Abstract
Objective
To estimate the cost of resources required to implement a set of Foundational Public Health Services (FPHS) as recommended by the Institute of Medicine.
Study Design
A stochastic simulation model was used to generate probability distributions of input and output costs across 11 FPHS domains. We used an implementation attainment scale to estimate costs of fully implementing FPHS.
Data Collection/Extraction Methods
We use data collected from a diverse cohort of 19 public health agencies located in three states that implemented the FPHS cost estimation methodology in their agencies during 2014–2015.
Principal Findings
The average agency incurred costs of $48 per capita implementing FPHS at their current attainment levels with a coefficient of variation (CV) of 16 percent. Achieving full FPHS implementation would require $82 per capita (CV=19 percent), indicating an estimated resource gap of $34 per capita.
Conclusions
Substantial variation in costs exists across communities in resources currently devoted to implementing FPHS, with even larger variation in resources needed for full attainment. Reducing geographic inequities in FPHS may require novel financing mechanisms and delivery models that allow health agencies to have robust roles within the health system and realize a minimum package of public health services for the nation.
Keywords: Health care financing/insurance/premiums, health promotion/prevention/screening, geographic/spatial factors/small area variations
The United States faces mounting pressure to improve population health as medical costs rise, while American health status falls further behind that of other developed nations (IOM 2013). Enactment of the Patient Protection and Affordable Care Act in 2010 ushered in a series of initiatives to expand health insurance coverage and find improved models for delivering and paying for medical care. Much less attention has focused on the nation's public health system, which is charged with preventing disease and injury in the population at large, and ensuring the safety of water, food, air, and other conditions necessary for optimal health. Of the $3 trillion spent on health and health care services in the United States in 2014, less than 3 percent supported governmental public health activities (CMS 2016). Studies consistently find the U.S. public health system to be highly variable in its capabilities across states and communities, fragmented with respect to governmental and private sector roles and responsibilities, and constrained by inadequate and unstable financing (Mays and Smith 2009; Mays et al. 2010).
A 2012 report from the Institute of Medicine identified two fundamental barriers to improving the nation's public health system: (1) lack of agreement on a core set of public health capabilities that should be present in every U.S. community and (2) lack of knowledge about the resources required to implement these capabilities (IOM 2012). The report concludes that sound policy for improving the nation's public health system can move forward only when there is sufficient understanding and agreement about what the public health system should be able to do and how much it will cost. Correspondingly, the report calls for an expert panel process to identify the components of a “minimum package” of public health services and crosscutting capabilities that should be available in every U.S. community to protect and improve population health. The report also recommended undertaking research to estimate the resources required to implement these services and capabilities universally across the United States.
In response to these Institute of Medicine recommendations, the Robert Wood Johnson Foundation commissioned an expert panel in 2013 to work on identifying components of a national “minimum package” of public health services and capabilities (PHLF 2014). Working as the Public Health Leadership Forum (PHLF), this panel included representatives from federal, state, and local public health agencies, public health professional associations, universities, public health accrediting bodies, and health policy advisory commissions. The Forum used available research, practical experience, and expert opinion to distinguish two broad types of responsibilities or “actions” within the public health system:
Type 1: Categorical programs and policies protect health and prevent disease and injury by intervening on specific risk factors and determinants of health experienced by defined population groups. These interventions are based on scientific evidence regarding efficacy and cost‐effectiveness in improving health status, and reflect evidence‐based guidelines and recommendations such as those profiled in the U.S. Centers for Disease Control and Prevention's Guide to Community Preventive Services. Examples include comprehensive smoking ban policies, tobacco cessation programs, school‐based and worksite nutrition and physical activity promotion programs, immunization campaigns for vaccine‐preventable diseases, and screening and treatment programs for sexually transmitted infections.
Type 2: Crosscutting capabilities allow the public health system to deploy its available resources in ways that optimize health and well‐being for an entire population. These capabilities allow the system to identify and track health needs and risks within a community over time, prioritize health needs and risks based on community values and preferences, engage community stakeholders in developing shared solutions to priority health needs, mobilize community partnerships and resources to implement solutions to priority health needs, and maintain measurement and evaluation processes that track progress over time and promote shared accountability for results. Examples include the capacity to lead the Emergency Support Function #8, ability to access 24/7 laboratory resources capable of providing rapid detection, developing and implementing a risk communication strategy, having organizational competencies of leadership and governance, financial management, information technology services, and the ability to strategically coordinate health equity programming.
