Summary
Objective
Colorectal cancer (CRC) is the third most common cancer among adults in Iran. CRC screening is an effective way in reducing mortality rate from this cancer. However, the screening rate of CRC is very low among Iranian adults. This study investigated predictors of Iranian average-risk adults ‘ intention to take up CRC screening with fecal occult blood test using a mediator model.
Methods
Participants of this cross-sectional study comprised of 477 average-risk adults who were selected using a national sampling frame in Hamadan city, west of Iran. Data was collected through the questionnaire based on the preventive health model constructs. Structural Equation Modeling (SEM) was employed to test the relationship using Smart PLS 2.0 software
Results
All measures were robust in terms of the reliability and validity. Benefit (b = 0.12, p < 0.01), self- efficacy (b = 0.36, p < 0.01), social support (b = 0.10, p < 0.05) and barriers (b = -0.14, p < 0.01) predicted the intention to be screened for CRC. Self- efficacy partly mediated the effects of social support and perceived barriers on intention. The study model explained approximately 24% of the variance in CRC screening intention with fecal occult blood test
Conclusion
Our findings indicated that the preventive health model constructs such as self -efficacy, social support and barriers are useful in understanding CRC screening intentions and can help health planners to develop effective interventions to encourage Iranian adults to undergo CRC screening.
Keywords: Colorectal neoplasms, Preventive health model, Iran
Introduction
Colorectal cancer (CRC), with 1.36 million diagnoses and 694,000 deaths in 2012, is the third most common cancer in adults worldwide [1]. In the Islamic Republic of Iran, after stomach and breast cancers, CRC is the third most common cancer in both genders [2]. Because of the slow progression of the CRC, this disease is highly curable in its earlier stage and screening can reduce the incidence and mortality of CRC [3, 4]. However, due to lack of screening programs in many countries including Iran, only 39% of CRC are diagnosed at the early stage [5]. Routine screening for CRC is recommended starting at age 50 years for men and women at average risk [4, 6]. The trend of cancer occurrence is observed in younger than 40 years of age in Iran [7] Hence, for this setting, it seems that beginning regular screening at age less than 50 is a more conservative approach.
Several screening modalities are available, including fecal occult blood testing (FOBT), multitarget stool DNA, flexible sigmoidoscopy (FS), colonoscopy, barium enema and CT colonography [6].
FOBT is the first option for CRC screening in countries with restricted resources [8]. Economic evaluations have indicated that FOBT is a cost-effective method of screening compared to FS or colonoscopy in average-risk individuals [9, 10].
At the time of the study (2015), there were no national screening programs for CRC in Iran. Guidelines for the early detection and screening of CRC were approved by the CRC Task Force in 2016. In this program, people aged 50-69 years are called and evaluated by health care providers. Then, Fecal Immunochemical Test (FIT or iFOBT) should be done. Patients refer to the doctor with positive family history or abnormal FIT. Since 2016, this program has been implemented in pilot form in four cities of Iran, but it has not yet become a regular national screening program.
The low screening rates in some countries [11, 12], as well as in Iran [13], highlight the necessity to recognize the factors that predict screening behavior and intention, and eventually to design effective interventions to undergo screening [14]. Evidence suggests that the psychosocial and cognitional factors such as attitudes and self-efficacy are important because they are more modifiable factors than others affecting the at-risk population’s healthy behavior [13, 15]. Identifying the socio-cognitive models of health behavior offers significant perceptions into the types of factors that affect a person’s decision to use screening tests [16].
In the health promotion and disease prevention literature, including cancer preventive behaviors, intention has been considered as the most powerful predictor of person’s engagement in a given health behavior [17, 18]. Preventive Health model (PHM) (Fig. 1), which combines elements from the health belief model [19], the theory of reasoned action [20] and social learning theory [21], suggests that intention is affected by four series of factors including background factors, cognitive and psychosocial constructs (e.g., perceived susceptibility to disease and perceived barriers), social support and influence, and program factors (e.g., interventions by health providers) [22]. This model has been applied to predict intention and behavior for CRC screening [18, 23]. The framework has been also used to design interventions and strategies to improve screening uptake [24].
Fig. 1.
