia | 2016 | Retrospective Cohort | 3 | 77 (88) | 33.9 | 71% | Capsular repair (37) vs Capsular plication (35) vs no closure (16) |
Patients with capsular plication AND labral repair had better good/excellent results* (a: 73% vs 53%), higher mHHS scores at final follow-up (b: 85 vs 77), and fewer failures (c: 18% vs 40%) when compared to all others. | a:0.06 b:0.13 c: 0.03 |
| Newman | AJSM | Revision FAI | 2016 | Prospective Cohort | 2 | 246 (246) Revisions; 492 (492) Primaries | 32.1 ± 9 | 59% | Capsular plication (106) vs no plication (140) within revision cohort |
Revision patients with increase in HOS-ADL >10 points more likely to have undergone capsular plication (75) vs no plication (31) | 0.001 |
| Amar | Arthroscopy | Primary FAI | 2015 | Retrospective Comparitive Study | 3 | 100 (100) | Capsular closure (50) vs no closure (50) |
Heterotopic ossification seen in 14/50 (28%) cases after capsular repair vs 22/50 (44%) cases without repair | 0.764 | ||
| Domb | Arthroscopy | Primary FAI | 2015 | Retrospective Case Series | 4 | 403 (403) | 36.9 | 58% | Capsular repair (168) vs no closure (235) |
After multivariate analysis, no difference was found in NAHS, HOS-ADL, HOS-SSS, and mHHS scores. | |
| Frank | AJSM | Primary FAI | 2014 | Retrospective Cohort | 3 | 64 (64) | 32.8 ± 9.9 | 63% | Partial repair (32) vs complete repair (32) of T-capsulotomy a: 13% Revision after partial repair vs 0% after complete repair. | a: 13% Revision after partial repair vs 0% after complete repair. b: HOS-SS favored complete repair @ 6, 12, and 30 months c: Finals satisfaction better after complete repair (8.6) vs partial repair (8.4) d: No difference in HOS-ADL and mHHS |
a: NA b: 0.039,0.006, <0.001 c: 0.025 d: NS |
| Larson | AJSM | Revision FAI | 2014 | Retrospective Cohort | 3 | 79 (85) Revisions; 220 (220) Primaries | 29.5 (range 16-59) | 56% | Capsular plication (23) vs repair within revision corhort (62) |
Greater increase in mHHS with capsular plication (26.4) vs repair (14.8) |
0.032 |
* Good and excellent results defined as mHHS >80
** Failure is <70 or osteotomy or THA
Borderline Hip Dysplasia
Larson, et al., evaluated the outcomes of patients with borderline hip dysplasia treated with all-arthroscopic procedures. They found that capsular repair or plication coupled with labral repair was associated with lower failure rates when compared to all other patients (18% with labral repair and capsular repair/plication versus 40% without, p=0.03). When evaluating patients treated with labral repair, there were no clinically relevant or statistically significant differences in outcomes between those who underwent capsular plication and those who did not (p=0.06 – 0.13). [Table 1]
Revision Hip Arthroscopy
Two studies18, 20 compared outcomes of revision arthroscopy according to capsular management. Newman et al., prospectively evaluated the outcomes of 179 patients undergoing revision hip arthroscopy; 106 cases underwent capsular plication and 73 did not. The HOS-ADL scores were compared pre- and post-operatively and patients who had demonstrated clinically important differences (minimal clinically important difference (MCID), >10 points) were more likely to have undergone plication of the capsule compared to those who did not (69% versus 44%, p=0.001).20 Larson et al.,18 evaluated the outcomes of patients undergoing revision hip arthroscopy and determined that capsular repair or plication was associated with greater changes in the mHSS preoperative to final follow-up when compared to no closure (14.8 vs 26.4; p=0.032). This difference in scores was both statistically significant and met minimum clinically important differences for the outcome measure. [Table 1]
Return to Sport/ Sport-specific PRO
Two studies12, 17 evaluated sports participation after hip arthroscopy by comparing capsular management. Domb et al., evaluated patients who were able to return to sport and those who were not. They reported 54/82 (65.85%) patients were able to return to sport after hip arthroscopy with capsular repair/plication compared to 39/76 (51.31%) who were not repaired.17 This difference was not found to be statistically significant. Meanwhile, Frank et al., evaluated sports participation using the HOS-SS,12 which determines the amount of difficulty patients have running one mile, jumping, landing, cutting and performing other sports-related tasks. When comparing partial repair of a T-capsulotomy (inter-portal capsulotomy equivalent) to complete repair, the complete repair group demonstrated a statistically significant increase in HOS-SS scores compared to the partial repair group. These differences were clinically relevant and statistically significant at 6 month and 1 year time points. At 2.5 years, however, differences in the HOS-SS scores between the complete and partial repair groups did not meet the minimum clinically important difference (MCID) for the outcome instrument (9 points)21. [Table 1]
Heterotopic Ossification
One study evaluated the development of heterotopic ossification as an outcome comparing capsular repair to no repair.16 Amar et al., determined that the rate of heterotopic ossification without capsulotomy closure was 44% compared to 28% after routine capsular closure, though this difference was not statistically significant (p=0.764). [Table 1]
Quality Appraisal
Overall, the quality of studies comparing outcomes by capsular management were deemed to be low by MCMS scoring. The MCMS is graded on a scale of 0-90 with 90 representing studies of the highest quality. Overall, the quality of studies comparing outcomes by capsular management were deemed to be low by MCMS scoring (range 36-59, mean 45.6). There were no differences in MCMS scores for revision hip arthroscopy (50) compared to primary hip arthroscopy (48) return to sport (39), borderline dysplasia (48) and heterotopic ossification (36), p=0.84. Of the studies included, the level of evidence was graded ‘2’ in one study, 4 studies were given a level 3 grade and two were graded level 4.
