Abstract
Objective: To examine general practitioners’ (GPs’) perception of their role in emergency medicine and participation in emergency services including ambulance call outs, and the characteristics of the GPs and casualty clinics associated with the GPs’ involvement in emergency medicine.
Design: Cross-sectional online survey.
Setting: General practice.
Subjects: General practitioners in Norway (n = 1002).
Main outcome measures: Proportion of GPs perceiving that they have a large role in emergency medicine, regularly being on call, and the proportion of ambulance callouts with GP participation.
Results: Forty six percent of the GPs indicated that they play a large role in emergency medicine, 63 percent of the GPs were regularly on call, and 28 percent responded that they usually took part in ambulance call outs. Multivariable logistic regression analyses indicated that these outcomes were strongly associated with participation in multidisciplinary training. Furthermore, the main outcomes were associated with traits commonly seen at smaller casualty clinics such as those with an absence of nursing personnel and extra physicians, and based on the distance to the hospital.
Conclusion: Our findings suggest that GPs play an important role in emergency medicine. Multidisciplinary team training may be important for their continued involvement in prehospital emergencies.
Key Points
Health authorities and other stakeholders have raised concerns about general practitioner’s (GPs) participation in emergency medicine, but few have studied opinions and perceptions among the GPs themselves.
• Norwegian GPs report playing a large role in emergency medicine, regularly being on call, and taking part in selected ambulance call outs.
• A higher proportion of GPs who took part in team training perceived themselves as playing a large role in emergency medicine, regularly being on call, and taking part in ambulance call outs.
• These outcomes were also associated with attributes commonly seen at smaller casualty clinics.
Keywords: Primary health care, emergency medical services, out-of-off hours service, general practitioner, Norway, prehospital emergency medicine, casualty clinic
Background
General practitioners (GPs) are involved in emergency medicine in different ways in different countries. They encounter emergency medicine during office hours, outside of office hours, and in both metropolitan and rural areas [1–3]. In some countries, GPs’ involvement both before and after the patient arrives at the hospital is thought to improve patient care and ease the strain on overcrowded emergency departments [4–6]. In Norway, GPs are totally integrated into pre hospital emergency medicine [7] and GP-staffed casualty clinics (out-off-hours emergency primary care services) together with the emergency medical technician (EMT) staff of ambulances are the primary prehospital emergency resources. All GPs in Norway are obliged to be on call at the local casualty clinic, but how often they do this differs between municipalities. The organization and structure of the casualty clinics are heterogeneous because they vary in size, staffing, population served, and area covered. The casualty clinic can serve a single municipality or several municipalities, or a sparsely populated area or a large city. The municipality is responsible for offering its inhabitants a casualty clinic staffed with a physician on call 24 h, 7 days per week, but otherwise the staffing varies from a single physician, with or without a colleague on standby at home, to several physicians working at the same time. Some have no nursing staff, whereas others might have several nurses and other ancillary personnel. Some casualty clinics are equipped with a response vehicle for the physician on duty, with or without a dedicated driver.
In the case of a suspected life-threatening event, severe injury, or disease, the emergency communication center (EMCC) will dispatch an ambulance (an ambulance call out). An alarm will simultaneously be sent to the GP on call at the local casualty clinic. The GP on duty then has to decide whether to leave the casualty clinic and attend to the patient at the site (i.e., take part in the ambulance call out) or let the EMTs take care of the patient by themselves. According to Norwegian legislation, the GP on call is obliged to take part in the ambulance call out whenever it is necessary [7]. A study from 2010 found that GPs take part in half of ambulance call outs [8], and a recent white paper on prehospital emergency medicine in Norway raised the concern that GPs take part in too few ambulance call outs [9]. GPs have described a lack of confidence in emergency medical skills [10], and challenges in the cooperation between GPs and EMTs on ambulance call outs have been reported [11].
Although health authorities and other stakeholders have expressed concerns about GPs’ participation in out-of-hours services, few have studied the opinions and perceptions among the GPs themselves. The aim of this study was to examine the GP’s perception of their own role in emergency medicine, their participation in out-of-hours emergency services and ambulance call outs, and the characteristics of the GPs and the casualty clinics associated with GPs’ involvement in emergency medicine.