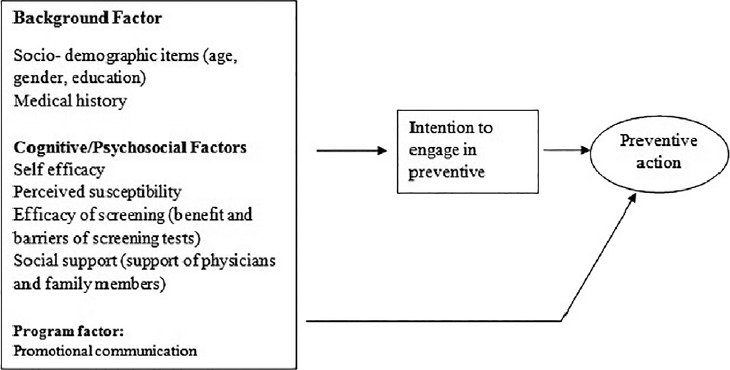
Conceptual framework of preventive health model.
In health behavior literature, self-efficacy has been consistently mentioned as one of the strongest determinants of intention and/or behavior in a range of health behaviors [25]. Self-efficacy is a feeling an individual has so that he or she can successfully engage in a behavior in a particular situation with known outcomes. Given that self-efficacy has been frequently cited as one of the strongest predictors of intention/ health behavior, it is important to examine whether it mediates the effect of other psychosocial determinants of intention to undergo CRC screening. In this study we examined mediating effects of self-efficacy on the association between two constructs of PHM (i.e., social support and perceived barriers) and intention to adhere to CRC.
Social support having been conceptualized in a variety of ways, may facilitate intention/ behavior directly through providing a stress-buffering effect. On the other hand, some previous investigations suggested that self-efficacy at least acts as a partial mediator of this relationship [26, 27]. For example, Gage reported that self-efficacy was the partial mediator of the relationship between social support and health practices [26]. Similar to social support, in conceptual frameworks such as PHM, it is assumed that a perceived barrier has a direct effect on intention. However, some investigators have tested pathways between barriers and different constructs including self-efficacy [28, 29]. The literature, however, shows mixed findings on the mediating effects of self-efficacy. For example, results of Hill and Startup study did not support the mediational role of self-efficacy [30]. Studies on psychosocial factors -associated with CRC screening abound in the literature [13, 31]. The aim of the study was twofold: (1) to identify the determinants of Iranian average-risk adults ‘ intention to take up CRC screening (FOBT), and (2) to examine whether self-efficacy would mediate the effects of social support and barrier on intention to take up CRC screening (FOBT).
Methods
SETTING AND STUDY DESIGN
This cross-sectional study was conducted on 480 average-risk adults in Hamadan city, the capital of Hamadan province, in 2015 with a population about 600000, placed in the west of Iran. The population over 40 years old is 171648 people [32].
Participants were recruited using cluster random sampling. A total of 20 clusters were randomly selected from Multiple Indicator Demographic and Health Survey (IrMIDHS-2010) [33]. Sample size of Hamadan province in IrMIDHS consisted of 74 clusters (urban cluster = 44, rural cluster =30). In current study, we selected 20 clusters among 24 urban clusters of Hamadan city (the capital of the province). Then, in each cluster, one house was selected as a starting point or ‘Cluster Head’ and moved to the right direction of each cluster head, 24 people above 40 years were entered into the study. Participants were eligible for the study if they were 40 years or older, had no history of CRC and polyp, and had mental ability to respond the questions. Data were collected by four trained senior public health students via face to face interviews. Two women and one man were excluded from the study due to imperfect or apathetic responses.
This study was approved by ethics committee of Hamadan University of Medical Sciences. The participants were given information about the purpose of the study and individual informed consent was obtained from interested individuals.
MEASURES
The survey instrument was generated by the literature review [13, 34, 35] and qualitative data were collected through 10 focus group interviews (61 persons) and 20 individual interviews with adults 40 years and older (results of this part of the study are reported elsewhere). Briefly, the results of the individual and group interviews indicated that several factors were associated with CRC screening, including awareness and knowledge about CRC and its screening, financial problems, low priority of health concerns, fear of detection of cancer, mistrust in the health care system and problems related to the nature of CRC screening tests.
The interviews permitted the researcher to hear the participants talk about CRC screening in their own words. The participants’ own words and statements from interviews helped to build survey questions.
At the beginning of the research, a pilot study was administered to 30 adults from the people of interest to acquire feedback about understandability, time of completion, reliability and face validity of the items. Also, content validity of questionnaire was confirmed by health education and promotion experts (n = 9) and gastroenterologist (n = 1).
The questionnaire contained two parts: The first part assessed demographic characteristics of the participants including age, sex, educational level, marital status, employment, medical insurance, and family history of CRC or polyps. The second part measured six constructs of the preventive health model as follows.