Discussion
Despite the increasing popularity of routine capsular closure in hip arthroscopy1, 2, there are limited applications supported by high level evidence in the present literature. The strongest available literature in the field (Level 2 and 3 evidence) supports capsular repair or plication in a revision hip arthroscopy setting. Clinically important differences in patient outcomes are not seen with complete closure after primary hip arthroscopic treatment of FAI at final follow up. Capsular repair may help patients after primary arthroscopy for FAI for surgeons who use a T capsulotomy, but no such differences are seen after inter-portal-only access. This review suggests capsular repair may aid in early return-to-sport for athletes but further studies are needed to prove or refute this hypothesis. Capsular closure does not appear to prevent the development of HO. Several of the findings in this literature review warrant further discussion.
Primary hip arthroscopy
The present literature is inconsistent regarding the influence of capsular closure on outcomes after primary hip arthroscopy. Domb et al11 evaluated the influence of capsular repair on outcomes after primary hip arthroscopy. Cases that were left unrepaired were older (42.3 vs 29.4; p<0.001) had higher BMIs (26.8 vs 22.9; p<0.001) and were more commonly male (p<0.001). Prior to surgery, they had more chondral damage (p<0.0081) and lower baseline patient reported outcomes. When univariate analysis was performed, it appeared that hip capsular repair yielded greater HOS-ADL and NAHS scores compared to those left unrepaired. Importantly, the study was adequately powered for a multivariate analysis in order to account for these potential confounders, and when proper statistical models were applied, capsular repair did not change any outcome. Frank, et al., retrospectively evaluated differences in outcomes after partial and complete closure of a T-capsulotomy after primary hip arthroscopy for FAI. They found no clinically important differences in HOS-ADL or mHHS; however, patients who underwent complete repair had improved early HOS-SS scores after surgery.12 It should be recognized that T-capsulotomies12 are much more extensile (extending to or through the zona orbicularis) than inter-portal11 capsulotomies. There may be a role for complete capsular closure for extensile capsulotomies in the primary setting in active patients, however further prospective studies are needed.
Return to Sport
When an athlete sustains a hip injury such as a labral tear and continues to stress the joint with both axial and rotational forces, the hip capsule is thought to be subjected to more tensile loading22, 23 once the suctionseal is lost due to a lesion in the acetabulum24. Athletes, therefore, should be examined for micro instability at the time of arthroscopy. Early return to sport may be improved with complete closure of the capsulotomy in athletes. It appeared that more athletes were able to return in a retrospective review by Domb et al17, however the study was not powered to detect a significant difference. In the report by Frank et al12, the sportsspecific subscale of the HOS was significantly better and met MCID for the first 6-12 months after surgery for those that underwent complete repair as opposed to partial repair, suggesting earlier return to activities. It has been suggested that hip injuries and labral tears in athletes can lead to focal instability with elongation of the iliofemoral ligament; this may be most pronounced in hip injuries with participation in football, golf, baseball, gymnastics and martial arts.23 With repetitive loading and rotational stress, injuries can occur including labral tears and iliofemoral ligament redundancy, resulting altered joint biomechanics.22, 23 Level 3 evidence suggests complete capsular repair after hip arthroscopy is associated with earlier return to activity and capsular closure should be considered in athletic populations with FAI and labral pathology.