Methods
Participants and data collection
In August 2016, all Norwegian GPs registered by the Norwegian Health Economics Administration (HELFO database) (n = 4701) were invited by postal mail to take part in an online survey about Norwegian GPs and emergency medicine. The first invitation was followed up by two reminders, also sent by postal mail. Furthermore, the Norwegian Center of Rural Medicine provided news coverage to urge GPs to participate; the outreach was posted twice on Facebook (11 September and 29 September 2016). We observed that the use of social media was associated with an increase in survey answers. We used Questback as the supplier of the web-based survey.
Questionnaire
We developed the questionnaire based on information from two qualitative studies conducted by MH in 2014 and in 2016. In the first study, we examined the EMTs experiences when working with GPs in emergency medicine [12]. In the second study, we examined rural GPs’ attitudes towards participating in emergency medicine [13]. The survey was piloted on a group of local GPs in Alta, Northern Norway. The survey included questions about the GPs’ perceptions of their own role in emergency medicine, and their participation in out-of-hours services and ambulance call outs. We also included socio-demographic data of the GPs and characteristics of their local casualty clinics. For other purposes (not reported here), we asked the GPs about their confidence in performing emergency procedures, their risk attitude, and whether they would participate in hypothetical ambulance call outs.
Outcome measures
We had three primary outcome measures. The first was to determine to what degree the GPs feel that they play a role in emergency medicine as measured on a Likert scale anchored at 1 (small degree) and 6 (large degree). The second was how often they were on call during the last year. Possible response options were weekly (1), monthly (2), twice (3), once (4), and not at all (5). The third outcome was the proportion of ambulance call outs in which they usually participate. Response options were “not relevant” (1), “never” (2), “25%” (3), “50%” (4), “75%” (5), and “always” (6).
Independent variables
To test for associations between primary outcomes and GP characteristics, we included the independent variables gender, age, patient list size, and if the GP was a specialist. This was done in order to see if more experienced GPs were more involved, and if GPs with fewer patients listed were more involved. To explore associations between casualty clinic characteristics and primary outcomes, we included the type of casualty clinic (municipal, inter-municipal, large city) and location (more or less than a 60-minute drive by car from the nearest hospital). These variables were included to explore whether GP involvement in emergency medicine is mainly a rural phenomenon. Furthermore, we included information about staffing (physicians in the clinic, extra standby physicians at home, nurses), colocation with ambulance services, a dedicated vehicle for the GP, and multidisciplinary team training. These are organizational characteristics thought to make it easier for the GP to work at the casualty clinic and to take part in callouts.
Statistical analysis
Descriptive data of the GPs was presented using means and percentages. We used multivariable logistic regression to explore possible associations between the independent variables and our primary outcome measures. The outcome measures were dichotomized. The GP’s role in emergency medicine was dichotomized into playing a large role (5 and 6) and not playing a large role (1, 2, 3 and 4). Being on call was dichotomized into being on call regularly (1 and 2) and not being on call regularly (3, 4, and 5). Participation in ambulance call outs was dichotomized into usually taking part in call outs (5 and 6) and not usually taking part in call outs (1, 2, 3, and 4). Analyses were done using IBM SPSS Statistics 23. P values <0.05 were considered as statically significant. MH and PH analyzed the data independently.
The study was approved by the Data Protection Official for Research, Norwegian Center for Research Data, which is the privacy ombudsman for all Norwegian Universities.
Results
Of the 4701 GPs invited, 1013 responded. Eleven respondents were excluded from further analyses because they were not GPs, leaving us with a total of 1002 responders. Our sample was fairly representative of Norwegian GPs with respect to age, gender, number of patients on the GPs list and specialist status, although the mean age was slightly younger and the proportion of females was slightly higher. Thirty five percent worked at a clinic covering a single municipality, 50 percent worked at inter municipal clinics, and 15 percent worked at one of four large city clinics; 26 percent of the respondents worked more than one hour’s drive from the nearest hospital. Because about 19 percent of Norwegian GPs work in rural municipalities [14], rural doctors were slightly overrepresented (Table 1).
Table 1.
Characteristics of the respondents.
| Respondents n = 1002 | All Norwegian GPs n = 4701 | |
|---|---|---|
| Mean age, years | 45 | 48 |
| Females | 439/988a (44%) | 41% |
| Mean number of patients on GP list | 1044 | 1128 |
| Specialist | 568/992b (57%) | 53% |
| Rural | 247/965c (26%d) | 19%e |
14 missing answers.