Perceived susceptibility: perceived susceptibility toward CRC was assessed using four items (e.g., “Compared with persons at my age, it is less likely that I will develop CRC”). The items were rated on a 5-point Likert scale ranging from strongly disagree = 1 to strongly agree = 5. Three items were reverse coded during data analysis in order that higher scores on this items reflected more positive susceptibility participants (Cronbach’s alpha = 0.73).
Perceived benefit: Perceived benefit to CRC screening was assessed using three items. A sample item is “If I have FOBT, I can prevent the disease progression”. The items were rated on a 5-point Likert scale ranging from strongly disagree = 1 to strongly agree = 5 (Cronbach’s alpha = 0.70).
Perceived barriers: Perceived barriers toward CRC screening was measured by seven items (e.g., “Having the FOBT test will be unpleasant and hard to me”). The items were rated on a 5-point Likert scale ranging from strongly disagree = 1 to strongly agree = 5 (Cronbach’s alpha = 0.75).
Social support: Social support toward CRC screening was measured by three items (e.g., “My family encourages me to have the FOBT”). The items were rated on a 5-point Likert scale ranging from strongly disagree =1 to strongly agree = 5.
Self -efficacy: Self-efficacy toward CRC screening was assessed using seven items. For example (“I can have FOBT, although it is unpleasant”). A 5-point Likert scale was employed for the items (Cronbach’s alpha = 0.81).
Intention: Intention to be screened for CRC was measured through three items (e.g., “I intend to have a FOBT (CRC screening) in the next year”). The items were rated on a 5-point Likert scale ranging from strongly disagree = 1 to strongly agree = 5 (Cronbach’s alpha = 0.74).
The third part assessed factor program using one item. The item was rated on a 5-point Likert scale ranging from strongly disagree = 1 to strongly agree = 5.The interview lasted nearly 15 min to complete the questionnaire.
DATA ANALYSIS
Structural Equation Modeling (SEM) [36] was used to assess the adequacy of PHM to explain average-risk adult’s intentions to undergo screening (FOBT) for CRC. SEM is a combination of two models: (1) a measurement model or outer model (relating observed variables to latent variables), (2) a structural model or inner model (relating latent variables to other latent variables). SmartPLS 2.0 software was employed for SEM analysis [37]. In the current study, our decision to select PLS was due to the existence of formative construct (Social support) [38].
Construct validity and reliability could be assessed through a number of indices such as factor loadings, cross-loadings, average variance extracted (AVE), composite reliability and Cronbach’s alpha. In addition, two important criteria, the level of the path coefficient and the significance of the path coefficient were utilized to measure the power of the relationship between latent variables in structural models. The predictive power of the model was examined by calculating Q2 indexes of intention. Finally, a goodness of fit (GoF) index was calculated to display the model fit to the data. Furthermore, the results of the descriptive data were acquired with SPSS version 20.
Results
The data were gathered from 477 adults (271 females and 206 males). Mean age (sd) of the adults was 53.63 (10.27) years (range 40-82). The majority of participants had high school or lower degrees and most were married (86.4%). Other demographic variables are demonstrated in Table I.
Tab. I.
Demographics characteristics of survey participants (N = 477).
| Characteristics | N (%) |
|---|---|
| Gender Female Men |
271 (56.8) 206 (43.2) |
| Occupation Housekeeper Employee Retired Unemployed |
235 (49.3) 156 (32.7) 72 (15.1) 14 (2.9) |
| Marital status Single Married Divorced/widow non-response |
12 (2.5) 402 (86.4) 52 (10.9) 1 (0.2) |
| Education illiterate Lower High school High school Higher education non-response |
79 (16.6) 228 (47.8) 95 (19.9) 73 (15.3) 2 (0.4) |
| Health insurance Yes No |
376 (78.8) 101 (21.2) |
| Family history of colorectal cancer/polyps Yes No Non-response |
34 (7.1) 442 (92.7) 1 (0.2) |
| Prior screening Yes No |
19(4) 458(96) |
MEASUREMENT MODEL RESULTS
The initial assessment of the measurement model for reflective constructs (susceptibility, benefit, barrier, self-efficacy and intention) displayed that 5 indicators of the constructs were deleted from the data set because of outer loading value lower than 0.6, recommended by Chin [39].After deletion of the items, all the outer loadings exceed 0.6 for further analyses (p < 0.05).
