Abstract
Due to its rarity, current literature assessing prognostic factors and survival outcomes of hemangioblastoma is limited. Patients with histologically confirmed hemangioblastoma were identified from the US National Cancer Data Base. 1488 patients met inclusion criteria. 644 patients underwent gross total resection (GTR), 220 subtotal resection (STR)/biopsy, 60 stereotactic radiosurgery (SRS), 15 external beam radiotherapy (EBRT), 51 surgery followed by radiotherapy (SR + RT) and 498 no treatment. Independent predictors of shorter OS included age ≥ 40 (HR, 3.897; 95% CI, 2.341–6.487; p < 0.001), Charlson-Deyo score ≥ 1(HR, 1.756; 95% CI, 1.213–2.544; p = 0.003), tumor location in the brainstem (HR, 1.955; 95% CI, 1.129–3. 384; p = 0.017) compared to cerebellum, no treatment (HR, 2530; 95% CI, 1.533–4.177; p < 0.001) and receipt of EBRT (HR, 2.860; 95% CI, 1.073–7.618; p = 0.036) compared to STR/biopsy. GTR was associated with longer OS (HR 0.617; 95% CI, 0.391–0.974; p = 0.038), while SRS had comparable OS to STR/biopsy. The overall trend of OS by treatment modality was consistent after matching to age- and sex-matched US population data. In patients younger than 40 years, treatment was not a significant predictor of OS. In conclusion, GTR remained the optimal treatment for hemangioblastoma. SRS may perform similarly to surgery alone. Treatment was not a significant predictor of survival in younger patients.
Introduction
Hemangioblastomas of the central nervous system (CNS) are benign vascular neoplasms that most commonly affect the cerebellum, followed by the brainstem and spinal cord1. The majority of CNS hemangioblastomas arise sporadically, but 20–30% of cases develop in association with Von Hippel-Lindau (VHL) disease1. VHL disease is an autosomal dominant, multisystem neoplastic syndrome caused by mutations in the VHL tumor suppressor gene2. Compared to the sporadic form, hemangioblastomas associated with VHL disease tend to manifest earlier in life and as multifocal lesions1,3. Long-term surveillance is required due to risk of new tumor development4.
Given the indolent nature of hemangioblastomas5,6, asymptomatic tumors may be managed with observation, and intervention is not required until symptoms develop6. Standard clinical management for all symptomatic presentations is complete microsurgical resection1,7. In general, surgical resection is a safe and effective strategy4. However, post-operative outcomes can vary depending on factors including disease location, number of lesions, and tumor characteristics that make complete resections difficult8–10. Radiotherapy (RT), in the form of stereotactic radiosurgery (SRS) or external beam radiotherapy (EBRT), can be used as primary, adjuvant, or salvage treatment strategy11,12. However, the current accepted practice patterns are based on small and medium -sized retrospective studies that include fewer than 200 patients, and there are no randomized clinical trials that compare these approaches12–19. Consequently, it is unclear if certain subgroups of patients may benefit from different management strategies.
In this study, we used the National Cancer Database (NCDB) to compare treatment strategies in patients with hemangioblastomas.
Materials and Methods
Study populations
The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society. Established in 1989, the NCDB is a comprehensive, nationwide facility-based oncology data set that captures nearly 70% of all newly diagnosed malignancies in the United States. The data used in this study are derived from a deidentified NCDB data file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology used, or for the conclusions drawn, from these data by investigators.
The NCDB was used to identify patients with hemangioblastoma from 2004 to 2013. In this study, we excluded patients with incomplete survival data and unknown extent of resection or tumor location. The flowchart of patient selection is shown in Fig. 1. Demographic and clinical data included age, race, sex, year of diagnosis, Charlson-Deyo score, tumor size, tumor location, lesion number, metastasis, and treatments. Tumor location of ventricle, overlapping lesion of central nervous system, cauda equina and cranial nerves was categorized as “other site of CNS” per NCDB. We included patients who received both EBRT and SRS.
Figure 1.