10 missing answers.
37 missing answers.
Rural was defined as over one-hour drive to closest hospital.
Rural defined according to classification of centrality, Statistics Norway.
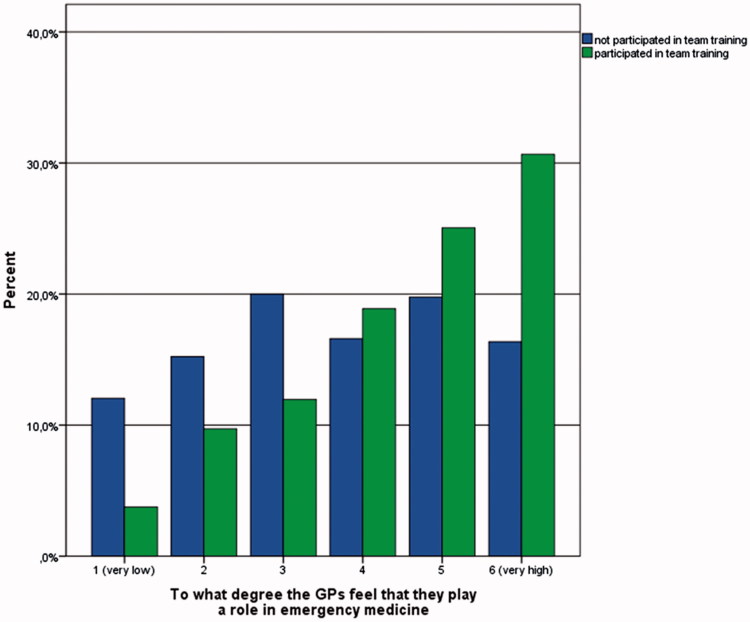
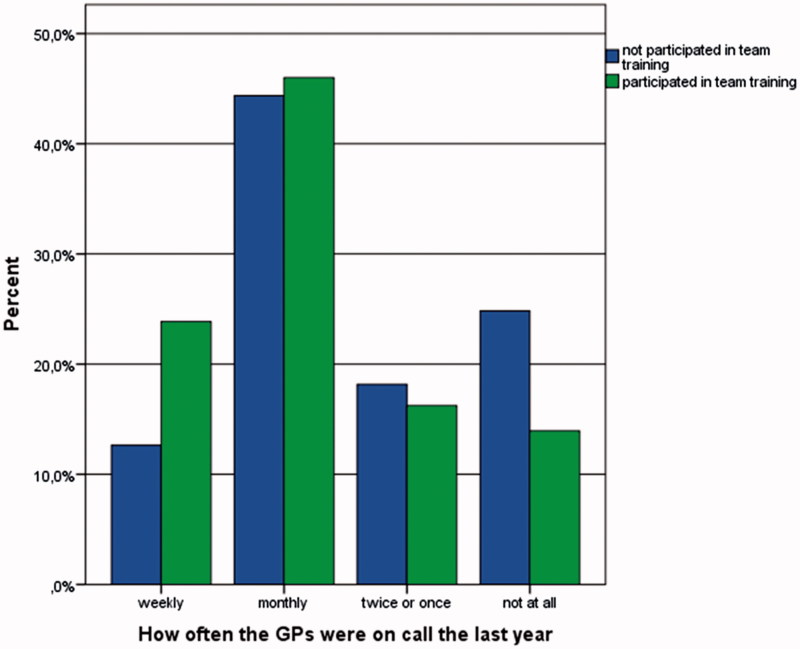
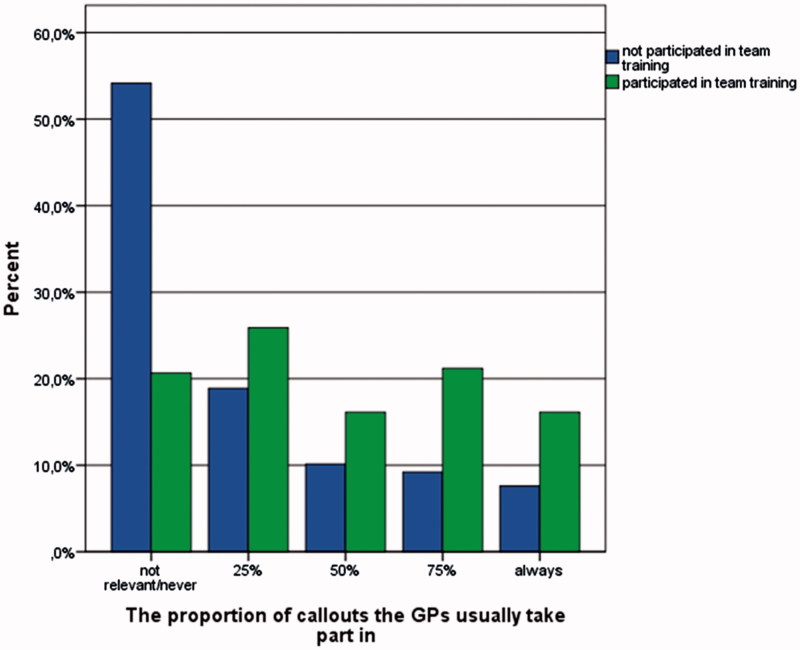
Forty six percent of the GPs indicated that they play a large role (5 or 6 on a scale from 1 = very low to 6 = very high) in emergency medicine (Figure 1), 63 percent were on call regularly (weekly or monthly) (Figure 2), and 28 percent answered that they usually (between 75 and 100 percent of the time) took part in ambulance call outs when asked by the EMCCS (Figure 3, Table 2).
Figure 1.
GPs’ role in emergency medicine.
Figure 2.
Frequency of being on call.
Figure 3:
Participation on call outs.
Table 2.
Multivariable logistic regression analyses: associations between GPs’ perceptions of playing a large role in emergency medicine and casualty clinic characteristics.
| Independent variables | GPs perceiving that they play a large role in emergency medicine | OR crude (95% CI) | OR adjusted (95% CI) |
|---|---|---|---|
| Casualty clinic location | |||
| Municipal | 187/334 (56%) | 2.68a (1.77–4.05) | 1.23 (0.70–2.15) |
| Inter municipal | 221/474 (47%) | 1.84a (1.24–2.73) | 1.24 (0.74–2.06) |
| Large city | 46/143 (32%) | Ref | |
| Are there several GPs at work | |||
| Yes | 94/270 (35%) | Ref | |
| On and off | 97/242 (40%) | 1.25 (0.86–1.73) | 0.93 (0.57-1.51 |
| No | 169/431 (61%) | 2.90a (2.12–3.98) | 1.43 (0.84-2.44) |
