Abstract
Background
Technologic advances, free open‐access medical education (FOAM or #FOAMed), and social media have increased access to clinician‐oriented medical education resources and interactions at the point of care (POC); yet, how, when, and why medical providers use these resources remains unclear. To facilitate the development and design of intuitive POC resources, it is imperative that we expand our understanding of physician knowledge‐seeking behavior at the POC.
Methods
Individual semistructured interviews were conducted and analyzed using a qualitative, grounded theory approach. Twelve emergency medicine providers (three medical students, three residents, and six attending physicians) were interviewed in person or via video chat to explore how POC resources are used in the emergency department (ED). A coding system was developed by two investigators and merged by consensus. A third investigator audited the analysis.
Results
A conceptual framework emerged from the data describing the four main uses of POC resources (deep‐dive, advanced clinical decision making, teaching patients, and teaching learners) and how practitioners’ main use varied based on medical expertise. Junior learners prioritize their own broad learning. Experienced learners and physicians prefer to 1) seek answers to specific focused clinical questions and 2) disseminate POC information to teach patients and learners, allowing them to devote more of their time to other clinical and teaching tasks.
Conclusion
The conceptual framework describes how physician knowledge‐seeking behavior using POC resources in the ED evolves predictably throughout training and practice. Knowledge of this evolution can be used to enhance POC resource design and guide bedside teaching strategies.
Technology has become an essential and ubiquitous component of modern medicine.1 Physicians and medical trainees rely heavily on technology such as desktop computers, smart phones, handheld tablets, and laptops for day‐to‐day information needs.2 In addition to being a repository for various references, these devices allow constant connection to the Internet via e‐mail, text messaging, video conferencing, and social networking software that can be used for rapid knowledge exchange.3 Finally, there has also been a rapid and unprecedented expansion of online resources such as blogs, websites, and podcasts used for curation, synthesis, and translation of medical knowledge.4, 5
Physician knowledge‐seeking behavior, specifically the formulation of appropriate questions, literature searching, and resource utilization is an important aspect of appropriate clinical care that has been broadly studied within the health informatics and library literature.6, 7 Unfortunately this literature focuses on the use of time‐consuming, extensive literature review using traditional bibliographic databases such as MEDLINE and fails to address physician knowledge‐seeking behavior directly at the point of care (POC). POC resources is defined as any reference material used in the provision of medical care directly at the bedside and may include clinical problem‐solving, patient care, patient education, or learner education. Limited survey data indicate that medical learners and faculty are regularly using mobile POC resources, but a greater understanding of this phenomenon is needed in light of the increasing availability of technology and these resources.8, 9, 10
Although healthcare providers generate a substantial number of clinical questions while caring for their patients, there is poor understanding of physician knowledge‐seeking behavior at the bedside. The availability and access to clinician‐oriented medical education resources have increased dramatically due to technologic advances, the recent popularity of the free open‐access medical education (FOAM and #FOAMed) movement, and the use of social media to exchange user‐generated content.4, 11 However, we do not know how, when, or why medical providers use these resources in the clinical setting.
The purpose of this study was to explore physician knowledge‐seeking behavior to facilitate education, integration, and rational design of POC resources for direct patient care. Specifically we examined usage patterns and clinical contexts wherein emergency medicine (EM) physicians and learners interact with these resources.
