Clinically, pulmonary embolism (PE) mostly comes from the lower extremity deep vein system, but if such patients have no evidence of deep venous thrombosis (DVT), other sources of emboli should be considered. It is very rare that embolus comes from the right heart system (in situ thrombosis).[1] Isolated right ventricular noncompaction (iRVNC) can cause PE, but it has not been reported so far. Ventricular noncompaction (VNC) is an unusual cause of cardiomyopathy.[2] The most common site of involvement is the left ventricle, with iRVNC involvement being reported in a few cases.[3],[4] VNC is pathologically characterized by abnormally increased ventricular muscle trabecular-formed deep intra-trabecular crypts, which normally involves in the left ventricular apex while rare in the bi-ventricles or right ventricle.[5] The difference in isolated ventricular noncompaction (iVNC) and VNC lies in that the former only has connection between the deep trabecular crypts and the ventricular cavity, but the latter has connection among the deep trabecular crypts, ventricular cavity, and coronary circulation.[6] Since most iVNC were of isolated left ventricular noncompaction (iLVNC) and iRVNC was reported rarely, it's not clear about the incidence, etiology, clinical manifestations, diagnostic criteria, treatment principles and clinical prognosis, and was easily misdiagnosed and missed. In this case, the patient occurred repeated chest tightness and amaurosis, and confirmed as PE by pulmonary angiography. Right ventricular angiography and cardiac color Doppler ultrasonography confirmed iRVNC, so right ventricular thrombosis was considered as the source of recurrent PE. After long-term anticoagulation, the patient didn't appear chest tightness, amaurosis, or syncope. IRVNC is very rare in clinics, and this disease can form in situ right ventricular thrombosis, thus leading to recurrent PE, so it should cause serious clinical attention.
Patient: male, 55 years old, admitted into the hospital with ‘one-year and 2-month aggravated chest tightness after intermittent activities, accompanied by breathlessness, repeated amaurosis, and syncope' as the main complaint. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
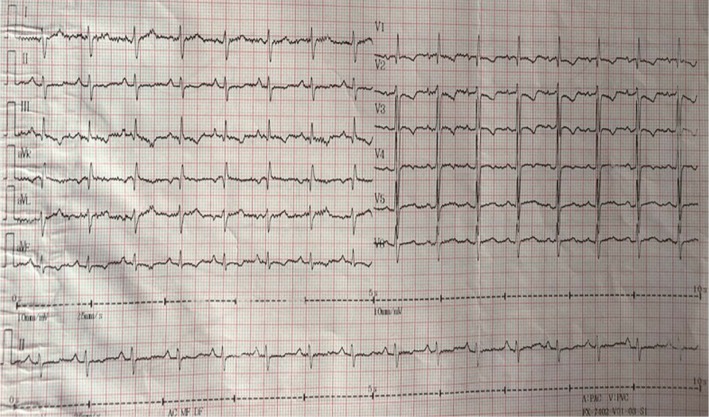
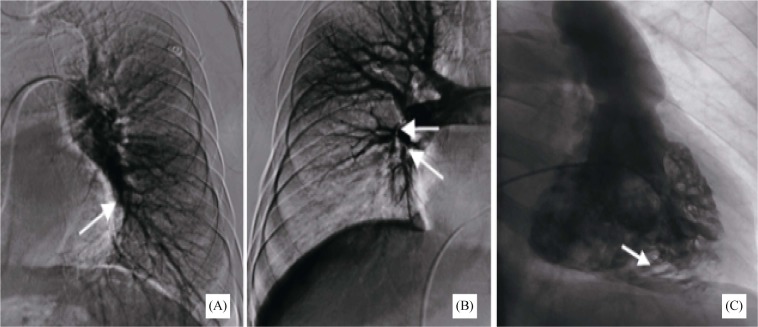
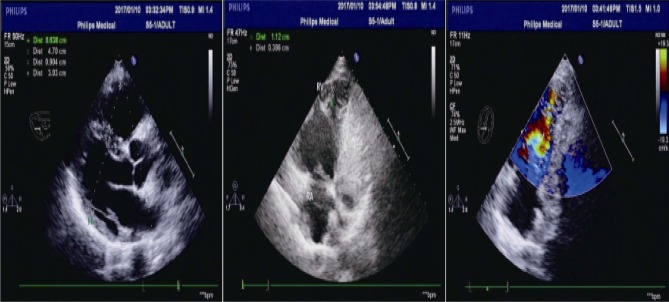
One year ago, the patient felt sudden burst of chest tightness and wheezing with syncope while no chest pain when moving heavy weight; he had been treated in several hospitals: chest computed tomography (CT) showed no obvious abnormality, cardiac ultrasound prompted pulmonary hypertension, together with D-dimer increase. Two months before admission, his symptoms gradually increased, and 50-meter walking can induce wheezing, together with occasional amaurosis; such symptoms repeated, so he came to our hospital for further treatment. The patient had allergic rhinitis for 30 years and hypertension for 10 years, but he denied the history of surgical trauma or family history of heart disease. Physical check on admission: body temperature, 