| Extra GP on stand by | |||
| Yes | 154/424 (36%) | Ref | |
| No | 294/514 (57%) | 2.34a(1.80–3.05) | 1.38 (0.93–2.04) |
| Co-located ambulance | |||
| Yes | 163/245 (67%) | Ref | |
| No | 290/716 (41%) | 0.82 (0.63–1.07) | 0.80 (0.59–1.08) |
| Dedicated response vehicle | |||
| Yes, with driver | 60/169 (36%) | 0.60a (0.42–0.85) | 1.02 (0.63–1.66) |
| Yes, without driver | 97/163 (60%) | 1.60a (1.12–2.26) | 1.06 (0.71–1.60) |
| No | 294/613 (48%) | Ref | |
| Distance to hospital | |||
| More than 60 minutes | 163/245 (67%) | 2.92a (2.15–3.96) | 1.77a (1.23–2.55) |
| Less than 60 minutes | 290/716 (41%) | Ref | |
| Nursing staff present | |||
| Yes | 303/736 (41%) | Ref | a |
| No | 147/213 (69%) | 3.18a (2.30–4.40) | 1.55a (1.03–2.35) |
| Team training | |||
| Never/not relevant | 159/440 (36.1%) | Ref | |
| Less than annually | 134/259 (52%) | 1.90a (1.39–2.59) | 1.39 (0.98–1.98) |
| Annually | 104/202 (52%) | 1.88a (1.34–2.63) | 1.59a (1.07–2.35) |
| Several times a year | 60/74 (81%) | 7.57a (4.10–13.99) | 4.17a (2.11–8.07) |
Adjusted for gender, age, and specialist status.
p < 0.05.
The perception of playing a large role in emergency medicine was associated with working a long distance from the hospital (adjusted odds ratio [OR] 1.77, 95% confidence interval [CI] 1.23–2.55), working with no nursing staff (adjusted OR 1.55, 95% CI 1.03–2.35), and with taking part in team training once a year (adjusted OR 1.59, 95% CI 1.07–2.35) or more often than once a year (adjusted OR 4.17, 95% CI 2.11–8.07) (Table 3).