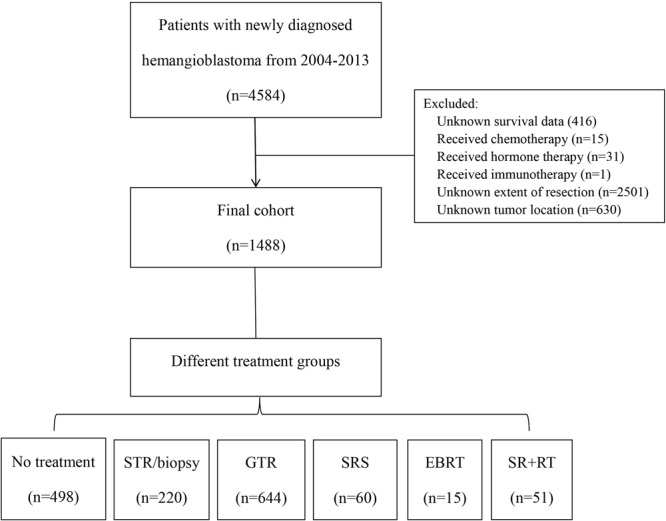
Patient selection flowchart.
Statistical methods
All data analyses were performed using SPSS 22.0 (SPSS Inc., Chicago, IL). Demographic factors and tumor characteristics of the overall cohort were analyzed using the Student’s t test for continuous variables and chi-square test for categorical variables. Univariable followed by multivariable Cox proportional hazard regression was used to identify significant predictors of OS. Variables with p value < 0.05 on univariate analysis was included in the multivariate analysis with the Cox proportional hazards model. A two-sided p value of < 0.05 was considered statistically significant. Subgroup analyses based on age were also performed. Using the R package relsurv, a “proportional excess hazard model”20,21 was used to analyze OS relative to age- and sex-matched population data from the Centers for Disease Control and Prevention to determine the excess risk of death associated with hemangioblastomas beyond what can be attributed to a patient’s age and sex22.
Data availability
The data that support the findings of this study are available from National Cancer Database (NCDB) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of NCDB.
Results
Patient characteristics
A total of 1488 patients met our inclusion criteria (Fig. 1). For all patients in our study, the median follow-up time was 33 months (range, 0–140 months). The median age at diagnosis was 49 years (range, 2–90 years); 55.3% patients were male; 75.6% were white; 80.6% had no significant comorbidities (Charlson-Deyo score of 0). In terms of treatment, 864 (58.2%) underwent surgery alone, 75 (5%) RT alone, 51 (3.4%) surgery followed by RT (surgery + RT), and 498 (33.5%) no treatment. Among patients who underwent surgery alone, 644 (76.9%) had gross total resection (GTR), and 220 (25.5%) subtotal resection (STR) or biopsy. Among patients who received RT alone, 60 (89%) received SRS, and 15 (20%) EBRT. Tumor size treated by SRS was much smaller than other treatments (p < 0.001; Fig. 2). The most common tumor location was the cerebellum (n = 1060, 71.2%) followed by the spinal cord (n = 145, 9.7%). A summary of demographic and clinical features of our cohort is shown in Table 1.
Figure 2.
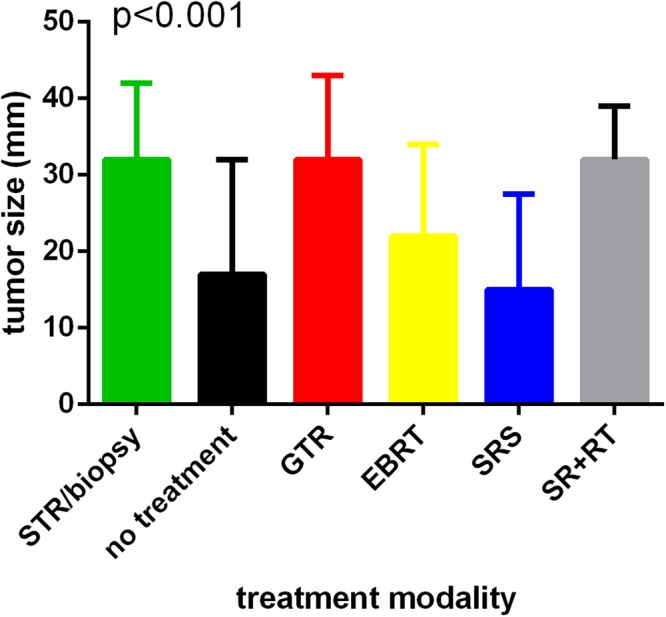
Tumor size distribution between different treatment modalities.
Table 1.