For the five reflective constructs, the Cronbach’s alpha ranged from 0.70 to 0.92, exceeding the recommended threshold value of 0.70 [40]. Composite reliability ranged from 0.81 to 0.95, exceeding the recommended threshold value of 0.70 [38]. And communality ranged from 0.51 to 0.86, exceeding the recommended threshold value of 0.50. Additionally, average variance extracted (AVE) for each reflective construct was 0.50 and higher, meaning that latent variable explains more than 50% of its indicator variance, indicating acceptable convergent validity [38].
The loading factors for the items on each construct were higher than loadings with all the remaining constructs (the cross-loadings), and the AVE squared root of any construct was higher than its correlation values with other constructs (Fornell and Larcker test) [38]. These results support discriminant validity at the latent variables level (Tab. II).
Tab. II.
Discriminate validity of Constructs-Fornell-Larcker criterion.
| Variable | Barriers | Benefit | Intention | Self efficacy | Susceptibility |
|---|---|---|---|---|---|
| Barriers | 0.4210 | ||||
| Benefit | -0.135864 | 0.8557 | |||
| Intention | -0.266733 | 0.182054 | 0.929 | ||
| Self efficacy | -0.388773 | 0.160378 | 0.431935 | 0.7662 | |
| Susceptibility | 0.081112 | -0.180311 | -0.037354 | -0.138540 | 0.9008 |
The formative construct (social support) was tested by each item weight, t-value and multicollinearity [38]. The t-value indicates whether the path from the indicator to the construct is significant. Critical t-values for a two-tailed test are 1.65 (p < 0.1), 1.96 (p < 0.05), and 2.58 (p < 0.01) [38]. All the items were found to have statistically significant outer weights except one item that was deleted from the construct.
Multicollinearity test performed using SPSS indicated that each indicator variance inflation factor (VIF) was less than cut-off value of 5 and each indicator tolerance value was less than cut-off value of 2 [38].
STRUCTURAL MODEL RESULTS
Figure 1 shows the structural model results. Benefit (b = 0.12, p < 0.01), self-efficacy (b = 0.36, p < 0.01) and social support (b = 0.10, p < 0.05) revealed positive direct relationship with CRC screening intention and barriers (b = -0.14, p < 0.01) and education years (β = 0.16, p < 0.01) revealed negative direct relationship with CRC screening intention. Additionally, susceptibility (β = 0.03, p > 0.05), factor program (β = 0.03, p > 0.05) and age (β = 0.07, p > 0.05) did not associate with CRC screening intention. The model explained 24% of the variability in intention to undergo CRC screening (R2 = 0.24).
The results revealed a significant indirect relationship between barriers and CRC screening intention (b = -0.14, p < 0.01) through the mediating role of self-efficacy and also a significant indirect relationship between social support and CRC screening intention (b = 0.08, p < 0.01) through the mediating role of self-efficacy. Thus, self-efficacy was a partial but not complete mediator. The R 2 value for self-efficacy is 0.206 that suggesting 21% of the variance of self-efficacy can be explained by barriers and social support.
The model’s predictive power was tested by calculating Q2 indexes of intention (Q2 = 0.21) and self-efficacy (Q2 = 0.12), exceeding the recommended threshold value (Q2 > 0) [41], indicating an adequate predictive value of the model. Finally, GoF = 0.36, indicating the model good fit [42].
Discussion
Considering very low level of uptake of CRC screening in Iran, identifying the determinants influencing this health behavior is critical to design an evidence-informed intervention. To our knowledge, this is the first study about the predictors of intention CRC screening (FOBT) using a mediator model among Iranian population. We found that lower perceived barriers and higher perceived benefits, stronger social support, higher self-efficacy and lower education were associated with stronger intention to undergo screening with FOBT. However, perceived susceptibility, factor program and age were not associated with intention. Also, self-efficacy mediates effects of social support and perceived barriers on intention.
The findings demonstrated that perceived benefits and perceived barriers were identified as the significant predictors of screening intention. Perceived barriers were negatively associated with intention to undergo screening with FOBT whereas perceived benefits were positively associated with intention to undergo screening with FOBT. This indicates that participants with high-perception of benefits and low-perception of barriers were more likely to express that they intention to undergo screening than participants having low perception of benefits and high perception of barriers. Therefore, researchers and educators in interventions program can use educating the people about the benefits of CRC screening and trying to relieve their worry about the barriers to undergo screening for CRC. This finding is similar to results reported in Zheng et al. [43] and Gregory et all studies [14] who found lower levels of perceived barriers, higher levers of perceived benefits were significantly associated with high intention respectively.