Table 3.
Multivariable logistic regression analyses: associations between being on call regularly and casualty clinic characteristics.
| Independent variables | Being on call regularly | OR crude (95% CI) | OR adjusted (95% CI) |
|---|---|---|---|
| Casualty clinic location | |||
| Municipal | 226/327 (69%) | 2.47a (1.65–3.70) | 0.81 (0.45–1.46) |
| Inter municipal | 320/464 (69%) | 2.45a (1.67–3.59) | 1.42 (0.84–2.41) |
| Large city | 68/143 (48%) | Ref | |
| Are there several GPs at work | |||
| Yes | 128/263 (49%) | Ref | |
| On and off | 159/237 (67%) | 2.15a (1.50–3.09) | 2.04a (1.21–3.43) |
| No | 323/426 (76%) | 3.31a (2.38–4.60) | 1.86a (1.04–3.34) |
| Extra GP on stand by | |||
| Yes | 213/414 (56%) | Ref | |
| No | 377/507 (74%) | 2.30a (1.74–3.03) | 1.45 (0.95–2.25) |
| Co-located ambulance | |||
| Yes | 229/351 (65%) | Ref | |
| No | 378/565 (67%) | 1.08 (0.81–1.43) | 1.01 (0.71–1.41) |
| Dedicated response vehicle | |||
| Yes, with driver | 84/164 (51%) | 0.50a (0.35–0.71) | 1.02 (0.62–1.70) |
| Yes, without driver | 121/160 (76%) | 1.48 (0.99–2.01) | 0.99 (0.61–1.59) |
| No | 409/604 (68%) | Ref | |
| Distance to hospital | |||
| More than 60 minutes | 179/242 (74%) | 1.83a (1.33–2.54) | 1.18 (0.77–1.81) |
| Less than 60 minutes | 426/701 (61%) | Ref | |
| Nursing staff present | |||
| Yes | 432/724 (60%) | Ref | Ref |
| No | 177/210 (85%) | 3.63a (2.43–5.41) | 3.06a (1.77–5.29) |
| Team training | |||
| Never/not relevant | 248/435 (57%) | Ref | |
| Less than annually | 177/256 (70%) | 1.69a (1.22–2.34) | 1.26(0.85-1.88) |
| Annually | 130/193 (67%) | 1.56a (1.09–2.22) | 1.72a (1.10–2.69) |
| Several times a year | 59/75 (79%) | 2.78a (1.55–4.99) | 2.71a (1.22–6.05) |
Adjusted for gender, age, and specialist status.
p < 0.05.
Being on call regularly was associated with working at a casualty clinic staffed with only one physician at all times (adjusted OR 1.86, 95% CI 1.21–3.43) or one staffed with only one physician part of the time (adjusted OR 1.86, 95% CI 1.04–3.34), working at a casualty clinic with no nursing staff (OR 3.06, OR 1.77–5.29), and with taking part in team training once a year (adjusted OR 1.72, 95% CI 1.10–2.69) or more often than once a year (adjusted OR 2.71, 95% CI 1.22–6.05) (Table 4).
Table 4.
Multivariable logistic regression analysis: associations between usually taking part in ambulance call outs and casualty clinic characteristics.