Methods
Design
We used a qualitative, grounded theory approach to our study. Grounded theory involves inductively generating a conceptual framework or theory making it well suited for initial exploration of relatively underresearched areas. We used the approach of Glaser,12 focusing on the emergence of concepts and categories from a process of constant comparison of the data without fixed preconceptions. We conducted semistructured individual interviews instead of focus groups because we wanted to explore decisions and compare differences and similarities among reference group members. All attempts were made to adhere to the Standards for Reporting Qualitative Research (SRQR) guidelines.13
Interview Development
We developed a standardized interview guide based on our research questions and an initial literature search (Data Supplement S1, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1002/aet2.10101/full). During the interviews, we used both scripted and unscripted follow‐up questions to further explore and ensure clarity around new ideas and adapt the discussion as themes began to emerge. Questions within the interview guide probed information about POC resources, specifically involving participants’ current usage patterns, barriers to use, and perceived needs. These questions were felt to facilitate our understanding of physician knowledge‐seeking behavior in a number of ways, which included 1) providing insight into the current practice of early adopters of this technology, 2) identifying barriers to more widespread adoption, and 3) identifying enablers that would enhance adoption and inform future design of POC resources.
Participants and Procedure
One investigator (CP) conducted interviews on an intentional sampling of medical students; junior and senior EM residents; and early‐ (<5 years), mid‐ (5–10 years), and late‐career (>10 years) EM attending physicians between January and June 2016. This intentional sampling allowed us to compare users at different stages of training and practice. A total of 12 interviews were conducted, and no participants withdrew from the study. The study was advertised via a blog post (https://www.aliem.com/2015/07/poll-use-pv-cards/) on the Academic Life in Emergency Medicine (ALiEM) medical education website where potential participants indicated their interest in being contacted for the study. Interested participants were invited via e‐mail; they were all from North America. Interviewed participants were asked to recommend other potential participants, who were subsequently invited. There were no exclusion criteria. Interviews were intended to be 15 to 35 minutes in length and were conducted virtually via an Internet‐based video/audio conference system (except for four interviews that were conducted in person at an EM medical education conference). No interviews were repeated. The goal of the study was revealed to participants prior to the interview. We continued data collection until theoretical sufficiency was reached. Ethical approval was obtained from the Conjoint Health Research Ethics Board, and confidentiality was guaranteed by informed verbal consent with the understanding that the data would be analyzed, aggregated, and reported anonymously.
Data Analysis
Recorded interviews were transcribed verbatim by an experienced transcriptionist, and the participants’ identities were redacted prior to analysis. Interview transcripts were not returned to participants for feedback; however, prior to final analysis, a member check was performed wherein the thematic framework from our analysis was sent to the participants of the study for comment. Analysis began as the data were being collected to facilitate exploration of newly emerging issues in subsequent interviews. Transcripts were individually coded by two authors (CP and TC) using an open‐coding approach to identify emergent ideas and concepts expressed by participants and to ensure sufficiency had been achieved. We compared separate codes, and used a consensus‐building process to generate a single list of codes. A second level of analysis consisted of continuous comparison and interpretation of the codes and their interrelationships to arrive at more comprehensive categories and themes.
Analytic Team
The primary investigator for this study (CP) is an attending EM physician and has also completed a Masters in Health Professions Education (MHPE). She was directly involved in study design, data collection, analysis, and interpretation. The second data analyst (TC) is an attending EM physician with qualitative research experience and multiple degrees in education. She participated in study design, analysis, and interpretation. JV is an attending EM physician with interest and expertise in technology design. He was involved in study design, analysis, and interpretation of the results. ML is an attending physician and professor of EM at a large academic center with experience in online education and POC content development. She participated in the study design and interpretation.
We acknowledge a preexisting interest in POC resources and their use in the ED. The team was tasked with elaborating an existing POC resource for EM providers (https://aliemcards.com/) and this study was a part of the project's needs assessment. We considered our foreknowledge of POC resources to be a platform on which we designed the project and its anticipated boundaries. This theoretical scaffolding was subsequently challenged and refined as the research progressed.
Results
Interviews were conducted with 12 participants (three medical students, three residents, and six attending physicians) after which we reached sufficiency. Participants were of various training levels from EDs across Canada and the United States. All participants reported regular use of POC resources while working or learning in the ED. All medical students were in their final 2 years of medical school and had at least 8 weeks of EM clerkship/elective experience. Residents were in their second to final year of training. Attending physicians all practiced EM in the academic or community setting. Many attending physicians had education roles within undergraduate medical education (UME) or graduate medical education (GME). The demographics of the interviewees are described in Table 1. We identified three major themes describing POC resource skill development among EM learners and practitioners. Table 2 summarizes these three themes, their subthemes, and sample quotes from each.