Contrary to findings from at least two other studies [14, 34], social support was one of the predictors of screening intention. Our finding suggests that family member may be a main source of adults’ social support that could help average-risk adults overcome barriers of CRC screening and could reinforce the adult’s intention through increased perceived ability to undergo CRC screening. Boonyasiriwat et al. [44] found that support from family and friends was associated with stronger intention to undergo CRC screening among relatives of CRC cases. Other studies have also indicated social support has a direct effect on intention or behavior [45, 46].
The current study findings showed self-efficacy which includes the confidence to perform a special behavior was a strong predictor of screening intention so that adults with higher self -efficacy expressed greater intention to be screened for CRC. Prior studies on the association between self-efficacy and intentions indicate consistent results [22, 47]. Also Watts et al. found that self-efficacy can be important in initiating screening intention [18]. Also, self-efficacy partially mediated the relationship between social support and intention, and relationship between perceived barriers and intention in current study. Thus, social support and barriers not only indicated direct impact on intention to screening with FOBT but also had indirect impact via self-efficacy. Our appraisal of the mediating role of self-efficacy, in predicting CRC screening intention among adults could inform health researchers concerning the utility of this construct in designing future interventions. These results guide us to believe that social support, barrier and self-efficacy are important to successfully increase adults’ intention to undergo FOBT screening. Some previous studies suggested that perceived susceptibility predicted screening intention [14, 48]. The current study indicates this construct do not have significantly effects on screening intention. Our data indicated that enhancing the perceived susceptibility of CRC might be less important for screening intention than increasing other construct of PHM. The Extended Parallel Process Model might be helpful to perceive the results regarding perceived susceptibility. According to this model, if adults believe that the early detection of CRC will not decline the risk of CRC, the perception of this risk will not increase the intention to undergo screening [49].
Physician`s recommendations can play an important role, in that eligible persons need to be able to talk about their doubts and their perceived barriers [50]. Physician`s recommendation in health care system to undergo screening for the CRC has been considered in the current study as a program factor. Lack of significant relationship between program factor and intention was inconsistent with results of study done by Boonyasiriwat et al. [44] who reported a positive and direct relationship between health-care provider recommendation and intention. Further, our results regarding education years were surprising. Lower years of education were associated with higher screening intentions. This finding was inconsistent with those of previous studies that reported individuals who intended to screen were more likely to have higher education [51]. Hence, further investigations are essential due to a negative relationship between screening intention and education years among adults in Hamadan city.
In this study, we used a national sampling frame to select the participants and collected data on a broad range of socio-demographic characteristics which makes the findings generalizable to the population. Study limitations include the inability to measure screening behavior (undergo FOBT). Although screening intention has the strongest association with screening behavior, measuring actual behavior (undergo screening) would fortify the overall study. Secondly, cross sectional nature of the study limits causal inferences. Third, the use of self-report measures may raise response bias.
Conclusions
The findings of this study indicated the effectiveness of PHM in predicting the intentions of Iranians to undergo a screening with FOBT for CRC. Self-efficacy, benefits, barriers, and social support were all directly associated with intention to undergo a screening. A partial mediating role of self-efficacy in the association between social support and barriers with intention was revealed. Given that CRC is curable in its earlier stage and screening could reduce the burden of this disease, we must develop theory-based educational programs that encourage Iranian adults to undergo screening.
Fig. 2.
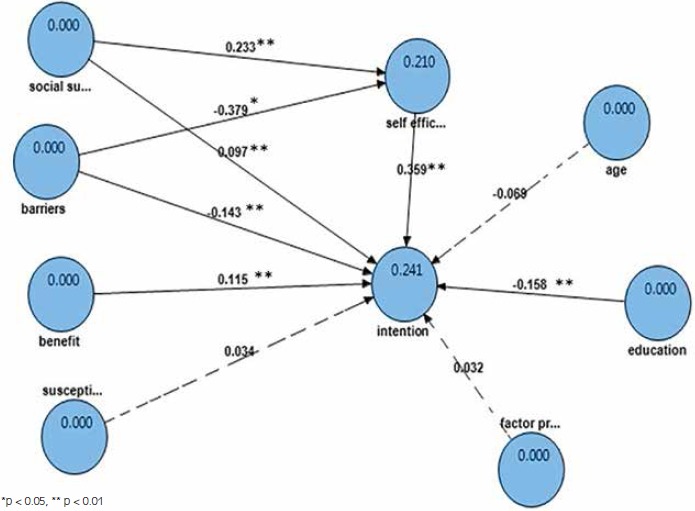
Structural model.