| Independent variables | GPs usually taking part in ambulance call outs | OR crude (95% CI) | OR adjusted (95%CI) |
|---|---|---|---|
| Casualty clinic location | |||
| Municipal | 141/330 (43%) | 3.83a (2.33–6.92) | 2.69a (1.36–5.32) |
| Inter municipal | 106/473 (22%) | 1.48 (0.90–2.43) | 1.52 (0.80–2.91) |
| Large city | 23/141 (16%) | Ref | |
| Are there several GPs at work | |||
| Yes | 54/269 (20%) | Ref | |
| On and off | 367240 (15%) | 0.70 (0.44–1.12) | 0.64 (0.34–1.20) |
| No | 178/428 (42%) | 2.84 (1.20–4.04) | 1.24 (0.66–2.35) |
| Extra GP on stand by | |||
| Yes | 74/422 (18%) | Ref | |
| No | 194/511 (38%) | 2.88a (2.12–3.92) | 1.80a (1.11–2.91) |
| Co-located ambulance | |||
| Yes | 112/357 (31%) | Ref | |
| No | 157/570 (28%) | 0.83 (0.62–1.11) | 0.77 (0.55–1.10) |
| Dedicated response vehicle | |||
| Yes, with driver | 44/168 (26%) | 0.96 (0.65–1.42) | 1.85 (1.05–3.26) |
| Yes, without driver | 63/163 (38%) | 1.71a (1.19–2.46) | 1.13 (0.73–1.75) |
| No | 164/609 (27%) | Ref | |
| Distance to hospital | |||
| More than 60 minutes | 98/245 (40%) | 2.14a (1.57–2.91) | 1.17 (0.89–1.73) |
| Less than 60 minutes | 168/707 (24%) | Ref | |
| Nursing staff present | |||
| Yes | 168/729 (23%) | Ref | |
| No | 103/214 (48%) | 3.10a (2.25–4.26) | 1.62a (1.06–2.47) |
| Team training | |||
| Never/not relevant | 73/434 (17%) | Ref | |
| Less than annually | 78/257 (30%) | 2.16a (1.50–3.11) | 1.61a (1.07–2.44) |
| Annually | 82/200 (41%) | 3.44a (2.35–5.01) | 2.77a (1.77–4.31) |
| Several times a year | 39/76 (51%) | 5.21a (3.11–8.73) | 3.84a (2.11–6.98) |
Adjusted for gender, age, and specialist status.
p < 0.05.
Taking part in ambulance call outs when alerted by the EMCC was associated with working in a municipal casualty clinic (adjusted OR 2.69, 95% CI 1.36–5.32), working without a GP on standby (adjusted OR 1.80, 95% CI 1.11–2.91), working with no nursing staff (OR 1.62, 95% CI 1.06-2.47), and with taking part in team training less than once per year (adjusted OR 1.61, 95% CI 1.07–2.44), at least once per year (adjusted OR 2.77, 95% CI 1.77–4.31), or more often than once per year (adjusted OR 3.84, 95% CI 2.11–6.98).
Discussion
Half of the GPs who responded to our survey reported that they play a large role in emergency medicine, two thirds were regularly on call, and one third usually took part in ambulance call outs. Playing a large role, regularly being on call, and taking part in ambulance call outs were all strongly associated with multidisciplinary training. These outcomes were also associated with attributes commonly seen at smaller casualty clinics.
Comparison with previous studies
Norwegian studies have shown that GPs play a part in local emergency medicine and improve patient care by participating in call outs [12,13,15]. In 2013, R⊘rtveit found that the EMCC has problems with over and under triage, and having a GP on the scene was suggested as a solution to this challenge [16]. A recent study from England also found that involving GPs improved prehospital treatment by providing better treatment and reducing the number of patients who were admitted to hospital [17]. Despite reporting having a large role in local emergency medicine, the GPs in our survey reported that they only took part in a select number of ambulance call outs. In a previous study, GPs reported being involved in emergency medicine in other ways such as by phone or seeing the patient at the casualty clinic, not by only taking part in ambulance call outs, possibly explaining this contradiction [13].
Taking part in training exercises with other local emergency staff was strongly associated with all of our primary outcome measures. There can be several reasons for this association, and our method cannot be used to prove a causal relationship between training exercises and GP involvement. We speculate that training might lead to knowledge, acquaintances and confidence leading to involvement in emergency medicine. A different interpretation might be that GPs that are involved in emergency medicine tend to take part in training exercises, and that the GPs that are less involved avoid taking part in training exercises. Training medical teams by simulation improves quality by reducing complications and mortality [18]. It is also an arena for learning, resulting in social and structural improvements [19]. Training based on simulation is associated with role clarity, role confidence, and feeling in control [20,21]. Norwegian EMTs want to take part in regular exercises with GPs from the casualty clinics [13], and training in cooperation and interaction between the different branches in emergency medicine is mandatory in Norway [7]. However, only 28 percent of the GPs in our survey reported that they participated annually in this type of training, and only half of Norwegian casualty clinics have annual training sessions [22]. Our findings suggest that annual training exercises could improve the GP’s involvement in local emergency medicine.