Type 1 public health actions are the most visible elements of the public health system because they are directly experienced by target populations and by the organizations and professionals involved in implementing them. Governmental and philanthropic funding mechanisms typically focus on Type 1 public health actions due in part to the constellation of interest groups, advocates, service providers, and scientific bodies that coalesce in support of these actions and their target populations (Oliver 2006). For these same reasons, research funding historically has focused on Type 1 public health actions, resulting in a large and growing body of evidence‐based guidelines and recommendations. Nevertheless, the task of defining a “minimum package” of Type 1 public health actions for the nation is complicated by several factors. First, the volume and mix of Type 1 actions needed within a community depend heavily on demographic, socioeconomic, environmental, cultural, and epidemiological characteristics that shape health risks and needs, which vary widely across communities and change over time. Second, some Type 1 actions involve trade‐offs between individual rights, collective health benefits, and the distribution of benefits and costs within a community that is subject to community values and preferences and therefore best resolved through democratic policy making processes. Some communities may prefer less intrusive, coercive, or costly interventions even if they are less effective in improving health.
By comparison, Type 2 public health actions form the organizational infrastructure, decision support architecture, and collaborative capacity that supports the nation's public health system. These actions are more diffuse and less visible within communities. The processes used to implement Type 2 actions are fluid and frequently adapted to fit specific political, legal, social, and economic contexts of individual communities. The stakeholders involved in Type 2 actions may not always recognize their roles in these actions nor attribute them as responsibilities of the public health system. Historically, the scientific community has focused much less attention on Type 2 actions than on Type 1 actions, and as a result, it is more difficult to link Type 2 actions to defined and measurable outcomes. Recent research, however, suggests large gains in population health are achievable over time through efforts to build Type 2 activities and infrastructure (Mays, Mamaril, and Timsina 2016). Unlike Type 1 actions, the need for Type 2 actions is not conditional on the presence or magnitude of specific risk factors, community conditions, or population characteristics. Importantly, Type 2 actions can be conceptualized as first‐order activities that inform and support the downstream, second‐order decisions about the volume and mix of Type 1 activities that are needed within communities. Type 2 actions are conceptually linked with principles of procedural justice, which stress that how decisions are made are at least as important as what decisions are made in shaping the implementation and outcomes of these decisions (Tsuchiya et al. 2005).
Defining Foundational Public Health Services
The Public Health Leadership Forum developed a consensus set of Foundational Public Health Services (FPHS) delineating skills and capabilities that every state and local public health agency should have to protect and improve health status across the American population (PHLF 2014). In developing this recommended set of services, the Forum chose to focus on crosscutting Type 2 public health actions and capabilities considered to be the primary responsibility of governmental public health agencies operating at state and local levels. These Type 2 actions were considered “foundational” by the Forum because they represent first‐order activities that enable and support the array of specific programs and policies that communities use in improving health and well‐being. The Forum recognized important federal roles in supporting and funding FPHS, but it chose to focus its recommendations on public health responsibilities carried out predominately at state and local levels. The Forum developed and defined its recommended set of FPHS using an iterative process of reviewing evidence from available research studies and existing data sources, assessing the experiences of practicing public health professionals across the United States, and examining findings from state‐specific initiatives to define core public health activities. Recent state initiatives in Washington, Ohio, and Colorado were particularly informative in developing FPHS definitions, as was the set of national public health accreditation standards developed by the Public Health Accreditation Board.
Following a one‐year development and deliberation period, the Public Health Leadership Forum released its initial version of FPHS recommendations and definitions in March 2014 (PHLF 2014). The recommended set of FPHS consists of six broad and crosscutting “Foundational Capabilities” along with five “Foundational Areas” that represent more specialized domains of activity and substantive areas of expertise. Together, these 11 FPHS elements, as summarized in Figure 1, comprise a significant portion of the “minimum package” of public health services and capabilities called for by the Institute of Medicine.
Figure 1.

- Source: Public Health Leadership Forum (PHLF 2014).Notes: The 11 Foundational Public Health Service domains are grouped according to (1) Foundational Capabilities (FC) defined as crosscutting skills that need to be present in state and local health departments everywhere for the health system to work anywhere and (2) Foundational Areas (FA), which are the substantive areas of expertise or program‐specific activities in all state and local health departments essential to protect the community's health. For the purpose of this paper, when we consider the Foundational Capabilities and Areas together as a whole, we refer to them as “Foundational Public Health Services” or “FPHS”—the suite of skills, programs, and activities that must be available in state and local health departments system‐wide.