Acknowledgments
This article is part of a Ph.D. thesis in health education and health promotion that was approved by Hamadan University of Medical Sciences. The authors thank all participants in this study.
Ethical approval for the study was provided by Hamadan University of Medical Sciences Ethical Committee whit code p/16/35/9/6385
Footnotes
The authors declared no conflicts of interest.
This study was funded by Hamadan University of Medical Sciences (grant number 9309184585).
Authors’ contributions
FB was involved in conceptualizing, generating of the project, data collection, data analyses and also drafting the manuscript. AKS was involved in conceptualizing, generating of the project, and also drafted the manuscript. JF assisted with the data analyses. SMMH and SB assisted with the conceptualization of the project. All authors read drafts of the manuscript and provided comments.
References
- [1].Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-E86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- [2].Centers for Disease Control and Prevention, Noncommunicable deputy-cancer office. National Cancer Registry Report 2008-2009. Ministry of Health and Medical Education; Tehran; 2012. [Google Scholar]
- [3].Benson VS, Patnick J, Davies AK, Nadel MR, Smith RA, Atkin WS. Colorectal cancer screening: a comparison of 35 initiatives in 17 countries. Int J Cancer 2008;122:1357-67. doi: 10.1002/ijc.23273. [DOI] [PubMed] [Google Scholar]
- [4].Levin B, Lieberman DA, McFarland B, Smith RA, Brooks D, Andrews KS, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin 2008;58:130-60. doi: 10.3322/CA.2007.0018. [DOI] [PubMed] [Google Scholar]
- [5].Moghimi-Dehkordi B, Safaee A. An overview of colorectal cancer survival rates and prognosis in Asia. World J Gastrointest Oncol 2012;4:71-5. doi:10.4251/wjgo.v4.i4.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Smith RA, Andrews K, Brooks D, DeSantis CE, Fedewa SA, Lortet-Tieulent J, et al. Cancer screening in the United States, 2016: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 2016;66(2):96-114.doi: 10.3322/caac.21336. [DOI] [PubMed] [Google Scholar]
- [7].Mousavinezhad M, Majdzadeh R, Akbari Sari A, Delavari A, Mohtasham F. The effectiveness of FOBT vs. FIT: a meta-analysis on colorectal cancer screening test. Med J Islam Repub Iran 2016;30:454-68. [PMC free article] [PubMed] [Google Scholar]
- [8].Sung JJ, Lau JY, Young GP, Sano Y, Chiu H, Byeon J, et al. Asia Pacific consensus recommendations for colorectal cancer screening. Gut 2008;57:1166-76. doi:10.1136/gut.2007.146316. [DOI] [PubMed] [Google Scholar]
- [9].Tappenden P, Eggington S, Nixon R, Chilcott J, Sakai H, Karnon J. Colorectal cancer screening options appraisal. Cost-effectiveness, cost-utility and resourse impact of alternative screening options for colorectal cancer. Report to the English Bowel Cancer Screening Working Group 2004. [Google Scholar]
- [10].Tsoi K, Ng S, Leung M, Sung J. Cost-effectiveness analysis on screening for colorectal neoplasm and management of colorectal cancer in Asia. Aliment Pharmacol Ther 2008;28:353-63. doi: 10.1111/j.0269-2813.2008.03726.x. [DOI] [PubMed] [Google Scholar]
- [11].Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011. CA Cancer J Clin 2011;61:212-36. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- [12].Smith RA, Cokkinides V, Brawley OW. Cancer screening in the United States, 2008: a review of current American Cancer Society guidelines and cancer screening issues. CA Cancer J Clin 2008;58:161-79. doi: 10.3322/CA.2007.0017 [DOI] [PubMed] [Google Scholar]
- [13].Salimzadeh H, Eftekhar H, Delavari A, Malekzadeh R. Psycho-social Determinants of Colorectal Cancer Screening in Iran. Int J Prev Med 2014;5:185. [PMC free article] [PubMed] [Google Scholar]
- [14].Gregory TA, Wilson C, Duncan A, Turnbull D, Cole SR, Young G. Demographic, social cognitive and social ecological predictors of intention and participation in screening for colorectal cancer. BMC Public Health 2011;11:1 doi: 10.1186/1471-2458-11-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. John Wiley & Sons; 2008. [Google Scholar]