Demographics and clinical characteristics of the overall cohort (n = 1488).
| Category | Subcategory | No. (%) |
|---|---|---|
| Age at diagnosis, y | Median | 49 |
| IQR | 35–61 | |
| Age at diagnosis, y | <40 year | 506 (34.0) |
| ≧40 year | 982 (66.0) | |
| Gender | Male | 823 (55.3) |
| Female | 665 (44.7) | |
| Race | White | 1126 (75.6) |
| African American | 147 (9.9) | |
| Asian | 52 (3.5) | |
| Hispanic | 132 (8.9) | |
| Others/Unknown | 31 (2.1) | |
| Year of diagnosis | 2004 | 26 (1.7) |
| 2005 | 31 (2.1) | |
| 2006 | 29 (1.9) | |
| 2007 | 28 (1.9) | |
| 2008 | 41 (2.8) | |
| 2009 | 54 (3.6) | |
| 2010 | 308 (20.7) | |
| 2011 | 318 (21.4) | |
| 2012 | 340 (22.9) | |
| 2013 | 313 (21.0) | |
| Charlson-Deyo Score | 0 | 1199 (80.6) |
| ≧1 | 289 (19.4) | |
| Tumor size | <4 cm | 808 (54.3) |
| ≧4 cm | 338 (22.7) | |
| Unknown | 342 (23.0) | |
| Number of tumors | Unifocal | 1168 (78.5) |
| Multifocal | 90 (6.0) | |
| Unknown | 230 (15.5) | |
| Tumor location | Cerebrum+ | 127 (8.5) |
| Cerebellum | 1060 (71.2) | |
| Brainstem | 91 (6.1) | |
| Spinal cord | 145 (9.7) | |
| Meninges | 31 (2.1) | |
| Other site of CNS++ | 34 (2.3) | |
| Behavior | Benign | 9 (0.6) |
| Borderline | 1475 (99.1) | |
| Invasive | 4 (0.3) | |
| Metastasis | No | 1382 (92.9) |
| Yes | 3 (0.2) | |
| Unknown | 103 (6.9) | |
| Treatment | No treatment | 498 (33.5) |
| STR/biopsy alone | 220 (14.8) | |
| GTR alone | 644 (43.3) | |
| SRS | 60 (4.0) | |
| EBRT | 15 (1.0) | |
| SR + RT | 51 (3.4) | |
| Facility location | Eastern | 398 (26.7) |
| Central | 361 (24.3) | |
| Western | 223 (15.0) | |
| Unknown | 506 (34.0) | |
| Median income | <$38,000 | 217 (14.6) |
| $38,000–$47,999 | 329 (22.1) | |
| $48,000–$62,999 | 393 (26.4) | |
| ≥$63,000 | 536 (36.0) | |
| Unknown | 13 (0.9) | |
| Proportion without high school degree in patient’s area of residence | ≥21% | 247 (16.6) |
| 13–20.9% | 328 (22.0) | |
| 7–12.9% | 510 (34.4) | |
| <7% | 392 (26.3) | |
| Unknown | 11 (0.7) | |
| Insurance | Uninsured | 116 (7.8) |
| Private insurance/managed care | 866 (58.2) | |
| Government insurance | 467 (31.4) | |
| Unknown | 39 (2.6) | |
| Urban/rural | Urban | 1422 (95.6) |
| Rural | 27 (1.8) | |
| Unknown | 39 (2.6) |
Abbreviations: IQR, Inter Quartile Range; p, probability; STR, subtotal resection; GTR, gross total resection; EBRT, external beam radiotherapy; SRS, stereotactic radiosurgery; SR, surgery; RT, radiotherapy; +include frontal lobe, temporal lobe, parietal lobe and occipital lobe; ++include ventricle, overlapping lesion of central nervous system, cauda equina and cranial nerves.
Survival analyses
The 1-, 3-, 5- and 10-year OS rate was 95%, 91%, 87%, 78%, respectively (Fig. 3). The 5-year OS of GTR group was 91%, followed by STR/biopsy (89%), SR + RT (88%), SRS (85%), no treatment (78%) and EBRT (71%). Independent predictors of shorter OS on multivariate Cox regression analysis included age ≥40 (HR, 3.897; 95% CI,2.341–6.487; p < 0.001), Charlson-Deyo score ≥1 (HR, 1.756; 95% CI, 1.213–2.544; p = 0.003), tumor location in the brainstem (HR, 1.955; 95% CI, 1.129–3. 384; p = 0.017) or other site of CNS (HR, 2.754; 95% CI, 1.268–5.980; p = 0.010) when compared to the cerebellum, no treatment (HR, 2.530; 95% CI, 1.533–4.177; p < 0.001) and EBRT (HR, 2.860; 95% CI, 1.073–7.618; p = 0.036) when compared to STR/biopsy. GTR was associated with longer OS (HR, 0.617; 95% CI, 0.391–0.974; p = 0.038) when compared to STR/biopsy (Fig. 4). The results of the Cox regression analyses are shown in Table 2. The overall trend of relative survival after matching to age- and sex-matched US population data was consistent, with patients who underwent GTR, SRS and surgery + RT demonstrating the best survival outcomes, followed by STR/biopsy, no treatment, and EBRT (Supplementary Fig. 1).