Revision Hip Arthroscopy
The highest level evidence (Level 2 and 3) supports capsular repair or plication in a revision hip arthroscopy setting18, 20. Larson et al compared a cohort of revision patients to those undergoing primary hip arthroscopy for FAI. They determined that capsular plication in a revision setting was associated with a pre- to post-operative difference in the mHHS of 26.4 points, which was significantly greater than the 14.8 point difference seen without plication.18 In their prospective study, Newman et al, found that capsular plication was more likely to meet MCID in HOS-ADL scores compared to no plication and this this difference was statistically significant (p=0.001).20 Furthermore, repair in a primary setting has been suggested to be associated with lower rates of revision surgery12, 19.
It should be recognized that inherent bias is present in retrospective studies with revision surgery as an outcome. While ACL graft failure or an infected joint arthroplasty are indications for re-operation in many settings, surgeons who are treating patients with persistent pain after hip arthroscopy with an un-closed capsulotomy may have a lower threshold to recommend revision in part to close their capsulotomy despite a clear association between their symptoms and previous treatment. Patients undergoing revision arthroscopic surgery of the hip do so for a wide array of indications. It has been demonstrated that patients with micro-instability after primary hip arthroscopy do improve with revision and capsular plication.25 The current literature suggests surgeons should have a low threshold for repairing or plicating the hip capsule in a revision setting most importantly if there is a concern for micro-instability contributing to symptomatology.
Heterotopic Ossification
Heterotopic ossification is a known complication of hip arthroscopy with an incidence between 5-36%16, 26. Heterotopic ossification is more commonly seen postoperatively in males when a large osteoplasty is performed.26 Furthermore, there is some retrospective evidence that suggests postoperative indomethacin is associated with decreased rates of heterotopic ossification. In a study by Bedi et al, the rate of HO was 1.8% when indomethacin was administered after surgery compared to 8.3% in the absence of prophylaxis. The rate of heterotopic ossification was found to be much higher in the study identified in our review.16 Capsular closure did not alter rates of heterotopic ossification following arthroscopic surgery for FAI.
Limitations
This review does have some limitations. First, comparative groups were not uniform across the identified studies that met inclusion criteria; they included partial versus complete closure of different types of capsulotomies and plication versus no closure. Further, capsular repair and plication were not always clearly defined and occasionally used interchangeably. Outcomes were not uniform or granularly reported; these shortcomings in the present literature prevented a quantitative meta-analysis as the data could not be pooled cleanly. The majority of studies evaluated comprised of level 3 evidence and multivariate analysis controlling for important patient factors was rarely utilized in this body of literature. Finally, several studies reported outcomes with small sample sizes and reported “no difference” in their selected outcome after capsular closure. These small studies, without the use of an a priori power analysis, may potentially be under-powered and subject to type two (beta) error.
Conclusions
The strongest available evidence in the present literature suggest capsular plication at the time of revision hip arthroscopy has meaningful impacts on patient outcomes after surgery. There is insufficient evidence in the present literature to indicate routine closure of inter-portal capsulotomies in a primary hip arthroscopy setting, however this may be a consideration if extensile capsulotomies are created. Athletes who present with an element of micro-instability may have better return to sport rates with capsular closure or plication, however further studies are warranted. Capsular management does not appear to impact rates of heterotopic ossification. Further prospective studies are indicated to elucidate the impact of capsular management on patient reported outcomes after hip arthroscopy.
References
- 1.Gupta A, Suarez-Ahedo C, Redmond JM, et al. Best Practices During Hip Arthroscopy: Aggregate Recommendations of High-Volume Surgeons. Arthroscopy. 31:1722–1727. doi: 10.1016/j.arthro.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 2.Matsuda DK. Editorial Commentary: Hip Capsule: To Repair or Not? Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2017;33:116–117. doi: 10.1016/j.arthro.2016.10.023. [DOI] [PubMed] [Google Scholar]
