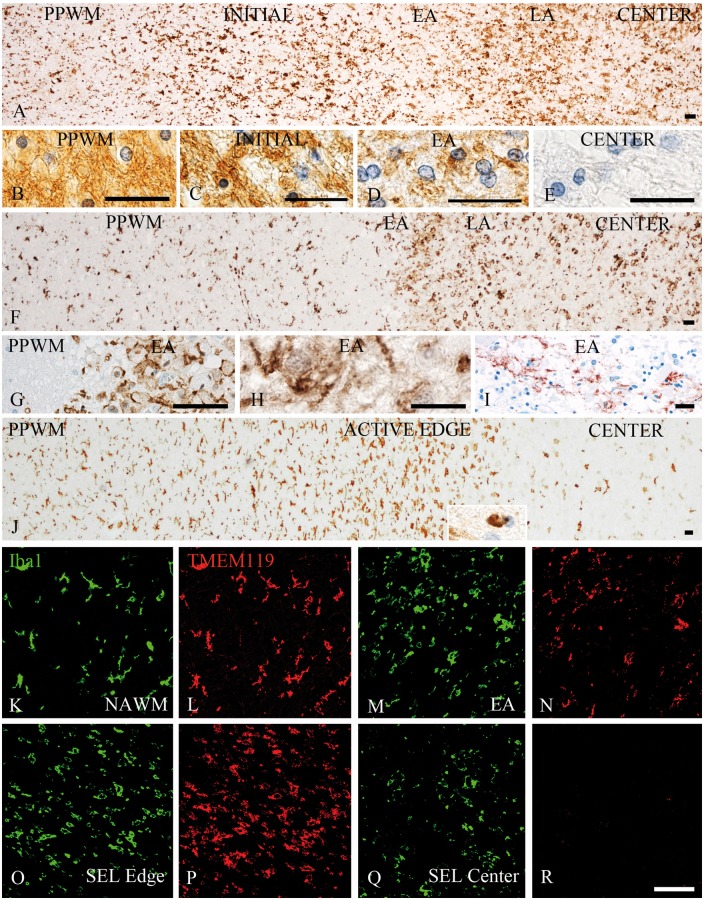
Figure 1.
Patterns of microglia and macrophage reaction in different types of multiple sclerosis lesions. (A–E) Active lesion following pattern III demyelination as defined by Lucchinetti et al. (2000) in a patient with acute multiple sclerosis; (A) low magnification image depicting the distribution and morphology of Iba1-positive cells in different zones of the active lesions including the peri-plaque white matter (PPWM), the initial ‘pre-phagocytic’ lesion area (INITIAL), the early active (EA) and the late active (LA) lesion zones and the macrophage-containing inactive lesion centre (CENTER). There is already profound microglia activation in the initial lesion areas and these cells are transformed into or replaced by macrophage-like cells in the areas, where myelin has been destroyed (early active, late active and centre); the myelin pathology in these different lesion areas are shown in B–E; normal myelin and glia are seen in the PPWM (B). In the initial area myelin is still preserved, but there is some oedema and many oligodendrocytes show nuclear condensation and chromatin margination reflecting apoptosis (C). In the early active zone, myelin is lost, but there are many macrophages with intracytoplasmic myelin degradation products reactive for MOG (D). No myelin or MOG reactivity is seen in the demyelinated lesion centre, but there are still many macrophages with empty vacuoles reflecting the neutral lipid stage of myelin degradation (E). (F–I) Active lesion following pattern II demyelination as defined by Lucchinetti et al. (2000) in a patient with acute multiple sclerosis. (F) Low magnification image depicting the distribution and morphology of Iba1-positive cells in different zones of the active lesions, including the peri-plaque white matter, the early active and the late active lesion zones and the macrophage-containing inactive lesion centre. In contrast to pattern III lesions, there is no zone of initial demyelination with oligodendrocyte apoptosis; in contrast, microglia density is reduced in a small zone surrounding the actively demyelinating lesion area (F and G) possibly due to recruitment of peri-plaque microglia to the site of active demyelination (early active and late active zones), the actively demyelinating area is characterized by a high density of cells with macrophage phenotype (F), which contain early myelin degradation products (H). In addition, there is deposition of activated complement (C9neo antigen) at the sites of active demyelination in these lesions (I). (J) Slowly expanding lesion in a patient with secondary progressive multiple sclerosis; low magnification image depicting the distribution and morphology of Iba1-positive cells in different zones of the active lesions including the peri-plaque white matter, the active lesion edge and the inactive lesion centre. An increased density of Iba1-positive cells with a phenotype of activated microglia is seen at the active edge; in contrast, there are only very few Iba1-positive microglia-like cells in the inactive lesion centre; the insert shows a macrophage with early myelin degradation products. (K–R) Double staining for Iba1 (green) and TMEM119 (red) shows co-expression of these molecules in most cells in the normal-appearing white matter (K and L) and the active edge of slowly expanding lesions (O and P), while TMEM119 is expressed only in a subset of cells with macrophage or microglia phenotype in early active multiple sclerosis lesions (M and N). In the centre of classical active lesions and slowly expanding lesions (SEL) Iba1-positive macrophages can be present, which are negative for TMEM119 (Q and R). Scale bars = 100 µm.