A cost estimation workgroup was also convened by PHLF to recommend a methodology for estimating the resources required to fully implement FPHS using a relatively rapid and low‐cost strategy that could generate estimates with an acceptable level of precision. This workgroup outlined a general set of principles to guide the development of a costing methodology including the use of a prospective costing approach to assess the required resources for health agencies to achieve “desired levels of capability” relative to existing levels of capability (Mays 2014). The workgroup recommended that a study be initiated to pilot‐test the methodology to further refine it, and it is this pilot‐testing phase of the FPHS cost estimation work that this paper focuses on. Specifically, we refine the cost estimation methodology by applying stochastic simulation techniques to estimate the level and variation of FPHS costs. We show how our simulation approach is a pragmatic and appropriate method for estimating FPHS costs especially when working with a small survey sample and where a high degree of uncertainty is involved.
The rest of this paper proceeds as follows. We describe the data collected and the simulation model. We then present and discuss the results, note the study's limitations, and conclude with possible future research avenues.
Methods
We estimated FPHS costs using data collected from a diverse cohort of 19 public health agencies located in three states who volunteered to implement the FPHS cost survey in their agencies during 2014–2015.1 The local public health agencies in this cohort serve a mix of rural and urban communities ranging in size from less than 25,000 residents to more than 500,000 residents. Costs are computed from the perspective of the health agency and estimates represent the annual economic value of resources utilized in each FPHS domain over a one‐year time horizon. To account for the scale of operation, we asked health agency respondents to report the population size of their respective jurisdictions. This information is used to express cost estimates on a per capita basis.
The resources required to implement FPHS are estimated using a microcosting methodology that adheres closely to approaches commonly used with public health agencies, substance abuse treatment programs, and other health and social service sectors (Mays 2014). This method uses a survey instrument administered to local health department directors and public health agency administrators to elicit information about the labor and nonlabor resources currently used by their agencies to implement activities specified in the FPHS definitions. With the exception of the implementation attainment scale, our survey instrument was adopted and modified from an early version of a data collection instrument developed by the Public Health Activities and Services Tracking (PHAST) Study team at the University of Washington (Bekemeier et al. 2017) and is comprised of six sections: (1) agency workforce composition; (2) labor resource use; (3) range of annual salaries plus fringe benefits; (4) total annual nonlabor costs; (5) administrative overhead rate; and (6) an implementation attainment scale.
Implementation Attainment Scale
To determine the expected cost of full attainment for each FPHS domain, the conventional method would be to elicit direct estimates from health agency respondents on the fraction of resource use or expected resources required to achieve the desired level of attainment as defined in PHLF (2014). The concern with this approach, however, is the possible upward bias inherent in aspirational type questions related to economic resource requirements, especially when respondents have a baseline point of reference of current cost or funding levels (i.e., more resources = increased attainment = greater cost). To minimize the potential for this type of bias, we designed a nonmonetary “implementation attainment scale” to derive the costs of full FPHS attainment. Figure 2 provides a simple conceptual representation of this approach. As the true functional form of the relationship between current and full FPHS attainment levels is unknown, we assume a linear function for our scale in deriving cost FA—the expected cost of full FPHS attainment based on knowing cost CA, where cost CA in Figure 2 represents the value of resources used at current levels of FPHS attainment, and where cost gap is the unmet resource gap or the difference between current and expected costs. To operationalize the scale, we ask the health agency administrator, based on his or her understanding of how each FPHS domain is defined in PHLF (2014), to provide an overall assessment on the following question:
Figure 2.
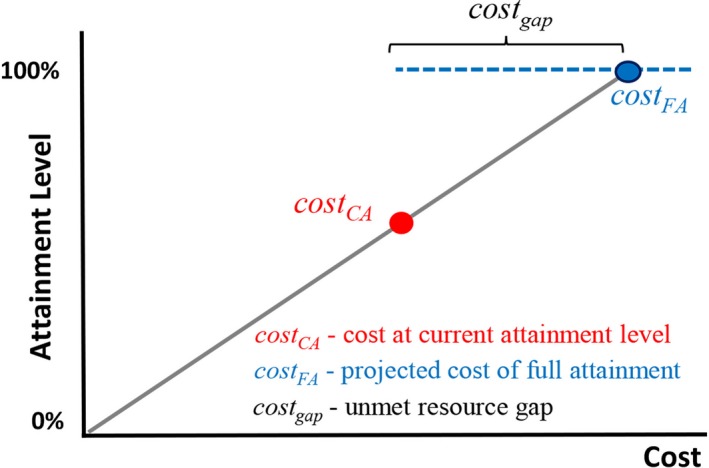
Conceptual Representation of Implementation Attainment Scale [Color figure can be viewed at http://wileyonlinelibrary.com]
For each FPHS domain, what is the estimated percentage currently being met by your health department?