Figure 3.

Overall survival of the entire cohort.
Figure 4.
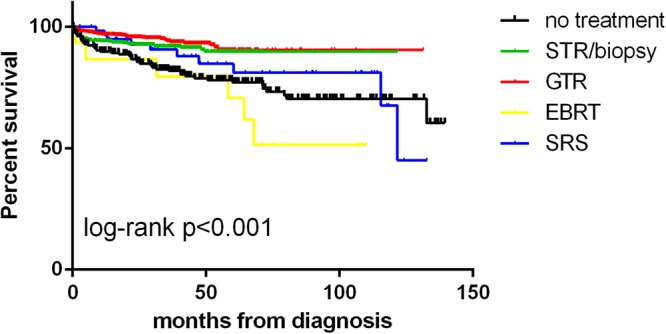
Comparison of overall survival among the different treatment groups. Supplementary Fig. 1. Overall trend of relative survival after matching to age- and sex-matched US population data.
Table 2.
Univariable and multivariate Cox proportional hazards analyses of overall survival (n = 1488).
| Variable | Univariate analyses | Multivariate analyses | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age | ||||
| <40 years | Ref. | — | Ref. | — |
| ≧40 years | 3.919 (2.379–6.456) | <0.001* | 3.897 (2.341–6.487) | <0.001* |
| Gender | ||||
| Male | Ref. | — | ||
| Female | 0.868 (0.622–1.210) | 0.402 | ||
| Race | 0.299 | |||
| White | Ref. | — | ||
| African American | 1.431 (0.868–2.360) | 0.160 | ||
| Asian | 1.665 (0.774–3.580) | 0.192 | ||
| Hispanic | 0.903 (0.485–1.680) | 0.747 | ||
| Year of diagnosis | ||||
| 2004–2008 | Ref. | — | Ref. | — |
| 2009–2013 | 0.518 (0.344–0.780) | 0.002* | 1.057 (0.627–1.783) | 0.834 |
| Charlson-Deyo Score | ||||
| 0 | Ref. | — | Ref. | — |
| ≧1 | 2.006 (1.403–2.867) | <0.001* | 1.756 (1.213–2.544) | 0.003* |
| Tumor size | ||||
| <4 cm | Ref. | — | ||
| ≧4 cm | 0.987 (0.653–1.491) | 0.949 | ||
| Number of tumors | ||||
| Unifocal | Ref. | — | ||
| Multifocal | 0.940 (0.432–2.042) | 0.875 | ||
| Tumor location | 0.025* | 0.019* | ||
| Cerebrum+ | 1.088 (0.595–1.989) | 0.784 | 0.898 (0.487–1.655) | 0.729 |
| Cerebellum | Ref. | — | Ref. | — |
| Brainstem | 2.088 (1.226–3.555) | 0.007 | 1.955 (1.129–3. 384) | 0.017 |
| Spinal cord | 1.023 (0.582–1.799) | 0.936 | 0.781 (0.438–1.394) | 0.404 |
| Meninges | 1.598 (0.647–3.949) | 0.310 | 1.218 (0.484–3.069) | 0.675 |
| Other sites of CNS++ | 2.593 (1.201–5.598) | 0.015 | 2.754 (1.268–5.980) | 0.010 |
| Metastasis at diagnosis | ||||
| M0 | Ref. | — | ||
| M+ | 0.050 (0–32455.797) | 0.708 | ||
| Treatment | <0.001* | <0.001* | ||
| No treatment | 2.068 (1.341–3.188) | 0.001 | 2.530 (1.533–4.177) | <0.001 |
| STR/biopsy alone | Ref. | — | Ref. | — |
| GTR alone | 0.662 (0.421–1.043) | 0.075 | 0.617 (0.391–0.974) | 0.038 |
| EBRT | 3.432 (1.446–8.144) | 0.005 | 2.860 (1.073–7.618) | 0.036 |
| SRS | 1.444 (0.716–2.913) | 0.305 | 1.459 (0.683–3.118) | 0.329 |
| SR + RT | 1.242 (0.490–3.147) | 0.648 | 1.089 (0.428–2.770) | 0.858 |
Abbreviations: HR, Hazards Ratio; CI, confidence interval; P, probability; Ref., reference; M0, no metastasis at diagnosis; M+ , with metastasis at diagnosis; STR, subtotal resection; GTR, gross total resection; EBRT, external beam radiotherapy; SRS, stereotactic radiosurgery; SR, surgery; RT, radiotherapy; +include frontal lobe, temporal lobe, parietal lobe and occipital lobe; ++include ventricle, overlapping lesion of central nervous system, cauda equina and cranial nerves *means statistically significant.