- 3.Clohisy JC, Nepple JJ, Larson CM, Zaltz I, Millis M. Members ANoCHOR. Persistent structural disease is the most common cause of repeat hip preservation surgery. Clinical Orthopaedics and Related Research®. 2013;471:3788–3794. doi: 10.1007/s11999-013-3218-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ross JR, Larson CM, Adeoyo O, Kelly BT, Bedi A. Residual Deformity Is the Most Common Reason for Revision Hip Arthroscopy: A Three-dimensional CT Study. Clinical Orthopaedics and Related Research®. 2015;473:1388–1395. doi: 10.1007/s11999-014-4069-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2007;23:1295–1302. doi: 10.1016/j.arthro.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 6.Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39 doi: 10.1177/0363546511412161. Suppl:85s-91s. [DOI] [PubMed] [Google Scholar]
- 7.Telleria JJM, Lindsey DP, Giori NJ, Safran MR. An Anatomic Arthroscopic Description of the Hip Capsular Ligaments for the Hip Arthroscopist. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2011;27:628–636. doi: 10.1016/j.arthro.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Abrams GD, Hart MA, Takami K, et al. Biomechanical Evaluation of Capsulotomy, Capsulectomy, and Capsular Repair on Hip Rotation. Arthroscopy. 2015;31:1511–1517. doi: 10.1016/j.arthro.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 9.Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, Kelly B. The function of the hip capsular ligaments: a quantitative report. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2008;24:188–195. doi: 10.1016/j.arthro.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 10.Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011;27:1379–1388. doi: 10.1016/j.arthro.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Domb BG, Stake CE, Finley ZJ, Chen T, Giordano BD. Influence of Capsular Repair Versus Unrepaired Capsulotomy on 2-Year Clinical Outcomes After Arthroscopic Hip Preservation Surgery. Arthroscopy. 31:643–650. doi: 10.1016/j.arthro.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved Outcomes After Hip Arthroscopic Surgery in Patients Undergoing T-Capsulotomy With Complete Repair Versus Partial Repair for Femoroacetabular Impingement A Comparative Matched-Pair Analysis. The American journal of sports medicine. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4(9.) doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman D, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statements. BMJ. 2009;339(5) [PMC free article] [PubMed] [Google Scholar]
- 15.Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury a systematic review. The American journal of sports medicine. 2009;37:1434–1443. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 16.Amar E, Warschawski Y, Sampson TG, Atoun E, Steinberg EL, Rath E. Capsular closure does not affect development of heterotopic ossification after hip arthroscopy. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2015;31:225–230. doi: 10.1016/j.arthro.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 17.Domb BG, Dunne KF, Martin TJ, et al. Patient reported outcomes for patients who returned to sport compared with those who did not after hip arthroscopy: minimum 2-year follow-up. Journal of Hip Preservation Surgery. 2016;3:124–131. doi: 10.1093/jhps/hnv078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larson CM, Giveans MR, Samuelson KM, Stone RM, Bedi A. Arthroscopic Hip Revision Surgery for Residual Femoroacetabular Impingement (FAI) Surgical Outcomes Compared With a Matched Cohort After Primary Arthroscopic FAI Correction. The American journal of sports medicine. 2014;42:1785–1790. doi: 10.1177/0363546514534181. [DOI] [PubMed] [Google Scholar]
- 19.Larson CM, Ross JR, Stone RM, et al. Arthroscopic Management of Dysplastic Hip Deformities: Predictors of Success and Failures With Comparison to an Arthroscopic FAI Cohort. Am J Sports Med. 2016;44:447–453. doi: 10.1177/0363546515613068. [DOI] [PubMed] [Google Scholar]
- 20.Newman JT, Briggs KK, McNamara SC, Philippon MJ. Revision Hip Arthroscopy A Matched-Cohort Study Comparing Revision to Primary Arthroscopy Patients. The American Journal of Sports Medicine. 2016 doi: 10.1177/0363546516650888. 0363546516650888. [DOI] [PubMed] [Google Scholar]
- 21.Martin RL, Philippon MJ. Evidence of Reliability and Responsiveness for the Hip Outcome Score. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2008;24:676–682. doi: 10.1016/j.arthro.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 22.Shindle MK, Ranawat AS, Kelly BT. Diagnosis and Management of Traumatic and Atraumatic Hip Instability in the Athletic Patient. Clinics in Sports Medicine. 2006;25:309–326. doi: 10.1016/j.csm.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 23.Philippon MJ, Schenker ML. Athletic hip injuries and capsular laxity. Operative Techniques in Orthopaedics. 2005;15:261–266. [Google Scholar]
- 24.Ferguson S, Bryant J, Ganz R, Ito K. The acetabular labrum seal: a poroelastic finite element model. Clinical Biomechanics. 2000;15:463–468. doi: 10.1016/s0268-0033(99)00099-6. [DOI] [PubMed] [Google Scholar]
- 25.Wylie JD, Beckmann JT, Maak TG, Aoki SK. Arthroscopic Capsular Repair for Symptomatic Hip Instability After Previous Hip Arthroscopic Surgery. The American Journal of Sports Medicine. 2016;44:39–45. doi: 10.1177/0363546515608162. [DOI] [PubMed] [Google Scholar]
- 26.Bedi A, Zbeda RM, Bueno VF, Downie B, Dolan M, Kelly BT. The incidence of heterotopic ossification after hip arthroscopy. The American journal of sports medicine. 2012;40:854–863. doi: 10.1177/0363546511434285. [DOI] [PubMed] [Google Scholar]