Table 1.
Characteristics of Participants (n = 12)
| Demographic | Characteristic | Number of Participants |
|---|---|---|
| Sex | Male | 8 (67%) |
| Female | 4 (33%) | |
| Training level | Medical student | 3 (25%) |
| Resident | 3 (25%) | |
| Attending physician | 6 (50%) | |
| Average number of years in training/practice | Medical student | 2.7 (range = 2–4) |
| Resident | 2.6 (range = 2–3) | |
| Attending physician | 9.7 (range = 3–26) | |
| Country of training/practice | Canada | 6 (50%) |
| United States | 6 (50%) |
Table 2.
Exemplar Interviewee Quotes for the Three Main Themes and Their Subthemes About POC Resources
| Theme | Subtheme | Quote |
|---|---|---|
| Main uses of POC resources | Learning within the clinical environment | “I definitely use them before and after seeing the patient and before reviewing.” (S‐3) |
| Advanced clinical decision making | “Pedi‐Stat dosages and looking up, it's mostly for resuscitations. So dosages for seizures, tubes size, how deep the tube is supposed to go, what size blade I am supposed to use. Pretty much all of the things that go away once a kid is sick in front of you and you can't really think and you just like to confirm.” (R‐3) | |
| Teaching/ communicating with patients | “[T]hat's something that can keep the patient more involved in their care … if the patient sees you checking to see if a drug is safe with breastfeeding before you pick it and are actually looking there, it probably increases the patient's confidence in you and they like that.” (AP‐5) | |
| Teaching learners | “… it is a really nice tool for teaching, for saying hey why don't you go… lookup this PV card [a particular POC resources] and you know that it's a good one … you get your learner to look it up “ (AP‐1) | |
| Variation of use with medical expertise | Focus of information | “… the information often revolves around very focused clinical questions.” (AP‐2) |
| Distributing rather than consuming information | “… and they come back in five minutes … and they are briefed up on the topic, like way faster probably than you would ever be able to do it. So I think that is a really great use of them. It really, really bracket[s] learning.” | |
| Habit of use | N/A | “I use [POC resources] primarily for data that I know. I know where to find it.” (R‐3) |
Participants are identified as student (S), resident (R) or attending physician (AP).
POC = point‐of‐care.
Theme 1: Main Uses of POC Resources
Learning Within the Clinical Environment
POC resources are used to facilitate the broader comprehension of a subject area (“deep‐dive”). This includes a review of general concepts relating to a clinical presentation, key areas of patient care, and alternative diagnoses.
Although participants were specifically asked to focus on their POC resource use in the clinical setting, many (in particular medical students and junior residents) mentioned regularly using POC resources to address knowledge gaps identified outside of dedicated study times (lying in bed awake at night, on their commute, immediately before or after a shift) especially at times when it is not possible or is inconvenient to access a more extensive resource such as a journal article or textbook.
Advanced Clinical Decision Making
Participants also used POC resources to address individual patient‐ and context‐specific questions related to management and disposition. This most frequently involved quick referencing of easily forgotten details such as a number, percentage, diagnosis, or a previously learned fact. Other specific tasks included checking medication dosages, performing calculations, and applying clinical decision instruments.
Teaching/Communicating With Patients
Practitioners bring POC resources directly to the bedside to effectively teach and communicate with patients. They are able to address questions directly at the bedside by either showing information on their screens or referring patients to a specific high‐quality resources. Examples include the use of a medical sketching application to show patients the anatomical location of pathology, addressing real‐time questions about medication side effects or contraindications, and printing previously vetted discharge instructions for the patient.