We use the percent attainment value reported by the respondent and relate it to the value of their agency's existing resource level use for a given FPHS domain as measured by its corresponding cost. The current attainment value thus becomes a proxy measure of the fraction of the value of resources needed to fully implement FPHS. As illustrated in Figure 2, by assuming the value of resource level use as proportional to the percent level of FPHS attainment, we compute for expected per capita cost required to fully implement each FPHS domain by solving a percentage problem question using the simple formula:
where pct CA is the current attainment percentage value, and pct FA is equal to 100 percent. The overall average FPHS current attainment level reported from our study cohort was around 60 percent.
Analytical Strategy
Prior to filling out the survey questionnaire, respondents were requested to first read the FPHS Definitions Document from PHLF (2014), and then answer questions regarding resource use and allocation based on their understanding of each FPHS domain. Because the FPHS elements are described and defined using general terms and are not precisely specified, our cost estimation methodology accounts for the possibility of differences in interpretation and differences in implementation across state and local public health settings. Using these general definitions, public health officials are likely to face some level of uncertainty in determining the resources currently used by their agencies to implement each FPHS domain. Further contributing to the uncertainty is that existing financial and performance reporting systems in public health do not align with the FPHS framework; that is, public health agencies do not keep financial records or manage resources according to these FPHS categories. To account for these uncertainties, our data collection tool elicits from respondents both upper‐bound and lower‐bound estimates of current resource use for each FPHS and each resource category (both labor and nonlabor categories), along with estimates of the most likely resource levels used in their agency. Using these three points of support for each resource category, we use Monte Carlo simulation modeling techniques to estimate both within‐agency uncertainty and between‐agency variation in resource use, separate these two components, and then calculate the most likely levels of resource use.
The methodology produces three sets of cost estimates that serve as our primary outputs of interest: (1) costs currently incurred by an agency to implement each FPHS domain (current costs); (2) expected costs that would be incurred by the agency to implement each FPHS at full attainment levels; and (3) unmet resource gap that is calculated as the difference between expected costs and current costs for each FPHS domain. We also consider the intermediate output level, where total FPHS costs are aggregated across six domains within the Foundational Capabilities category and across five domains across the Foundational Area category. In running our simulation, labor and nonlabor costs for each of the 11 FPHS domains are treated as random input variables to account for the uncertainty associated with collected cost data. In total, we randomly sample 22 separate input cost distributions across 11 FPHS domains to simulate a distribution of total FPHS per capita costs:
We used Palisade @Risk 7.5 software to estimate 10,000 iterations of the simulation model using Latin Hypercube Sampling and assume Program Evaluation and Review Technique (PERT) distributions for all cost parameters.2
Results
The results of our simulation model are presented in Table 1. The first three columns and fifth to seventh columns in Table 1 list the mean, the 2.5th and 97.5th percentile value for per capita FPHS costs at current and at full attainment, respectively. Estimates for the mean per capita value of the resource gap, expressed as the difference between expected and current costs, are listed in the ninth column of Table 1. For all three sets of cost estimates, we also report the coefficient of variation (CV) to evaluate the distribution spread of our cost estimates.
Table 1.
