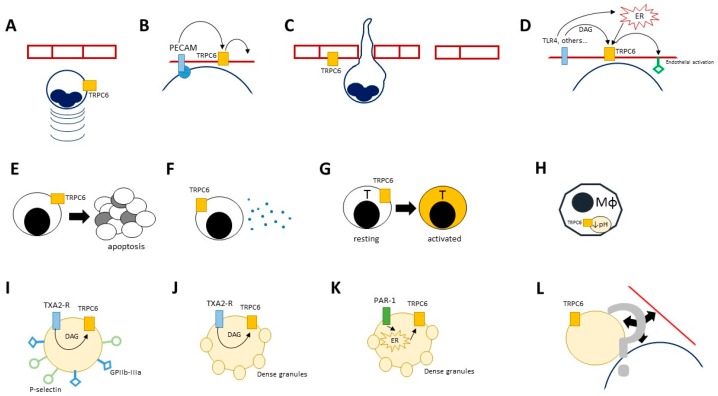
Figure 2.
Effects of TRPC6 on immune cells. Activation of TRPC6 plays a critical role in the control of key cellular functions in several immune-committed cells, such as neutrophils (panel (A–D)), lymphocytes (panel (E–G)), macrophages (panel (H)), platelets (panel (I–L)) and the endothelium (panel (A–D,L)). TRPC6 contributes to neutrophil activation, adhesion to the vascular walls and extravasation by enhancing the stimulatory effects on chemo-attractants such as MIP-2 and CXCR2 (A); by promoting the downstream effects of endothelial cell adhesion molecules such as platelet/endothelial cell adhesion molecule (PECAM; (B)) or surface sensors of pro-inflammatory stimuli such as TLR-4 (D); by favouring the signal cascades that lead to looser transcellular junction between endothelial cells (C). Enhanced TRPC6 activation in lymphocytes might accelerate apoptosis, which could constitute a further trigger for inflammation in autoimmune disorders such as SLE (E). The expression of TRPC6 in T cells promotes cytokine release (F) and cell activation (G), which eventually translate in more aggressive inflammatory or allergic responses. In macrophages, TRPC6 is required for the acidification of endophagolysosomes (H). Platelets express high amounts of TRPC6 and might exploit its activation within ROCE (I,J) or SOCE (K) to undergo activation. Receptor-operated stimulation of TRPC6 downstream the thromboxane A2 (TXA2) pathway might be responsible for surface expression of crucial adhesion molecules such as GPIIb-IIIa or P-selectin (J) and for the release of platelet dense granules (J). This latter event might also occur as the result of TRPC6 activation after mobilisation of calcium from intracellular stores (K). Whether these events might impact on the interaction between platelets, leukocytes and the endothelium is still unknown (L).