Teaching Learners
Educators use POC resources in many different ways to teach learners. Sometimes they point learners to previously vetted resources, while at other times they promote independence and problem‐solving skills by instructing them to embark on a scavenger hunt to find the answer to their questions independently. These resources also allow for more tailored teaching for specifically identified learner needs. For example, if a medical student identifies electrocardiogram (ECG) interpretation as a learning priority, instead of seeking out a patient with a particular ECG abnormality, they can access high‐quality normal and abnormal examples quickly and efficiently.
Theme 2: Variation in POC Resource Use With Expertise
Medical students use POC resources to deep‐dive around almost every patient encounter. They tend to focus on general concepts such as “chest pain” or “pediatric fever” with the goal of expanding their knowledge about a given clinical presentation or diagnosis. Early in their clerkship experiences, worried that they might miss key questions to ask patients, they often access POC resources to review the chief complaint immediately prior to seeing a patient. As they gain more experience, they progress to preferentially accessing POC resources following a patient encounter and prior to reviewing the case with their supervisor.
In contrast, residents feel that the busy clinical environment precludes the opportunity to read about a general topic and prefer to focus on key areas that help them advance patient care, addressing issues such as “management/disposition of chest pain” or “management of pediatric fever.” For example, a resident assessing an infant with fever may use POC resources to apply clinical decision rules regarding the need for further testing and then access their local online antibiogram to inform their decision regarding empiric antibiotic therapy. Attending physicians rarely use POC resources for deep‐dives. Occasionally when faced with an uncommon clinical entity or atypical presentation, they may access POC resources to broaden their differential and identify alternative diagnoses. They also describe sporadic reading of these resources while off shift to refresh their knowledge of a particular topic.
Both senior residents and attending physicians most frequently use POC resources for advanced clinical decision making (checking medication dosages, performing calculations, and applying clinical decision instruments). They consider this an important safety check and feel it is particularly useful in uncommon events with high cognitive or emotional load. Pediatric resuscitation is a frequently cited example of such an event where practitioners are looking up details such as weight‐based drug dosages, endotracheal tube (ETT) size, ETT depth of insertion, and laryngoscope blade size. Additionally, those who have POC resources integrated into their institutional workflow, such as customized order sets or apps, use them for both common and uncommon presentations. They feel that using these integrated POC resources facilitates standardized practice. They also perceive that it improves communication with other allied health professionals such as nurses who, for example, may be more likely to question deviations in investigations, drug choices, or dosing.
Senior residents and attending physicians bring POC resources to the bedside, regularly using them in their communication with and education of patients. This behavior is not described by medical students and junior residents who described feeling uncomfortable and awkward engaging with their phones in front of attending physicians and patients.
POC resource use is also highly valued by senior residents and attending physicians in teaching learners. Specifically, participants appreciate the ability to offload the teaching of basic principles, while reserving face‐to‐face time to clarify more advanced concepts and address questions.
Theme 3: Habit of Use
The most powerful driver for POC resource selection is habit of use. The more familiar or more frequently a resource is accessed, the more likely it is to be accessed again. Accessibility, searchability, and usability are important drivers of use; however, once a user has established habit of use, inconveniences such as number of clicks/taps or lack of an independent platform are no longer perceived as barriers and can be overlooked. Habitual users were directly asked about the perceived inconvenience of extra clicks (specifically identified by novel users a significant barriers to use) and are largely unaware and not bothered about expending this extra effort to access information on a familiar POC resource.
With regard to POC resource selection, medical students and junior residents tend to explore a wide range of resources. They are more likely to access those geared toward primary care, rather than specialty‐specific resources. The importance of habit of use is already present among junior residents who describe being less likely to access a resource (even if it is available on their device) if it is not something they use often or have a lot of experience using. Despite having innumerable resources available on their device, even at their early stage of learning, junior residents appear to have an established “workflow,” which includes a few key resources that they access frequently.