- [16].Cole SR, Zajac I, Gregory T, Mehaffey S, Roosa N, Turnbull D, et al. Psychosocial variables associated with colorectal cancer screening in South Australia. Int J Behav Med 2011;18:302-9. doi: 10.1007/s12529-010-9101-1. [DOI] [PubMed] [Google Scholar]
- [17].Hollier JM, Hinojosa-Lindsey M, Sansgiry S, El-Serag HB, Naik AD. Clinical and psychosocial variables associated with behavioral intentions to undergo surveillance endoscopy. BMC Gastroenterol 2014;14:1 doi: 10.1186/1471-230X-14-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Watts BG, Vernon SW, Myers RE, Tilley BC. Intention to be screened over time for colorectal cancer in male automotive workers. Cancer Epidemiol Biomarkers Prev 2003;12:339-49. [PubMed] [Google Scholar]
- [19].Rosenstock IM. The health belief model and preventive health behavior. Health Educ Behav 1974; 2:354-86. doi: 10.1177/109019817400200405. [Google Scholar]
- [20].Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Prentice-Hall; 1980. [Google Scholar]
- [21].Bandura A. Social foundations of thought and action: a social cognitive theory: Prentice-Hall, Inc. 1986. [Google Scholar]
- [22].Myers RE, Ross E, Jepson C, Wolf T, Balshem A, Millner L, et al. Modeling adherence to colorectal cancer screening. Prev Med 1994;23:142-51. [DOI] [PubMed] [Google Scholar]
- [23].McQueen A, Vernon SW, Rothman AJ, Norman GJ, Myers RE, Tilley BC. Examining the role of perceived susceptibility on colorectal cancer screening intention and behavior. Ann Behav Med 2010;40:205-17. doi:10.1007/s12160-010-9215-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Salimzadeh H, Eftekhar H, Majdzadeh R, Montazeri A, Delavari A. Effectiveness of a theory-based intervention to increase colorectal cancer screening among Iranian health club members: a randomized trial. J Behav Med 2014;37:1019-29. doi:10.1007/s10865-013-9533-6. [DOI] [PubMed] [Google Scholar]
- [25].Thirlaway K, Upton D. The psychology of lifestyle: promoting healthy behavior. Routledge; 2009. [Google Scholar]
- [26].Gage GS. Social support and positive health practices in black late adolescents the role of mediating variables. Clin Nurs Res 2015;26:93-113. doi: 10.1177/1054773815594579. [DOI] [PubMed] [Google Scholar]
- [27].Zhang S, Edwards H, Yates P, Li C, Guo Q. Self-efficacy partially mediates between social support and health-related quality of life in family caregivers for dementia patients in Shanghai. Dement Geriatr Cogn Disord 2013;37:34-44. doi:10.1159/000351865. [DOI] [PubMed] [Google Scholar]
- [28].Dishman RK, Motl RW, Sallis JF, Dunn AL, Birnbaum AS, Welk GJ, et al. Self-management strategies mediate self-efficacy and physical activity. Am J Prev Med 2005;29:10-8. doi:10.1016/j.amepre.2005.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Manne S, Kashy D, Albrecht T, Wong Y-N, Flamm AL, Benson AB, et al. Knowledge, attitudes, and self-efficacy as predictors of preparedness for oncology clinical trials a mediational model. Med Decis Making 2014;34:454-63. doi: 10.1177/0272989X13511704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hill K, Startup M. The relationship between internalized stigma, negative symptoms and social functioning in schizophrenia: the mediating role of self-efficacy. Psychiatry Res 2013;206:151-7. [DOI] [PubMed] [Google Scholar]
- [31].McQueen A, Vernon SW, Myers RE, Watts BG, Lee ES, Tilley BC. Correlates and predictors of colorectal cancer screening among male automotive workers. Cancer Epidemiol Biomarkers Prev 2007;16:500-9. doi: 10.1158/1055-9965.EPI-06-0757. [DOI] [PubMed] [Google Scholar]
- [32].Statistical center of Iran, The president’s office deputy of strategic planning and control. National population and housing census 2011 (1390): selected findings. Tehran 2011. [Google Scholar]