Subgroup analysis based on age
Patients were divided into two groups based on an age cutoff of 40 years. The demographic and clinical features of the two age subgroups are shown in Supplementary Table 1. Younger patients were more likely to be non-white and without comorbidities, while their tumors tended to be larger, multifocal and located in the spinal cord. On multivariate Cox regression analysis, no treatment (adjusted HR, 2.578; 95% CI, 1.528–4.351; p < 0.001) and EBRT (adjusted HR, 4.199; 95% CI, 1.573–11.207; p = 0.004) were associated with shorter OS in older patients, while GTR was associated with longer OS when compared to biopsy/STR (adjusted HR, 0.571; 95% CI, 0.349–0.935; p = 0.026). In contrast, treatment was not a significant predictor of OS for younger patients. The results of the Cox regression analyses are shown in Supplementary Tables 2 and 3.
Discussion
Due to its rarity, current literature assessing prognostic factors and survival outcomes of hemangioblastoma is limited9,17,23–25. Consequently, the established guidelines for treatment are based on small to medium-sized retrospective studies. In this study, we analyzed a large cohort of patients with hemangioblastomas using the NCDB.
Our analysis found that receipt of surgery was associated with longer OS. Due to the stuttering growth pattern and indolent nature of hemangioblastomas, symptomatic progression of these tumors is difficult to predict6,26. Therefore, while asymptomatic sporadic tumors can be managed with observation, therapeutic intervention is generally recommended. This is supported in our analysis with receipt of surgery having better outcomes than no treatment. Tumor size was not associated with survival on univariate analysis. However, patients with larger tumors were more likely to undergo resection. Notably, due to small cohort sizes, there is very little data in the current literature assessing survival outcomes based on extent of resection. However, several studies have reported increased rate of intra-operative and post-operative hemorrhage in patients who underwent a partial resection, likely secondary to the highly vascular nature of the tumor4,7,17,27–29. This suggests that STR may carry a greater risk of morbidity.
Our results showed that GTR resulted in longer OS than STR/biopsy. Nevertheless, cases in which aggressive tumor removal may be detrimental for patient outcomes should always be considered, as GTR has the potential to damage nearby cranial structures and produce significant patient morbidity. This may be particularly relevant for hemangioblastomas originating from the brainstem as these tumors were found to have worse OS when compared to cerebellar tumors in our cohort and are oftentimes proximal to critical structures. A number of studies have emphasized the need for meticulous resection of brainstem lesions for this reason8,23,29,30.
Compared to resection, the role of RT in the treatment of hemangioblastomas is less well-defined. Given the considerable interest in the use of RT as a minimally invasive primary or adjuvant treatment strategy13,18,31, we analyzed how primary SRS and EBRT perform compared to surgery in this cohort. Our results demonstrate that patients who underwent SRS or EBRT as primary treatment had smaller tumor size when compared to patients who underwent surgery, while size of tumor was similar to surgery alone in patients who had adjuvant RT after surgery. On relative survival analysis, SRS trended towards a similar relative survival compared to GTR. In contrast, on Cox regression analysis, SRS yielded comparable survival outcomes to STR/biopsy. These results are limited by the small number of patients undergoing primary SRS in our cohort, but may indicate that SRS at least provides comparable survival outcomes to surgery. In the literature, while several studies have presented outcomes for hemangioblastomas treated by SRS11,18,19,24,32–34, none has directly compared their findings to resection. In a study of 186 patients, Kano et al. found that SRS provided decent tumor control with improved outcomes for small, solid-type tumors but was unable to compare those results to surgical outcomes11. While limited by our cohort size, our findings support the use of SRS as a reasonable alternative to surgery alone especially for small tumors. Additionally, EBRT is generally only indicated when surgery and SRS are not viable options12. Studies describing the use of EBRT in the management of hemangioblastoma are very limited. In the largest paper discussing use of EBRT (n = 18), Koh et al. noted this modality has a role in managing extensive, multifocal disease, tumors adjacent to critical structures, and treatment of residual or recurrent tumors12. In our study, receipt of EBRT was associated with a significantly worse OS, and this may be related to the unfavorable prognostic factors in patients who were selected for this treatment. Nevertheless, given the limited number of patients in our cohort undergoing SRS (n = 60) and EBRT (n = 15) as primary treatment, further investigation is necessary to fully evaluate the role of RT in management of this disease. Although we did not find a survival benefit of post-operative RT, the small number of patients undergoing both surgery and post-operative RT in our cohort, (n = 51) made it difficult to assess the efficacy of RT as an adjuvant treatment.