Senior residents and attending physicians are more heterogeneous with regard to resource variety and usage. Those who used POC resources throughout their training have a greater variety of resources compared to mid‐ or late‐career clinicians who incorporated POC resources while already in practice. In general, senior residents and attending physicians access specialty‐specific, succinct, and easy‐to‐use resources. Personalized, customizable, or personally developed references are particularly valued and desired. Attending physicians who developed their own notes throughout their training and practice access these in lieu of external resources while others rely heavily on institutional resources that highlight institution‐specific protocols or recommendations. One commonly stated reason for not exploring a new POC resource is the lack of motivation or desire to do things differently. Overall, time, reliability, and familiarity are important considerations in choosing which POC resource to access.
Discussion
Point‐of‐care resources are increasingly available to health care providers and have the potential to impact decision making, patient care, teaching, and learning within the clinical environment. Despite the ubiquity and accessibility of these resources, little is understood about physician knowledge‐seeking behavior at the bedside. Such an understanding will greatly facilitate the design of POC resources and development of strategies to instruct trainees and providers on how best to incorporate these technologies into their workflow.
Proposed Conceptual Framework
To encourage further work and understanding of physician knowledge‐seeking behavior in using POC resources, we propose the following conceptual framework (Figure 1). The framework highlights the four main uses of POC resources (deep‐dive, advanced clinical decision making, teaching patients, and teaching learners) and dichotomizes knowledge‐seeking behavior into “knowledge for self,” that is knowledge that the provider is seeking for his/her own direct consumption versus knowledge for others which refers to knowledge that is sought with the specific intent of sharing it with others. The type of knowledge chosen largely depends on how much time a provider has, with knowledge for self requiring a greater time commitment versus “knowledge for others offering the possibility of time savings. Finally, our conceptual framework highlights the fact that POC resource usage patterns evolve predictably with clinical expertise.
Figure 1.
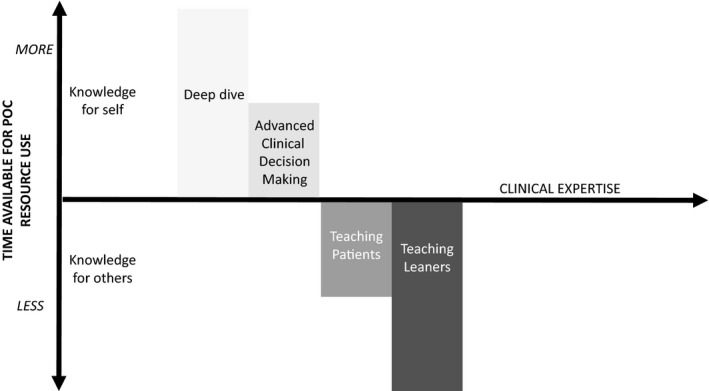
A proposed conceptual framework for POC resource use in the ED. POC = point of care.
The framework clarifies several of our key findings. Less experienced providers, such as medical students and junior residents, use POC resources almost exclusively for knowledge for self. They devote a considerable amount of time to broaden their knowledge and “dive deep” into general topics. Experienced providers prefer to engage in small bursts of knowledge‐seeking focused on cueing recall of important details, performing calculations, applying clinical decision instruments, or addressing patient‐ and context‐specific clinical questions aimed almost exclusively at advancing patient management. Furthermore, experts greatly value time‐saving interventions and tend to focus their POC resource use on seeking knowledge for others. They direct patients and learners to high‐quality resources with standardized content and reserve face time for clarification and more nuanced questions. Access to high‐quality resources also allows them to tailor their teaching to a learner's identified needs regardless of the real cases available in the clinical environment.