36.5 °C; pulse, 96 beats/min; respiratory, 22 times/min; blood pressure (BP) 110/76 mmHg; the lips appeared cyanosis, and the jugular vein was filling together with negative liver-jugular vein backflow sign (-); His bi-lung breath sounded clear, and the heart beat sounded strong with regular heart rhythm, P2 > A2; valve auscultation did not appear any noise, and the both lower extremities showed no edema. D-dimer 4.50 g/mL (0–0.3 g/mL), blood gas analysis: arterial oxygen partial pressure 61.7 mmHg (75–100 mmHg), arterial carbon dioxide partial pressure 29.1 mmHg (35–45 mmHg), and brain natriuretic peptide 486.30 pg/mL (0–100 pg/mL). Electrocardiogram (ECG): sinus rhythm, SIQIIITIII, TV1-V5 inversion (Figure 1), then PE was considered with the results above. Pulmonary angiography (Figure 2A, B): the left lower pulmonary artery exhibited thrombosis, and the middle and lower lobes of right pulmonary artery occurred occlusion. The main pulmonary artery pressure 81/23/43 mmHg, right pulmonary artery pressure 56/33/41 mmHg, left pulmonary artery pressure 54/31/40 mmHg. It was found the contrast agents flows back to the right ventricle in main pulmonary arteriography and was considered as iRVNC, then the right ventricular angiography was conducted to confirm iRVNC (Figure 2C): the right ventricle was enlarged, and diffuse exercises were weakened, right anterior oblique view (RAO) 30°: the right ventricular anterior wall, lateral wall, and apex had multiple abnormally thick trabecular muscles and deep trabecular crypts, and the crypts exhibited retention of contrast agent in the form of typical feathers. Since there was no abnormality in lower extremity angiography, as well as in coronary angiography and left ventricular angiography, it was thought that iRVNC might lead to PE, then cardiac color Doppler ultrasound was conducted to find if there was any change of the heart (Figure 3): the left atrium was slightly larger (37 mm), the right ventricle was enlarged (right ventricular diameter: 30 mm), the right ventricular apex exhibited multiple trabecular muscles and formed a network structure with the deep crypts. The right ventricular apical myocardium became thinner, the thickness of dense myocardium was about 0.38 cm, and the thickness of reticular myocardium was about 1.1 cm (the thickness of reticular myocardium was about/the thickness of dense myocardium = 2.89), at which site the myocardial exercise amplitude decreased, and blood flow signals can be seen in the crypts; the main pulmonary artery was widened, together with mild tricuspid regurgitation, pulmonary hypertension (mean pulmonary arterial pressure = 69 mmHg), and left ventricular ejection fraction = 59%. After examination, the patient was diagnosed as iRVNC-caused PE, and then was given urokinase (thrombolysis), heparin sodium and warfarin (anticoagulation), angiotensin converting enzyme inhibitors (ACEI), β-receptor inhibitors, and spironolactone so as to improve the cardiac function. The 6-month follow-up revealed no recurrence of chest tightness, suffocation, or post-exercise breathing.