When our cohort was stratified by age, we found that for patients <40 years of age, treatment was not a significant prognostic factor of survival. In contrast, treatment remained a predictive factor for patients >40 years of age, with similar trend to the overall cohort. These findings may be related to the fact that younger patients are more likely to have VHL-related hemangioblastomas, and older patients are more likely to have sporadic tumors. The average age at time of diagnosis for VHL patients is generally in the third decade1,5,6,9,35 with one series noting all VHL-associated hemangioblastoma cases presenting at age 40 or younger36. In contrast, average age at time of diagnosis for sporadic cases is much more likely to be greater than 40 years1,9,35. Higher prevalence of brainstem and multifocal lesions in the <40 age group also suggests that the younger age group encompasses the majority of patients with VHL disease in our cohort. What remains a significant challenge for providers is determining the optimal management strategy for VHL patients in which disease progression is attributed to manifestations of symptoms associated with new tumor development. The frequency of intervention should be minimized in order to avoid additional treatment-related morbidities over time4,5. Our findings underscore the need for careful longitudinal surveillance of VHL patients because successful therapy may not lead to better survival outcomes.
We acknowledge a few limitations. First, there was selection bias associated with a retrospective analysis. Second, because there was no central pathology review, misdiagnosed cases of hemangioblastomas could be present in our study cohort. Third, because data on recurrence was not available, progression-free survival could not be assessed. Likewise, data on clinical manifestations or neurological status was not provided by the NCDB, limiting the conclusions that can be made about site-specific surgical risks and outcomes37. Fourth, the limited size and quality of data makes it difficult to draw definite conclusion on the efficacy of RT. Finally, the database does not have information on VHL, so we used age <40 as a surrogate marker for a VHL diagnosis. Despite these limitations, the large sample size allows for meaningful trends to be observed with adequate power across multiple healthcare systems. Further studies focusing on patients with a definite VHL diagnosis and those who were treated with RT are needed to guide management of these specific populations.
Conclusion
Patients with smaller tumors were more likely to undergo no treatment or treated by SRS or EBRT as primary treatment. Brainstem tumors had worse outcomes than cerebellar tumors. GTR remained the optimal treatment for hemangioblastoma. SRS as primary treatment may perform similarly to surgery alone. Treatment was not a significant predictor of survival in younger patients with hemangioblastoma.
Electronic supplementary material
Acknowledgements
ShenghuaYuying Project of Central South University to L.Y. and National Science Foundation of China to XJL (81472594 and 81770781).
Author Contributions
Li Yang, Harrison X. Bai, Yuqian Huang and Lilian Chan conceptualized the project. Harrison X. Bai obtained the data used for this study. All authors contributed to data analysis and editing of the article.
Competing Interests
The authors declare no competing interests.
Footnotes
Yuqian Huang and Lilian Chan contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-29047-9.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bo Xiao, Email: Xiaobo_xy@126.com.
Li Yang, Email: yangli762@csu.edu.cn.
