Figure 1.
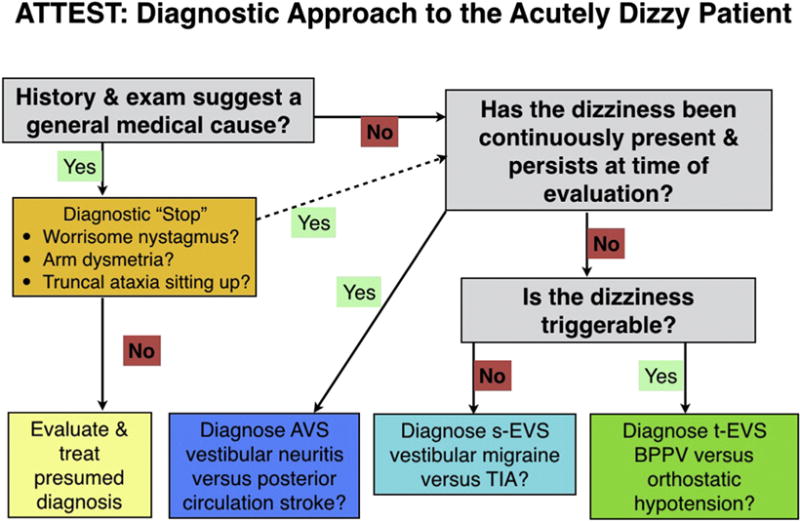
Diagnostic approach to the acutely dizzy patient. ATTEST = A, associated symptoms; TT, timing and triggers; ES, examination signs; and T, additional testing as needed. The first step is to take a history focused on associated symptoms, timing and triggers of the dizziness, and the overall context. Many patients’ histories will suggest a general medical cause (various toxic, metabolic, infectious, or cardiovascular causes). In this group of patients, we recommend a very brief diagnostic “stop” in order to reduce misdiagnosis. As part of this stop, first make sure there are no suspicious neurovestibular signs (nystagmus, limb ataxia, or gait/truncal ataxia). If a general medical cause still seems likely, evaluate and treat for the presumed diagnosis or diagnoses. For patients with a positive stop or whose history does not suggest a general medical cause, ask questions aimed at timing and triggers to place the patient into one of three categories. For patients in the acute vestibular syndrome (AVS) and triggered, episodic vestibular syndrome (t-EVS), physical examination (see text) will often allow a specific diagnosis to be made. For patients with the spontaneous episodic vestibular syndrome (s-EVS), use history to try to distinguish vestibular migraine from transient ischemic attack (TIA) or other causes (see text) since, by definition, these patients will no longer have symptoms and their dizziness cannot be triggered at the bedside. BPPV = benign paroxysmal positional vertigo.