Estimated Current and Expected Costs per Capita by FPHS Domain
| FPHS Domain | A. Current Resource Use ($) | B. Expected Cost of Full Attainment ($) | C. Resource Gap ($) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Percentile | Coef. Var. (%) | Mean | Percentile | Coef. Var. | Mean | Coef. Var. | |||
| 2.5th | 97.5th | 2.5th | 97.5th | |||||||
| Foundational capabilities | ||||||||||
| Assessment | 1.70 | 0.32 | 3.43 | 49 | 3.40 | 0.55 | 7.28 | 53 | 1.71 | 117 |
| Emergency Preparedness | 2.57 | 0.48 | 5.33 | 51 | 5.47 | 0.78 | 12.45 | 57 | 2.90 | 118 |
| Communication | 0.63 | 0.11 | 1.32 | 51 | 0.98 | 0.20 | 1.94 | 47 | 0.35 | 162 |
| Policy Development | 1.52 | 0.24 | 3.27 | 54 | 3.21 | 0.63 | 6.90 | 52 | 1.69 | 111 |
| Community Partnerships | 2.22 | 0.36 | 4.77 | 53 | 3.85 | 0.71 | 8.06 | 51 | 1.63 | 100 |
| Org. Competencies | 9.82 | 3.65 | 16.18 | 34 | 14.91 | 3.64 | 29.29 | 46 | 5.09 | 150 |
| Tot. Found. Capabilities | 18.46 | 11.04 | 26.27 | 22 | 31.82 | 17.20 | 48.80 | 26 | 13.36 | 68 |
| Foundational areas | ||||||||||
| Communicable Disease | 3.40 | 0.84 | 6.34 | 43 | 5.53 | 1.36 | 10.21 | 43 | 2.13 | 132 |
| Chronic Disease | 3.30 | 0.60 | 6.77 | 50 | 6.72 | 1.23 | 14.16 | 52 | 3.42 | 113 |
| Environmental | 7.49 | 2.51 | 14.43 | 43 | 10.85 | 3.66 | 19.02 | 38 | 3.36 | 155 |
| Maternal Child Health | 10.93 | 2.19 | 21.71 | 48 | 19.08 | 2.80 | 41.80 | 55 | 8.15 | 143 |
| Access and Linkage | 4.56 | 0.77 | 9.58 | 52 | 8.42 | 1.15 | 18.94 | 57 | 3.86 | 139 |
| Tot. Found. Areas | 29.68 | 17.03 | 43.66 | 23 | 50.60 | 27.80 | 78.00 | 26 | 20.92 | 70 |
| Total FPHS | 48.14 | 33.31 | 64.32 | 16 | 82.43 | 55.00 | 114.40 | 19 | 34.28 | 50 |
Estimates of the current resources devoted to FPHS by local public health agencies in the study cohort totaled $48.14 per capita in 2014–2015, including $18.46 for Foundational Capabilities and $29.68 for Foundational Areas. Organizational competencies accounted for the largest share of resources devoted to Foundational Capabilities, contributing 53 percent of these costs. Communication accounted for the smallest share of resources devoted to Foundational Capabilities, contributing 3.4 percent of these costs. The Maternal and Child Health domain accounted for the largest share of resources devoted to Foundational Areas, contributing nearly 37 percent of these costs. The Chronic Disease and Injury Prevention domain accounted for the smallest share of resources devoted to Foundational Areas, contributing 11.1 percent of these costs. Estimates of the expected costs to achieve full attainment of the FPHS were more than 70 percent larger than the estimates of current resource use. Expected costs totaled $82.43 per capita, including $31.82 for Foundational Capabilities and $50.60 for Foundational Areas. Expected cost estimates were more than twice as large as current cost estimates in four FPHS domains: Assessment, Emergency Preparedness, Policy Development, and Chronic Disease and Injury Prevention. These estimates imply that reaching full attainment of FPHS in these domains would require more than a twofold increase in resources per capita. Subtracting expected costs from current costs yields an estimated resource gap that totals $34.29 per capita. More than 60 percent of this resource gap is attributable to Foundational Areas, while 39 percent is attributable to Foundational Capabilities.
Because the FPHS elements are defined using general terms, this leaves considerable room for interpretation regarding resource requirements. The lower‐bound and upper‐bound cost estimates produced by this analysis, representing 2.5th and 97.5th percentiles of the cost distribution, reflect the uncertainties inherent in the FPHS definitions. Overlaying the probability distribution graphs of our current and expected FPHS costs provides additional insight into the uncertainty associated with our estimates (Figure 3). By comparing their shape, their gap, and corresponding variation, these types of graph overlays can serve as a useful decision‐making aid to inform the level of investment needed to fully implement FPHS.3 Consistent with the CV values reported in Table 1, we observe a “tighter” spread in the shape of the distribution for current per capita costs compared to the projected FPHS cost distribution. We attribute the higher CV for expected costs of full FPHS attainment to the uncertainty inherent in prospective costing methodologies. By contrast, we expect less uncertainty with estimating current costs as these involve retrospective and concurrent approaches informed by direct information sources such as financial reports and administrative records.
Figure 3.
