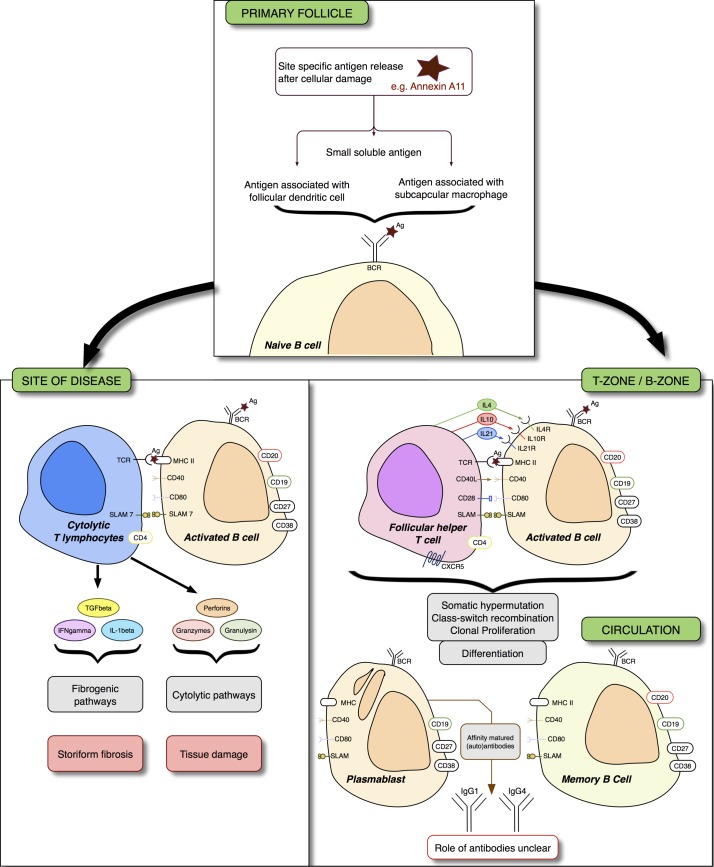
Figure 1.
Immunoglobulin G4-related disease (IgG4-RD) and immune pathways to therapy. Naïve B cells are activated by exposure to antigens. In tertiary lymph nodes or in tertiary lymphoid tissue within an affected tissue, T follicular helper (Tfh) cells help B cells differentiate into antibody secreting cells. Interleukins (IL) 4, 10 and 21 are critical to B-cell affinity maturation, class switching and clonal expansion. At the site of disease, B cells are thought to interact with cytolytic T cells by the mutual expression of signalling lymphocytic activation molecule 7 (SLAM7). These effector T cells secrete profibrogenic cytokines that may be critical to subsequent storiform fibrosis, and cytolytic enzymes. The exact nature of the B cell to cytotoxic T cell interaction is still unclear. Therapy targeting CD20 (rituximab) leads to a reduction of plasmablasts as a consequence of killing their parent cells; plasmablasts do not express CD20. XmAb587 1 is a monoclonal antibody therapy that targets CD19 and enhances FcγRIIb-mediated inhibition—a receptor that inhibits B-cell function. A phase II trial examining the effect of XmAb5871 in IgG4-RD has completed enrolment. Elotuzumab leads to SLAM7-induced antibody directed cellular cytotoxicity in multiple myeloma. The utility of elotuzumab in IgG4-RD is currently only theoretical. Other therapies that may interfere with the pathogenic process are beyond the scope of this article, but could include therapy targeting the BAFF APRIL pathway (belimumab, atacicept); BAFF is critical for B-cell survival. Ag, antigen; APRIL, a proliferation-inducing ligand; BAFF, B-cell activating factor; BCR, B-cell receptor; CXCR5, chemokine receptor type 5; MHC, major histocompatibility complex; TCR, T cell receptor.