Figure 1. ECG sinus rhythm, SIQIIITIII, TV1-V5 inversion.
Figure 2. Pulmonary and right ventricular angiography.
(A) & (B): Pulmonary angiography: the left lower pulmonary artery exhibits thrombosis (left), and the middle and lower lobes of right pulmonary artery occur occlusion (right); (C): right ventricular angiography: the black part (arrow) is the retention of contrast agent, and the white part is the trabecular muscles.
Figure 3. Cardiac color Doppler ultrasound.
The left atrium and right ventricle were enlarged, the right ventricular apex exhibited multiple trabecular muscles and formed a network structure with the deep crypts, and blood flow signals can be seen in the crypts (arrow).
VNC is a rare congenital cardiomyopathy. It is pathologically characterized by abnormally increased ventricular muscle trabecular-formed deep intra-trabecular crypts, which normally involves in the left ventricular apex while rare in the bi-ventricles or right ventricle, and it can exist solely or be combined with other congenital heart deformities.[7] American Heart Association (AHA) classified VNC as primary hereditary cardiomyopathy in 2006,[8] and European Society of Cardiology (ESC) classified it as undetermined cardiomyopathy in 2008.[9] The difference in iVNC and VNC lies in that the former only has connection between the deep trabecular crypts and the ventricular cavity, but the latter has connection among the deep trabecular crypts, ventricular cavity, and coronary circulation.[5] The prevalence of VNC is about 0.01% in adults and 0.14% in pediatric patients.[10],[11] However, iRVNC was rare and the prevalence was unclear.
The pathogenesis of VNC is not clear yet, and it is generally believed to be caused by the arrest of ventricular compaction in the embryonic period, which may be related to genetic variation, and 12%–50% of patients has a family history and often combine with heart deformity or other hereditary diseases.[12] In the 5th to 8th week of normal fetal development, the ventricle occurs the compaction process from the bottom to the apex and from the epicardium to the endocardium, during which process the ventricular trabecular muscles disappear, the crypts are compressed into the capillaries, and the coronary microcirculation gradually forms, and the failure of this process causes VNC. Kohli, et al.[13] divided VNC into three forms: spongy, grid-like, and simple thickened trabecular muscles, and the patient in this report belongs to the mixed type of the latter two forms.
iRVNC has been rarely reported, so no specific standard for the diagnosis of iRVNC has been proposed so far. Jenni, et al.[14] once proposed four diagnostic criteria of iLVNC, which have been widely used: (1) lacking coexistent cardiac malformation; (2) with typical double-layer-structure ventricular wall, and the inner non-compacted myocardial thickness/outer compacted myocardial thickness at the end-stage of ventricular systolic period > 2; (3) the lesions mainly locate in the apes, lateral wall, and inferior wall; (4) color Doppler ultrasound can measure the blood perfusion in the deep crypts connecting with the heart cavity instead of with the coronary circulation. Due to different anatomical characteristics, iRVNC is more difficultly diagnosed in clinics than iLVNC. ECG, ventricular angiography, computed tomography, and magnetic resonance imaging (MRI) are recommended as the diagnostic models.[7] MRI and ECG have good correlation. The characteristic ECG appears abnormally enlarged trabecular muscles and staggered deep crypts; ECG is convenient, so it's the preferred method of imaging examination. MRI is also helpful in diagnosing this disease (sensitivity 86% and specificity 99%), which can be used for the cases in which ultrasound results are unclear. Ventriculography is rarely reported as a diagnostic tool, and in this report, the patients was found noncompaction of right ventricular myocardium occasionally in main pulmonary artery angiography and the right ventricular angiography showed typical feather-like changes in the right ventricle. The subsequent color Doppler examination confirmed it, and because no other coexistent cardiac abnormality can be found (met the above diagnostic criteria), together with the results of right ventricular angiography, iRVNC was thus confirmed.