By applying a qualitative lens to examine POC resource use among medical providers in the ED, our study has revealed some unique aspects of knowledge‐seeking behaviors. Our study confirms that ED providers routinely use POC resources in the clinical environment. This expectantly follows provider goals to provide current, evidence‐based patient care, often by navigating an exponentially growing amount of primary and secondary medical literature.5, 14 Advances in technology have brought these sources of literature to their fingertips on devices such as smartphones, tablets, laptop, or desktop computers. Thus, it follows that clinicians perceive a benefit from their accessibility at the bedside.1 Although other studies of EM trainees suggest considerable uptake of asynchronous education (e.g., sharing online resources and promoting peer‐to‐peer interactions), our study is the first to suggest that all levels of EM providers, regardless of expertise, take advantage of these POC resources for direct patient care.15, 16
Given the relative infancy of POC resources, educators may be called upon to promote and champion this technology for all medical providers. Educators can tailor their tips and strategies to the expertise of the learner. Junior learners may be referred to resources that allow them to broaden their knowledge. Furthermore, they can be encouraged to complete their case‐based learning cycle and information retrieval at the POC, as this may improve their experiential learning.17 More advanced trainees and clinicians could be encouraged to take some time outside of the clinical environment to explore relevant, succinct resources prior to using them while on shift. To accelerate POC resource adoption, the time‐saving benefits of off‐loading learner and patient education tasks can be highlighted. Time saved can be better spent answering clarification or nuanced questions. Overall, appropriate POC resource use should be encouraged among all providers. Attempts should be made to combat the potentially perceived stigma associated with use of digital devices. These same concepts can be used to ultimately guide POC resource design.
The emergence of new instructional strategies, digitalization of information, and accelerating pace of change has significant potential to transform medical education.18 This, however, requires educators to be aware of and prepared to use POC resources in the clinical setting. POC resources offer the prospect of not only supporting current teaching methods but also to catalyze change and enable a healthy disruption in the way that medical education and ultimately health care are delivered.19
Limitations
To our knowledge, this is the first published study to present a conceptual framework and developmental model for the use of POC resources in the clinical setting. Our use of a single modality of data collection (semistructured individual interviews) and single clinical setting (the ED) limit transferability and generalizability of our results. Also, the lead investigator and interviewer (CP) is an EM attending physician with a preexisting interest in POC resources, which may have resulted in inadequate metaposition (analytical distance from the subject matter). Finally this study was completed as a planned subanalysis of a larger study regarding POC resources with the explicit purpose of informing future design of an existing POC resource. Our analyses may have been affected by respondents’ answers to other questions regarding the use, enablers, and barriers of specific POC resources. Finally, as with all qualitative work, ours represents a step in theory building that, while transferrable and may resonate with others, is not meant to be broadly generalizable. Prior to generalizing our findings, more robust quantitative work will be needed to test the conceptual framework we have built.
Conclusion
We propose a novel conceptual framework to delineate our findings that physician knowledge‐seeking behavior and point‐of‐care resource utilization evolve over time with clinical experience and expertise.
Supporting information
Data Supplement S1. Guide for one‐on‐one semi‐structured interview
AEM Education and Training 2018;2:221–228
An abstract based on this manuscript was presented at The Royal College of Physicians and Surgeons of Canada International Conference on Medical Education, Quebec City, Quebec, Canada, Oct 2017.
The work in this paper was supported by a grant from AgileMD.
CP and JV report receiving grant money to conduct work related to this project from AgileMD. TC reports grant money and honoraria from McMaster University, the PSI foundation, and the Academic Life in Emergency Medicine (ALiEM) Faculty Incubator program for work that is related to this present work and other medical education. ML is the founder/owner of a start‐up company (ALiEM) with an interest for the subject matter.
Author contributions: CP, TC, JV, and ML engaged in study concept and design; CP led the acquisition of the data; CP, TC, JV, and ML all conducted the analysis and interpretation of the data; CP, TC, JV, and ML all drafted of the manuscript; CP, TC, JV, and ML were all responsible for critical revision(s) of the manuscript for important intellectual content; TC provided methodologic expertise; and ML assisted with acquisition of funding.