References
- 1.Neumann HP, et al. Hemangioblastomas of the central nervous system. A 10-year study with special reference to von Hippel-Lindau syndrome. Journal of neurosurgery. 1989;70:24–30. doi: 10.3171/jns.1989.70.1.0024. [DOI] [PubMed] [Google Scholar]
- 2.Gossage L, Eisen T, Maher ER. VHL, the story of a tumour suppressor gene. Nature reviews. Cancer. 2015;15:55–64. doi: 10.1038/nrc3844. [DOI] [PubMed] [Google Scholar]
- 3.Richard, S. et al. Central nervous system hemangioblastomas, endolymphatic sac tumors, and von Hippel-Lindau disease. Neurosurgical review23, 1–22; discussion 23–24 (2000). [DOI] [PubMed]
- 4.Conway, J. E. et al. Hemangioblastomas of the central nervous system in von Hippel-Lindau syndrome and sporadic disease. Neurosurgery48, 55–62; discussion 62–53 (2001). [DOI] [PubMed]
- 5.Wanebo JE, Lonser RR, Glenn GM, Oldfield EH. The natural history of hemangioblastomas of the central nervous system in patients with von Hippel-Lindau disease. Journal of neurosurgery. 2003;98:82–94. doi: 10.3171/jns.2003.98.1.0082. [DOI] [PubMed] [Google Scholar]
- 6.Ammerman JM, Lonser RR, Dambrosia J, Butman JA, Oldfield EH. Long-term natural history of hemangioblastomas in patients with von Hippel-Lindau disease: implications for treatment. Journal of neurosurgery. 2006;105:248–255. doi: 10.3171/jns.2006.105.2.248. [DOI] [PubMed] [Google Scholar]
- 7.Liao CC, Huang YH. Clinical features and surgical outcomes of sporadic cerebellar hemangioblastomas. Clinical neurology and neurosurgery. 2014;125:160–165. doi: 10.1016/j.clineuro.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 8.Chen LF, et al. Operative management of brainstem hemangioblastomas. Journal of clinical neuroscience: official journal of the Neurosurgical Society of Australasia. 2013;20:1727–1733. doi: 10.1016/j.jocn.2013.01.027. [DOI] [PubMed] [Google Scholar]
- 9.Weil RJ, Lonser RR, DeVroom HL, Wanebo JE, Oldfield EH. Surgical management of brainstem hemangioblastomas in patients with von Hippel-Lindau disease. Journal of neurosurgery. 2003;98:95–105. doi: 10.3171/jns.2003.98.1.0095. [DOI] [PubMed] [Google Scholar]
- 10.Van Velthoven, V., Reinacher, P. C., Klisch, J., Neumann, H. P. & Glasker, S. Treatment of intramedullary hemangioblastomas, with special attention to von Hippel-Lindau disease. Neurosurgery53, 1306–1313; discussion 1313–1304 (2003). [DOI] [PubMed]
- 11.Kano H, et al. Stereotactic radiosurgery for intracranial hemangioblastomas: a retrospective international outcome study. Journal of neurosurgery. 2015;122:1469–1478. doi: 10.3171/2014.10.JNS131602. [DOI] [PubMed] [Google Scholar]
- 12.Koh ES, et al. Role of fractionated external beam radiotherapy in hemangioblastoma of the central nervous system. International journal of radiation oncology, biology, physics. 2007;69:1521–1526. doi: 10.1016/j.ijrobp.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 13.Hanakita S, et al. The long-term outcomes of radiosurgery for intracranial hemangioblastomas. Neuro-oncology. 2014;16:429–433. doi: 10.1093/neuonc/not201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jagannathan J, Lonser RR, Smith R, DeVroom HL, Oldfield EH. Surgical management of cerebellar hemangioblastomas in patients with von Hippel-Lindau disease. Journal of neurosurgery. 2008;108:210–222. doi: 10.3171/JNS/2008/108/2/0210. [DOI] [PubMed] [Google Scholar]
- 15.Kanno H, et al. Spinal cord hemangioblastomas in von Hippel-Lindau disease. Spinal cord. 2009;47:447–452. doi: 10.1038/sc.2008.151. [DOI] [PubMed] [Google Scholar]
- 16.Parker F, et al. Results of microsurgical treatment of medulla oblongata and spinal cord hemangioblastomas: a comparison of two distinct clinical patient groups. Journal of neuro-oncology. 2009;93:133–137. doi: 10.1007/s11060-009-9861-0. [DOI] [PubMed] [Google Scholar]
- 17.Fukuda M, et al. Clinical factors predicting outcomes after surgical resection for sporadic cerebellar hemangioblastomas. World neurosurgery. 2014;82:815–821. doi: 10.1016/j.wneu.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Moss, J. M. et al. Stereotactic radiosurgical treatment of cranial and spinal hemangioblastomas. Neurosurgery65, 79-85; discussion 85, 10.1227/01.neu.0000348015.51685.d2 (2009). [DOI] [PubMed]
- 19.Kano, H. et al. The role of stereotactic radiosurgery for intracranial hemangioblastomas. Neurosurgery63, 443–450; discussion 450-441, 10.1227/01.neu.0000313120.81565.d7 (2008). [DOI] [PubMed]