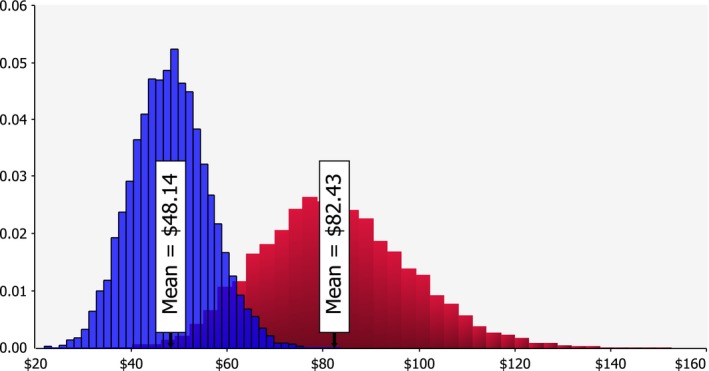
Overlay of Probability Density Graphs for Current and Expected FPHS per Capita Costs [Color figure can be viewed at http://wileyonlinelibrary.com]
Discussion
The Foundational Public Health Services framework represents a national expert panel consensus on the set of essential skills and capabilities that every public health agency should have to protect and improve health status across the American population. While the cost estimates generated from the simulation model results may not be nationally representative, they still represent and serve as first‐generation cost estimates using the FPHS framework. To put these estimates into perspective, we scale them up to the total U.S. population size in 2014 to try and draw some implications within the context of the recent impetus toward acquiring a clearer understanding of the U.S. public health system's fundamental components and costs.
Evaluating current levels of resources devoted to FPHS, we estimate that current costs incurred by state and local public health agencies in implementing FPHS totaled $15.4 billion or just over $48 per capita in 2014–2015 as reported from our model results. This level of resource use allows the U.S. public health system to implement more than 60 percent of the skills and capabilities represented in the FPHS recommendations (i.e., 100 percent attainment). These estimates imply that public health agencies currently devote approximately 23 percent of their resources to FPHS, with the remaining 77 percent of spending devoted to Type 1 activities representing categorical public health programs and services.
Full attainment of the FPHS recommendations developed by the Public Health Leadership Forum would require an estimated $34.29 per capita or $10.94 billion in additional resources per year based on these estimates. Generating these additional resources would require state and local governments to increase their spending on public health activities by 16.1 percent over the levels estimated in the National Health Expenditure Accounts for 2014 (CMS 2016). Alternatively, the estimated resource gap could be filled by nearly doubling federal government spending on public health activities from the $11.0 billion estimated in 2014. Overall, we find that our resource gap estimates are consistent with the Institute of Medicine's 2012 report that recommended a doubling of the federal government's expenditures for public health activities to fund a minimum package of public health services (IOM 2012).
As with any simulation study that relies on data where bias can be introduced from voluntary participation, self‐reported surveys, and expert opinion, it is important to keep in mind several limitations when using the results from this analysis. For one, the cost estimates produced in this analysis are based on cost data collected from a sample of only 19 agencies in three states and are therefore not fully representative of the nation as a whole. Even with the simulation model approach to account for uncertainty in the cost estimates, it should be noted that the simulations only serve as a tool for adding subjectively derived variances of the FPHS cost components; simulation does not formally address sampling error or the effect on the simulation distribution of possible correlation of errors across the FPHS domains.
The linearity assumption of the implementation attainment scale used for calculating full FPHS attainment costs is another limitation of the analysis as the true functional form of the relationship between FPHS costs and attainment level is unknown. Thus, the “percentage” formula used for estimating the total or incremental cost of 100 percent attainment is essentially based on an extrapolation from existing data and currently cannot be theoretically or empirically justified. Further investigation into modeling FPHS costs, particularly the expected cost function associated with full FPHS attainment, will be helpful in addressing this limitation. It should also be noted that the cost estimates reflect the resources required to implement FPHS using existing approaches for organizing and implementing public health services at state and community levels. Hence, our models do not reflect economies of scale and scope that may be possible through alternative organizational and implementation strategies. Lastly, the cost estimates generated in this study are limited to Type 2 activities reflected in the Public Health Leadership Forum's FPHS recommendations. They do not include resources required for implementing Type 1 activities, which are also essential elements for improving population health and well‐being. Further work will be necessary to estimate the resource requirements for essential Type 1 activities to provide a complete assessment of the costs required to realize a minimum package of public health services for the nation.