VNC has various clinical manifestations and severity degrees, and the age of onset varies from fetus to elderly, can be asymptomatic or progressive heart failure, ventricular arrhythmia, or even sudden death, thromboembolism, or coexistence of a variety of clinical manifestations.[7] One follow-up toward 34 adults with IVNC revealed the clinical manifestations as heart failure (53%), ventricular tachycardia (41%), sudden cardiac death (35%), thromboembolism (24%), and syncope (18%).[10] There were few reports about iRVNC and the manifestation were different. The patient in this report exhibited pulmonary embolism as the first symptom, which is easily mis- or missed-diagnosed in clinics. Pulmonary thrombosis is the most common type of PE, refers to the disease caused the vein system or right heart-blocked pulmonary artery or its branches, and has the main clinical manifestation and pathophysiological characteristics as pulmonary circulation and respiratory dysfunction (accounting for most cases of pulmonary embolism). Deep vein thrombosis is the main source of PE, which mostly occurs in the lower limbs or pelvic deep vein while relatively rare from the right heart system (in situ thrombosis),[1] and no iRVNC caused PE has been reported so far. Oechslin, et al.[10] reported that iVNC caused cardiogenic embolism rate can be as high as 24%, and these events are often independent from the ventricular size and function while closely related to the abnormal heart cavity structures caused crypt and wall-adherent thrombus formation.[15] The patient reported in this study occurred repeated chest tightness and suffocation with syncope, and was diagnosed as PE by pulmonary angiography. Since no thrombus was found in venography in both lower limb varices, it was thought the PE that caused by situ embolus of the right ventricle, led to the pulmonary arterial hypertension.
The treatment principle of VNC is mainly symptomatic treatment, and the patients combined with heart failure can be routinely given drug treatments recommended by the guidelines of heart failure diagnosis and treatment by American College of Cardiology (ACC)/AHA. Regardless of the ventricular size and functional status, all adult VNC cases are recommended long-term anticoagulant therapy so as to prevent thrombosis and PE and to protect further damage in the heart and lungs.[10] This study suggests that the prognosis of iRVNC is not benign, inconsistent with Aggarwal, et al.[16] Although there is no treatment recommendation related to iRVNC, we recommend immediate anticoagulation therapy after diagnosis. The patient in this report was applied long-term oral warfarin anticoagulation therapy together with oral ACEI, β-block inhibitors, and spironolactone simultaneously so as to improve the right heart function. Although this patient has been followed up for 6 months without recurrence of chest distress, suffocated or syncope, but still need long-term follow-up.
VNC has quite different prognoses, varying from long-term asymptomatic to severe cardiac dysfunction, death, or heart transplantation. A study has demonstrated that iLVNC is related to a high incidence of death or heart transplantation.[17] Advanced heart failure, a dilated left heart with systolic dysfunction, reduced systolic blood pressure, pulmonary hypertension, and right bundle branch block can predict adverse outcomes of iLVNC,[17] while the prognosis of iRVNC was not expectable based on the few case reports now.
IRVNC is very rare in clinics, the patients with PE, especially those without significant risk factors or with normal results in lower extremity deep venous system examination, should be considered the possibility of this disease. IRVNC-induced right ventricular thrombosis can lead to chronic recurrent PE or even life-threatening large PE, so PE can be considered as the first diagnostic cause for iRVNC, so serious attention should be given clinically. ECG is the preferred means of examination, as well as cardiac MRI and right ventricular angiography for diagnosis if necessary; otherwise, it's easily mis- or missed-diagnosed, especially in the patients with non-heart-related symptoms (such as PE) as the first symptom.