- 20.Pohar M, Stare J. Relative survival analysis in R. Computer methods and programs in biomedicine. 2006;81:272–278. doi: 10.1016/j.cmpb.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 21.Dickman PW, Sloggett A, Hills M, Hakulinen T. Regression models for relative survival. Statistics in medicine. 2004;23:51–64. doi: 10.1002/sim.1597. [DOI] [PubMed] [Google Scholar]
- 22.Iyer JG, et al. Relationships among primary tumor size, number of involved nodes, and survival for 8044 cases of Merkel cell carcinoma. Journal of the American Academy of Dermatology. 2014;70:637–643. doi: 10.1016/j.jaad.2013.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wind JJ, et al. Long-term outcome after resection of brainstem hemangioblastomas in von Hippel-Lindau disease. Journal of neurosurgery. 2011;114:1312–1318. doi: 10.3171/2010.9.JNS10839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sayer, F. T., Nguyen, J., Starke, R. M., Yen, C. P. & Sheehan, J. P. Gamma knife radiosurgery for intracranial hemangioblastomas–outcome at 3 years. World neurosurgery75, 99–105; discussion 145–108, 10.1016/j.wneu.2010.09.032 (2011). [DOI] [PubMed]
- 25.Niu L, et al. The analysis of correlative factors affecting long-term outcomes in patients with Solid Cerebellar Hemangioblastomas. Clinical neurology and neurosurgery. 2016;150:59–66. doi: 10.1016/j.clineuro.2016.08.028. [DOI] [PubMed] [Google Scholar]
- 26.Lonser RR, et al. Prospective natural history study of central nervous system hemangioblastomas in von Hippel-Lindau disease. Journal of neurosurgery. 2014;120:1055–1062. doi: 10.3171/2014.1.JNS131431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glasker S, et al. Essentials and pitfalls in the treatment of CNS hemangioblastomas and von Hippel-Lindau disease. Central European neurosurgery. 2010;71:80–87. doi: 10.1055/s-0029-1234040. [DOI] [PubMed] [Google Scholar]
- 28.Wang, C., Zhang, J., Liu, A. & Sun, B. Surgical management of medullary hemangioblastoma. Report of 47 cases. Surgical neurology56, 218–226; discussion 226–217 (2001). [DOI] [PubMed]
- 29.Ma D, Wang Y, Du G, Zhou L. Neurosurgical Management of Brainstem Hemangioblastomas: A Single-Institution Experience with 116 Patients. World neurosurgery. 2015;84:1030–1038. doi: 10.1016/j.wneu.2015.05.030. [DOI] [PubMed] [Google Scholar]
- 30.Xu, Q. W., Xu, R., Du, Z. Y. & Gao, X. Surgical treatment for hemangioblastomas in the medulla oblongata. Acta neurochirurgica152, 1331–1335; discussion 1335, 10.1007/s00701-010-0668-8 (2010). [DOI] [PubMed]
- 31.Goyal N, et al. Stereotactic radiosurgery in hemangioblastoma: Experience over 14 years. Journal of neurosciences in rural practice. 2016;7:23–27. doi: 10.4103/0976-3147.172165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jawahar, A. et al. Stereotactic radiosurgery for hemangioblastomas of the brain. Acta neurochirurgica142, 641–644; discussion 644-645 (2000). [DOI] [PubMed]
- 33.Patrice SJ, et al. Radiosurgery for hemangioblastoma: results of a multiinstitutional experience. International journal of radiation oncology, biology, physics. 1996;35:493–499. doi: 10.1016/S0360-3016(96)80011-3. [DOI] [PubMed] [Google Scholar]
- 34.Wang EM, et al. The long-term results of gamma knife radiosurgery for hemangioblastomas of the brain. Journal of neurosurgery. 2005;102:225–229. doi: 10.3171/jns.2005.102.s_supplement.0225. [DOI] [PubMed] [Google Scholar]
- 35.Padhi S, et al. A 10-year retrospective study of hemangioblastomas of the central nervous system with reference to von Hippel-Lindau (VHL) disease. Journal of clinical neuroscience: official journal of the Neurosurgical Society of Australasia. 2011;18:939–944. doi: 10.1016/j.jocn.2010.12.050. [DOI] [PubMed] [Google Scholar]
- 36.Woodward ER, Wall K, Forsyth J, Macdonald F, Maher ER. VHL mutation analysis in patients with isolated central nervous system haemangioblastoma. Brain: a journal of neurology. 2007;130:836–842. doi: 10.1093/brain/awl362. [DOI] [PubMed] [Google Scholar]
- 37.Westwick HJ, Giguere JF, Shamji MF. Incidence and Prognosis of Spinal Hemangioblastoma: A Surveillance Epidemiology and End Results Study. Neuroepidemiology. 2016;46:14–23. doi: 10.1159/000441147. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from National Cancer Database (NCDB) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of NCDB.


