Figure. Proposed clinical algorithm for MNGIE diagnosis.
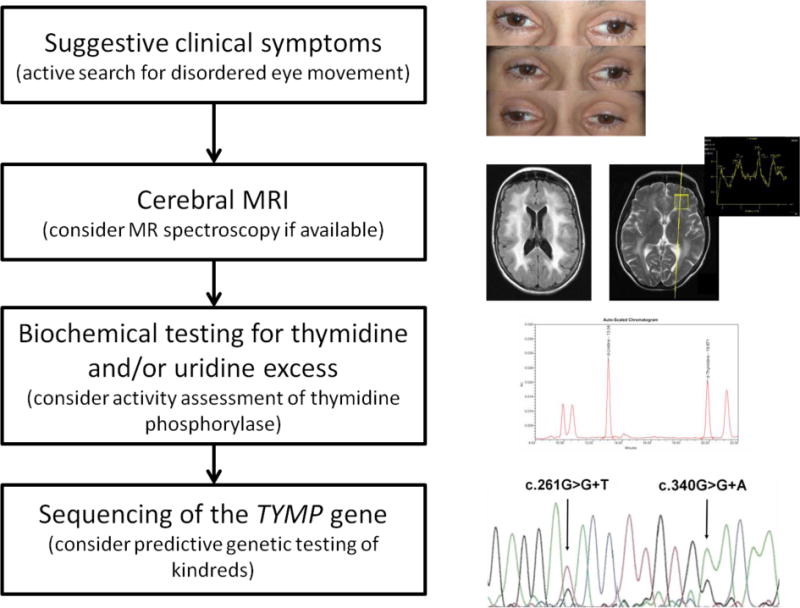
Clinical MNGIE suspicion may arise from variable signs GI dysmotility, severe cachexia, external ophthalmoparesis/ptosis, and (often subclinical) peripheral neuropathy. As a next step, radiology assessment by brain MRI to detect diffuse leukencephalopathy and, optionally, lactate peaks on MR spectroscopy. Biochemical testing for thymidine (dThd) and/or deoxyuridine (dUrd) excess in plasma and/or urine with optional assessment of thymidine phosphorylase (TP) activity. Sequencing of the thymidine phosphorylase (TYMP) gene should be performed to confirm the diagnosis and to identify presymptomatic and asymptomatic mutation carriers in kindreds. (clinical material from the patient reported in [9])