Conclusion
In this paper, we presented results from a stochastic simulation model designed to estimate the cost of implementing a set of Foundational Public Health Services as recommended by the Institute of Medicine while accounting for the dynamic nature of public health service delivery and demand. The results suggest substantial variation in costs across FPHS domains and a substantial gap between current costs of FPHS implementation and the expected costs to fully meet FPHS needs. We also show how the resource gap estimates presented in this study can be used for priority‐setting purposes to inform policy as it relates to determining the level of investments needed in prevention and public health.
The rationale for the Institute of Medicine minimum package recommendations was motived by the uncertainty over what was essential to health departments everywhere and how much it would cost. Even with the FPHS framework in place, policy makers will still need to determine investment and resource allocation decisions—all under uncertainty. That uncertainty is further driven by lack of data on costs for developing the essential public health services infrastructure which has constrained the ability of public health leaders to make a clear economic case for committing the required investments in population‐based health services (Whittington et al. 2016). The demand for empirically demonstrating value in public health, and the challenges and complexities in priority setting, is likely to grow over time as policy makers and practitioners at all governmental levels face budget constraints coupled with an increasingly challenging fiscal environment (Jacobson and Neumann 2009; Kinner and Pellegrini 2009; Ingram, Bernet, and Costich 2012). Therefore, having a comprehensive accounting of available and required public health resources is critical for ensuring that policy makers can make informed decisions that lead to the efficient allocation of those resources (Budetti and Lapolla 2008; Jacobson and Neumann 2009; Honore 2015).
In conclusion, the cost estimation work presented in this paper is intended to further develop the FPHS framework and promote its use to inform broader efforts to address health disparities, secure sustainable funding for governmental health agencies to have robust roles within the health system, and help contribute to realizing a minimum package of public health services for the nation.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported by Grant #72043 and Grant #72949 from the Robert Wood Johnson Foundation. The authors thank Georgia Heise, the Kentucky Health Departments Association, Terry Allan, the Association of Ohio Health Commissioners, and members of the Public Health Leadership Forum for their helpful assistance and support. The authors declare that they have no relevant or material financial interests that relate to the research described in this study.
Disclosure: None.
Disclaimer: None.
Notes
Our study cohort combined two separate samples. The first sample was comprised of nine local health agencies that participated in our pilot survey from July 2014 to April 2015 with the assistance and collaboration of the Kentucky Health Departments Association and Association of Ohio Health Commissioners. The second sample included 10 agencies from Washington State that collected cost data using a separate measurement tool developed by the Public Health Activities and Services Tracking (PHAST) Study team at the University of Washington (Bekemeier et al. 2017). The Washington tool used FPHS definitions and measures that were tailored for Washington's state‐specific public health planning initiative, but these data are generally consistent with the national FPHS definitions and measures. In providing data collection guidance on FPHS resource use and requirements, we advised survey respondents to use information from agency budget and financial reporting statements from their most recently completed fiscal year.
Given that the true underlying cost distributions across the FPHS domains are unknown, a commonly used approximate, less time‐consuming, and demanding method is to assess these probability distributions to elicit expert opinion in terms of just three parameters—the minimum, maximum, and most likely (modal) values—as these three values can be used to fit one of the two convenient distributions: the triangular distribution or the Program Evaluation and Review Technique (PERT) distribution. The appeal of the PERT distribution is that it maintains the tractability of our analysis but avoids the unrealistic shape of the triangle distribution. A special case of the beta distribution, sampling from the PERT distribution, requires the same three parameters of a minimum, maximum, and most likely value in addition to two shape parameters and a scale parameter, but generally assigns more probability to outcomes near the mode and less to the tails then the triangle distribution with the same parameters (Vose 2008). Unlike the triangular distribution, which may emphasize the modal value at the expense of the values on either side, the smooth curve of the PERT distribution allows us the flexibility of assuming an expectation, while the most likely value may not be exactly accurate that the model simulation results will be close to that estimate.
While the discussion focuses on aggregate estimates from the combined cohort of participating sites in our study sample, we can use our cost estimation model to also examine geographic variation in costs at various levels of granular interest such as FPHS costs by public health population jurisdiction size, and by state and local health agency governance. For example, we find that the average coefficient of variation for current, expected, and resource gap FPHS costs between the three participating sites in our study sample is 16 percent, 14 percent, and 70 percent, respectively.