References
- 1. Boulos MN, Wheeler S, Tavares C, Jones R. How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed Eng Online 2011;10:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Twiss‐Brooks AB, Andrade R Jr, Bass MB, Kern B, Peterson J, Werner DA. A day in the life of third‐year medical students: using an ethnographic method to understand information seeking and use. J Med Libr Assoc 2017;105:12–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Choo EK, Garro AC, Ranney ML, Meisel ZF, Morrow Guthrie K. Qualitative research in emergency care part I: Research principles and common applications. Acad Emerg Med 2015;22:1096–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nickson CP, Cadogan MD. Free Open Access Medical education (FOAM) for the emergency physician. Emerg Med Australas 2014;26:76–83. [DOI] [PubMed] [Google Scholar]
- 5. Cadogan M, Thoma B, Chan TM, Lin M. Free Open Access Meducation (FOAM): the rise of emergency medicine and critical care blogs and podcasts (2002‐2013). Emerg Med J 2014;31:e76–7. [DOI] [PubMed] [Google Scholar]
- 6. Dawes M, Sampson U. Knowledge management in clinical practice: a systematic review of information seeking behavior in physicians. Int J Med Inform 2003;71:9–15. [DOI] [PubMed] [Google Scholar]
- 7. Davies K. The information‐seeking behaviour of doctors: a review of the evidence. Health Info Libr J 2007;24:78–94. [DOI] [PubMed] [Google Scholar]
- 8. Boruff JT, Storie D. Mobile devices in medicine: a survey of how medical students, residents, and faculty use smartphones and other mobile devices to find information. J Med Libr Assoc 2014;102:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Duran‐Nelson A, Gladding S, Beattie J, Nixon LJ. Should we Google it? Resource use by internal medicine residents for point‐of‐care clinical decision making. Acad Med 2013;88:788–94. [DOI] [PubMed] [Google Scholar]
- 10. Edson RS, Beckman TJ, West CP, et al. A multi‐institutional survey of internal medicine residents learning habits. Med Teach 2010;32:773–5. [DOI] [PubMed] [Google Scholar]
- 11. Franko OI, Tirrell TF. Smartphone app use among medical providers in ACGME training programs. J Med Syst 2012;36:3135–9. [DOI] [PubMed] [Google Scholar]
- 12. Glaser BG. Basics of Grounded Theory Analysis: Emergence vs. Forcing. Mill Valley, CA: Sociology Press, 1992. [Google Scholar]
- 13. O'Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research. Acad Med 2014;89:1245–51. [DOI] [PubMed] [Google Scholar]
- 14. Bornmann L, Mutz R. Growth rates of modern science: a bibliometric analysis based on the number of publications and cited references. J Assoc Inform Sci Technol 2015;66:2215–22. [Google Scholar]
- 15. Mallin M, Schlein S, Doctor S, Stroud S, Dawson M, Fix M. A survey of the current utilization of asynchronous education among emergency medicine residents in the United States. Acad Med 2014;89:598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Purdy E, Thoma B, Bednarczyk J, Migneault D, Sherbino J. The use of free online educational resources by Canadian emergency medicine residents and program directors. CJEM 2015;17:101–6. [DOI] [PubMed] [Google Scholar]
- 17. Cooper AL, Elnicki DM. Resource utilisation patterns of third‐year medical students. Clin Teach 2011;8:43–7. [DOI] [PubMed] [Google Scholar]
- 18. Robin BR, McNeil SG, Cook DA, Agarwal KL, Singhal GR. Preparing for the changing role of instructional technologies in medical education. Acad Med 2011;86:435–9. [DOI] [PubMed] [Google Scholar]
- 19. Masters K, Ellaway RH, Topps D, Archibald D, Hogue RJ. Mobile technologies in medical education: AMEE Guide No. 105. Med Teach 2016;38:537–49. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Guide for one‐on‐one semi‐structured interview