- [33].Rashidian A, Karimi-Shahanjarini A, Khosravi A, Elahi E, Beheshtian M, Shakibazadeh E, Khabiri R, Arab M, Zakeri MR. Iran’Multiple Indicator Demographic and Health Survey (IrMIDHS-2010): study protocol. Int J Prev Med 2014;5:632-42. [PMC free article] [PubMed] [Google Scholar]
- [34].Griffin MJ. Health belief model, social support, and intent to screen for colorectal cancer in older African American men. [PhD thesis]. School of Nursing, University of North Carolina at Greensboro; 2011. [Google Scholar]
- [35].Vernon SW, Myers RE, Tilley BC. Development and validation of an instrument to measure factors related to colorectal cancer screening adherence. Cancer Epidemiol Biomarkers Prev 1997;6:825-32. [PubMed] [Google Scholar]
- [36].Hoyle RH. Structural equation modeling: concepts, issues, and applications: Sage Publications; 1995. [Google Scholar]
- [37].Ringle CM, Wende S, Will. SmartPLS (Version 2.0 (beta)). Hamburg, Germany: 2005. [Google Scholar]
- [38].Hair JF, Ringle CM, Sarstedt M. PLS-SEM: indeed a silver bullet. Journal of Marketing Theory and Practice 2011;19:139-52. doi 10.2753/MTP1069-6679190202. [Google Scholar]
- [39].Chin WW. The partial least squares approach to structural equation modeling. Modern methods for business research. Edited by Marcoulides GA. New York: Psychology Press; 1998, pp-295-336. [Google Scholar]
- [40].Straub D, Boudreau M-C, Gefen D. Validation guidelines for IS positivist research. The Communications of the Association for Information Systems 2004;13:63 doi: 10.1007/978-3-540-32827-8_29. [Google Scholar]
- [41].Haenlein M, Kaplan AM. A beginner’s guide to partial least squares analysis. Understanding statistics 2004;3:283-97. [Google Scholar]
- [42].Tenenhaus M, Amato S, Esposito Vinzi V, editors. A global goodness-of-fit index for PLS structural equation modeling. Proceedings of the XLII SIS Scientific Meeting 2004. [Google Scholar]
- [43].Zheng Y-F, Saito T, Takahashi M, Ishibashi T, Kai I. Factors associated with intentions to adhere to colorectal cancer screening follow-up exams. BMC Public Health 2006;6:1 doi: 10.1186/1471-2458-6-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Boonyasiriwat W, Hung M, Hon SD, Tang P, Pappas LM, Burt RW, et al. Intention to undergo colonoscopy screening among relatives of colorectal cancer cases: a theory-based model. Ann Behav Med 2014;47:280-91. doi:10.1007/s10865-006-9068-1. doi:10.1007/s12160-013-9562-y. [DOI] [PubMed] [Google Scholar]
- [45].Honda K, Kagawa-Singer M. Cognitive mediators linking social support networks to colorectal cancer screening adherence. J Behav Med 2006;29:449-60. doi:10.1007/s10865-006-9068-1. [DOI] [PubMed] [Google Scholar]
- [46].Power E, Van Jaarsveld CH, McCaffery K, Miles A, Atkin W, Wardle J. Understanding intentions and action in colorectal cancer screening. Ann Behav Med 2008;35:285-94. doi:10.1007/s12160-008-9034-y. [DOI] [PubMed] [Google Scholar]
- [47].Tolma EL, Reininger BM, Evans A, Ureda J. Examining the theory of planned behavior and the construct of self-efficacy to predict mammography intention. Health Education & Behavio 2006;33:233-51. doi: 10.1177/1090198105277393. [DOI] [PubMed] [Google Scholar]
- [48].Bunn JY, Bosompra K, Ashikaga T, Flynn BS, Worden JK. Factors influencing intention to obtain a genetic test for colon cancer risk: a population-based study. Prev Med 2002;34(6):567-77. doi:10.1006/pmed.2002.1031. [DOI] [PubMed] [Google Scholar]
- [49].Witte K. Putting the fear back into fear appeals: the extended parallel process model. Commun Monogr 1992;59:329-49. doi: 10.1080/03637759209376276. [Google Scholar]
- [50].Valle I, Tramalloni D, Bragazzi N. Cancer prevention: state of the art and future prospects. J Prev Med Hyg 2015;56:E21-7. [PMC free article] [PubMed] [Google Scholar]
- [51].Christou A, Thompson SC. Colorectal cancer screening knowledge, attitudes and behavioral intention among Indigenous Western Australians. BMC Public Health 2012;12:1 doi: 10.1186/1471-2458-12-528. [DOI] [PMC free article] [PubMed] [Google Scholar]