References
- Bekemeier, B. , Marlowe J., Squires L. S., Tebaldi J., and Park S.. 2017. “Perceived Need Versus Current Spending: Gaps in Providing Foundational Public Health Services in Communities.” Journal of Public Health Management and Practice Publish Ahead of Print. Available at: http://journals.lww.com/jphmp/Abstract/publishahead/Perceived_Need_Versus_Current_Spending___Gaps_in.99559.aspx [DOI] [PubMed] [Google Scholar]
- Budetti, P. P. , and Lapolla M.. 2008. “Aligning Public Health Spending and Priorities in Oklahoma.” Journal of Public Health Management & Practice 14 (3): 289–98. [DOI] [PubMed] [Google Scholar]
- CMS . 2016. U.S. Centers for Medicare and Medicaid Services, Office of the Chief Actuary. National Health Expenditure Accounts, Historical 1980–2014. Baltimore, MD: CMS; [accessed on October 23, 2016]. Available at https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical.html [Google Scholar]
- Honore, P. A. 2015. “Transforming Public Health Economic and Financial Analytical Practices Through the Affordable Care Act.” Journal of Public Health Management & Practice 21 (1): 83–6. [DOI] [PubMed] [Google Scholar]
- Ingram, R. , Bernet P., and Costich J.. 2012. “Public Health Services and Systems Research: Current State of Finance Research.” Journal of Public Health Management & Practice 18 (6): 515–19. [DOI] [PubMed] [Google Scholar]
- IOM . 2012. For the Public's Health: Investing in a Healthier Future. Washington, DC: Institute of Medicine Committee on Assuring the Health of the Public in the 21st Century; [accessed on December 2, 2015]. Available at http://iom.nationalacademies.org/Reports/2012/For-the-Publics-Health-Investing-in-a-Healthier-Future.aspx [Google Scholar]
- IOM . 2013. U.S. Health in International Perspective: Shorter Lives, Poorer Health. Institute of Medicine of the National Academy of Sciences. Washington, DC: National Academies Press; [accessed on October 23, 2016]. Available at http://www.nationalacademies.org/hmd/Reports/2013/US-Health-in-International-Perspective-Shorter-Lives-Poorer-Health.aspx [PubMed] [Google Scholar]
- Jacobson, P. D. , and Neumann P. J.. 2009. “A Framework to Measure the Value of Public Health Services.” Health Services Research 44(5p2): 1880–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinner, K. , and Pellegrini C.. 2009. “Expenditures for Public Health: Assessing Historical and Prospective Trends.” American Journal of Public Health 99 (10): 1780–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays, G. P . 2014. “Estimating the Costs of Foundational Public Health Capabilities: A Recommended Methodology.” University of Kentucky [accessed on December 2, 2015]. Available at http://works.bepress.com/glen_mays/128
- Mays, G. P. , Mamaril C. B., and Timsina L.. 2016. “Multi‐Sector Contributions to Population Health Activities Lead to Reductions in Preventable Deaths. Health Affairs (35): 11. [DOI] [PubMed] [Google Scholar]
- Mays, G. P. , and S. A., Smith . 2009. “Geographic Variation in Public Health Spending: Correlates and Consequences.” Health Services Research 44(5 Pt 2): 1796–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays, G. P. , Scutchfield F. D., Bhandari M. W., and Smith S. A.. 2010. “Understanding the Organization of Public Health Delivery Systems: An Empirical Typology.” Milbank Quarterly 88(1): 81–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver, T. R. 2006. “The Politics of Public Health Policy.” Annual Review of Public Health 27: 195–233. [DOI] [PubMed] [Google Scholar]
- PHLF . 2014. “Defining and Constituting Foundational “Capabilities” and “Areas” Version 1 (V‐1).” RESOLVE [accessed on December 2, 2015]. Available at http://www.phaboard.org/phnci/assets/Foundational%20Capabilities%20and%20Areas%20version%201.0.pdf
- Tsuchiya, A. , Miguel L. S., Edlin R., Wailoo A., and Dolan P.. 2005. “Procedural Justice in Public Health Care Resource Allocation.” Applied Health Economics and Health Policy 4(2): 119–27. [DOI] [PubMed] [Google Scholar]
- Vose, D . 2008. Risk Analysis: A Quantitative Guide. Chichester, UK; Hoboken, NJ: Wiley. [Google Scholar]
- Whittington, M. , Atherly A., VanRaemdonck L., and Lampe S.. 2016. “Strategic Methodologies in Public Health Cost Analyses.” Journal of Public Health Management and Practice 1–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