Working at a long distance from the nearest hospital and working without a nursing staff was associated with a perception of having a large role in emergency medicine. This result was expected since the GPs in these areas must be able to perform emergency medicine by themselves over a long period of time. We anticipated that the availability of nurses and more physicians on call or on standby would be associated with working at the clinic more often and taking part in more ambulance call outs, but we found the opposite result. The reasons for this could be that the absence of these resources is more commonly represented at smaller, rural casualty clinics. These clinics may not necessarily be located more than a one hour car drive away from the hospital. Furthermore, other attributes of rural medicine than the distance from hospitals may be important for GP involvement in emergency medicine. Unfortunately, we are unable to account for such attributes, since we did not collect pertinent data. Fewer GPs work in areas with small casualty clinics such that each GP has to be on call more frequently. GPs working in small rural areas also want to participate in ambulance call outs in order to maintain their skills and improve patient care [13]. It is therefore likely that working at a small casualty clinic is associated with playing a large role in emergency medicine, being on call, and taking part in ambulance call outs.
Strengths and limitations
The main strengths of the study were the large sample size and that our questionnaire, even if not formally validated, was based on qualitative studies among GPs (i.e. our target population). There are also some limitations to our study. First, we used social media to encourage GPs to participate in the survey. This may have led to selection bias because use of social media is more common among younger people and women [23]. This phenomenon might explain why the age in our sample is three years younger than the average age of GPs in Norway and why the proportion of women was larger. Because the study was endorsed by the Norwegian Center in Rural Medicine, we might also have an overrepresentation of rural doctors in our sample. Caution must be used when comparing the GPs in the survey working in rural areas with the national data, as the survey uses another definition than used by Statistics Norway. Second, our data were based on what the GPs reported and not actual observations. This makes our study prone to social desirability bias [24]. It is also a limitation to the study design that the causal relationship between the three outcomes variables cannot be examined. Third, our responders only represent 21 percent of all Norwegian GPs; therefore, caution should be used when transferring these results to the general population of GPs in Norway. Even though a higher rate of participation would have been desirable, it is well documented that physicians respond to requests for participation in such studies at a lower rate than the general population [25].
Conclusion
Our findings suggest that GPs play an important role in emergency medicine. Multidisciplinary team training may be important for their continued involvement in prehospital emergencies.
Funding Statement
Magnus Hjortdahl was funded by the Norwegian Research Fund for General Practice. This work was also supported by the Norwegian Center of Rural Medicine.
Acknowledgements
We wish to thank the Norwegian Center of Rural Medicine for the news coverage about the project. The authors also thank the GPs who took part in this study.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Notes on contributors
Magnus Hjortdahl is a GP in training and PhD student at UiT - The Artic University of Norway. His research interest is GP’s role in pre hospital emergency medicine.
Erik Zakariassen is a nurse, Phd and Associate Professor at the University of Bergen, and a researcher at National Centre for Emergency Primary Health care, UNI Health. His research interest is the prehospital emergency system.
Peder A. Halvorsen is a practicing GP, PhD and part time Professor in general practice at UiT - the Arctic University of Norway. His research interests are medical decision making, public health and rural medicine.
References
- 1.Mole J, McGuire D, Riely R, et al. . Are Perth metropolitan GPs prepared for common emergencies? Aust Fam Phys. 2006;35:553–554. [PubMed] [Google Scholar]
- 2.Liddy C, Dreise H, Gaboury I.. Frequency of in-office emergencies in primary care. Can Fam Phys. 2009;55:1004–1005. [PMC free article] [PubMed] [Google Scholar]
- 3.Bondevik GT.Norsk legevakt i et internasjonalt perspektiv [Norwegian Emergency Primary Health Care in an international perspective] In: Hansen EH, Hunskår S, editors. Legevaktarbeid En innføringsbok for leger og sykepleiere [An introduction to Emergency Primary Health Care]. Oslo: Gyldendal Norsk Forlag AS; 2016. p. 31–36 [Google Scholar]