References
- 1.Konstantindes SV, Torbicki A, Agnelli G, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3303–3069. doi: 10.1093/eurheartj/ehu283. [DOI] [PubMed] [Google Scholar]
- 2.Asfalou I, Boulaamayl S, Baissouni M, et al. Left ventricular noncompaction-A rare form of cardiomyopathy: revelation modes and predictors of mortality in adults through 23 cases. J Saudi Heart Assoc. 2017;29:102–109. doi: 10.1016/j.jsha.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saglam M, Saygin H, Kozan H, et al. Noncompaction of ventricular myocardium involving the right ventricle. Korean Circ J. 2015;45:439–441. doi: 10.4070/kcj.2015.45.5.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choudhary S, Bagarhatta R. Isolated right ventricular non-compaction: a rare form of dilated cardiomyopathy. J Indian Coll Cardiol. 2015;5:98–102. [Google Scholar]
- 5.Rigopoulos A, Rizos IK, Aggeli C, et al. Isolated left ventricular noncompaction: an unclassified cardiomyopathy with severe prognosis in adults. Cardiology. 2002;98:25–32. doi: 10.1159/000064677. [DOI] [PubMed] [Google Scholar]
- 6.Hussein A, Karimianpour A, Collier P, et al. Isolated noncompaction of the left ventricle in adults. J Am Coll Cardiol. 2015;66:578–585. doi: 10.1016/j.jacc.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 7.Weiford BC, Subbarao VD, Mulhern KM, et al. Noncompaction of the ventricular myocardium. Circulation. 2004;109:2965–2971. doi: 10.1161/01.CIR.0000132478.60674.D0. [DOI] [PubMed] [Google Scholar]
- 8.Maron BJ, Towbin JA, Thiene G, et al. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006;113:1807–1816. doi: 10.1161/CIRCULATIONAHA.106.174287. [DOI] [PubMed] [Google Scholar]
- 9.Elliott P, Andersson B, Arbustini E, et al. Classification of the cardiomyopathies: a position statement from the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29:270–276. doi: 10.1093/eurheartj/ehm342. [DOI] [PubMed] [Google Scholar]
- 10.Oechslin EN, Attenhofer Jost CH, Rojas JR, et al. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: a distinct cardiomyopathy with poor prognosis. J Am Coll Cardiol. 2000;36:493–500. doi: 10.1016/s0735-1097(00)00755-5. [DOI] [PubMed] [Google Scholar]
- 11.Pignatelli RH, Mcmahon CJ, Dreyer WJ, et al. Clinical characterization of left ventricular noncompaction in children: a relatively common form of cardiomyopathy. Circulation. 2003;108:2672–2678. doi: 10.1161/01.CIR.0000100664.10777.B8. [DOI] [PubMed] [Google Scholar]
- 12.Murphy RT, Thaman R, Blanes JG, et al. Natural history and familial characteriatics of isolated left ventricular non-compaction. Eur Heart J. 2005;26:187–192. doi: 10.1093/eurheartj/ehi025. [DOI] [PubMed] [Google Scholar]
- 13.Kohli SK, Pantazis AA, Shah JS, et al. Diagnosis of left-ventricular non-compaction in patients with left-ventricular systolic dysfunction: time for a reappraisal of diagnostic criteria? Eur Heart J. 2008;29:89–95. doi: 10.1093/eurheartj/ehm481. [DOI] [PubMed] [Google Scholar]
- 14.Jenni R, Wyss CA, Oechslin EN, et al. Isolated ventricular noncompaction is aassociated with coronary microcirculatory dysfunction. J Am Coll Cardiol. 2002;39:450–454. doi: 10.1016/s0735-1097(01)01765-x. [DOI] [PubMed] [Google Scholar]
- 15.Chin TK, Perloff JK, Williams RG, et al. Isolated noncompaction of left ventricular myocardium. A study of eight cases. Circulation. 1990;82:507–513. doi: 10.1161/01.cir.82.2.507. [DOI] [PubMed] [Google Scholar]
- 16.Aggarwal S, Kalavakunta J, Gupta V, et al. A case of isolated right ventricle noncompaction with ST-elevation chest leads. Heart Views. 2016;17:30–34. doi: 10.4103/1995-705X.182645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tian T, Liu Y, Gao L, et al. Isolated left ventricular noncompaction: clinical profile and prognosis in 106 adult patients. Heart Vessels. 2014;29:645–652. doi: 10.1007/s00380-013-0409-z. [DOI] [PubMed] [Google Scholar]