Fig. 1.
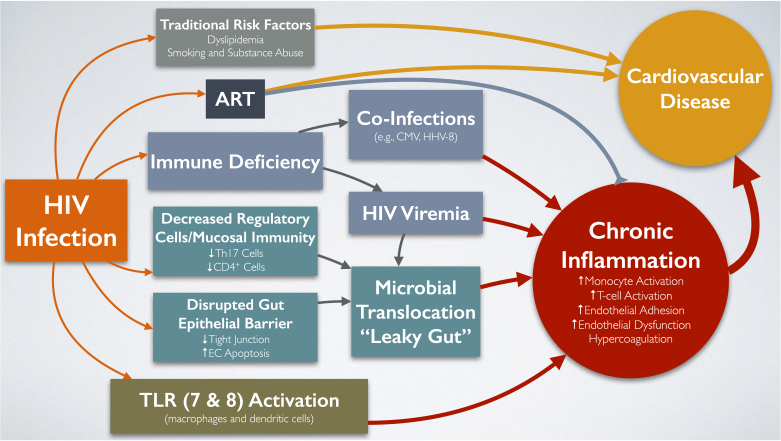
Current paradigm of mechanisms involved in increased risk of cardiovascular disease among people living with HIV. HIV infection results in the emergence of several factors that increase cardiovascular disease (CVD) risk. Traditional CVD risk factors such as dyslipidemia, smoking, high blood pressure, and substance abuse contribute to higher CVD risk in people living with HIV (PLWH). Some antiretroviral therapies (ARTs) have been directly and indirectly (via traditional risk factors) associated with CVD risk, particularly abacavir and protease inhibitors (PIs). Chronic inflammation, in the form of increased monocyte and T cell activation, endothelial adhesion, and dysfunction and hypercoagulation, has been significantly associated with increased CVD in the general population and is more aggravated in PLWH due to (1) HIV-associated immune deficiency leading to coinfections with pathogens such as cytomegalovirus (CMV) and human herpesvirus-8 (HHV-8) that increase chronic inflammation; (2) subclinical viremia also leads to higher inflammation; (3) microbial translocation, or “leaky gut,” characterized by decreased regulatory cells and mucosal immunity (lower Th17 and CD4+ cells), disrupted gut epithelial barrier (less tight junctions and higher endothelial cell (EC) apoptosis), and persistent presence of the HIV virus in the gut; and (4) toll-like receptor (TLR) 7 and 8 activation in macrophages and dendritic cells. Early initiation and sustained use of ART has been shown to decrease chronic inflammation in PLWH