- 4.Porter KM.Training doctors in prehospital care: the West Midlands (UK) approach. Emerg Med J. 2004;21:509–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy AW, Bury G, Plunkett PK, et al. . Randomized controlled trial of general practitioner versus usual medical care in an urban accident and emergency department: process, outcome, and comparative cost. Bmj. 1996;312:1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larsson G, Holmén A, Ziegert K.. Early prehospital assessment of non-urgent patients and outcomes at the appropriate level of care: A prospective exploratory study. Int Emerg Nurs. 2017;32:45–49. [DOI] [PubMed] [Google Scholar]
- 7.The Ministry of Health and Care Services Regulation on pre-hospital emergency medicine services; 2015. [Internet]; [cited 2017 Aug 17]. Available from: https://lovdata.no/dokument/SF/forskrift/2015-03-20-231?q=akuttmedisinforskriften. [Google Scholar]
- 8.Zakariassen E, Hunskaar S.. Involvement in emergency situations by primary care doctors on-call in Norway – a prospective population-based observational study. BMC Emerg Med. 2010;10:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Ministry of Health and Care Services Først og fremst — Et helhetlig system for håndtering av akutte sykdommer og skader utenfor sykehus [First and foremost – a complete system for managing the care of acute illness and injuries outside hospitals]. Official Norwegian Report NOU 2015; 17:2015. [Google Scholar]
- 10.Wisborg T, Brattebø G.. Confidence and experience in emergency medical procedures. Norwegian general practitioners. Scand J Prim Health Care. 2001;19:99–100. [DOI] [PubMed] [Google Scholar]
- 11.Forland O, Zakariassen E, Hunskar S.. Samhandling mellom ambulansearbeider og legevaktlege [Cooperation between ambulance personnel and regular general practitioners.]. Tidsskr Laegeforen. 2009;129:1109–1111. [DOI] [PubMed] [Google Scholar]
- 12.Hjortdahl M, Zakariassen E, Wisborg T.. The role of general practitioners in the pre hospital setting, as experienced by emergency medicine technicians: a qualitative study. Scand J Trauma Resusc Emerg Med. 2014;22:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hjortdahl M, Halvorsen P, Risø MB.. Rural GPs’ attitudes toward participating in emergency medicine: a qualitative study. Scand J Prim Health Care. 2016;34:377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.StatBank Norway [Internet]. Statistics Norway 2015 [cited 2017 Aug 17] Available from: https://www.ssb.no/en/statistikkbanken [Google Scholar]
- 15.Rortveit S, Hunskar S.. Akuttmedisinsk handsaming i ein utkantkommune. [Management of emergency medical events in a rural community]. Tidsskr Laegeforen. 2009;129:735–737. [DOI] [PubMed] [Google Scholar]
- 16.Rortveit S, Meland E, Hunskaar S.. Changes of triage by GPs during the course of prehospital emergency situations in a Norwegian rural community. Scand J Trauma Resusc Emerg Med. 2013;21:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villareal M, Leach J, Ngianga-Bakwin K, et al. . Can a partnership between general Practitioners and ambulance services reduce conveyance to emergency care? Emerg Med J. 2017;34:459–465. [DOI] [PubMed] [Google Scholar]
- 18.Haerkens MH, Knox M, Lemson J, et al. . Crew Resource Management in the Intensive Care Unit: a prospective 3-year cohort study. Acta Anaesthesiol Scand. 2015;59:1319–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brandstorp H, Halvorsen PA, Sterud B, et al. . Primary care emergency team training in situ means learning in real context. Scand J Prim Health Care. 2016;34:295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Utsi R, Brandstorp H, Johansen K, et al. . Tverrfaglig akuttmedisinsk teamtrening i kommunehelsetjenesten [Training in multiprofessional emergency medicine in primary health care]. Tidsskr Laegeforen. 2008;128:1057–1059. [PubMed] [Google Scholar]
- 21.Pedersen MJ, Gjerland A, Rund BR, et al. . Emergency preparedness and role clarity among rescue workers during the terror attacks in Norway July 22, 2011. PLoS One. 2016;11:e0156536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morken T, Myhr K, Raknes G, et al. Legevaktorganise-ring i Norge. Rapport fra Nasjonalt legevaktregister 2016 [The organization of emergency primary health care in Norway. Research report 2016]. National Centre for Emergency Primary Health Care, 2016. [Google Scholar]
- 23.Use of social media in Norway Q4, 2016. [internet] Ipsos [cited 2017 Aug 17] Available from: https://www.ipsos.com/nb-no/ipsos-tracker-om-sosiale-medier-q416 [Google Scholar]
- 24.Althubaiti A.Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson PT.Why physicians do not respond Chapter 20.2. In: Handbook of health survey methods. Neywork: Wiley; 2014. p. 517 [Google Scholar]