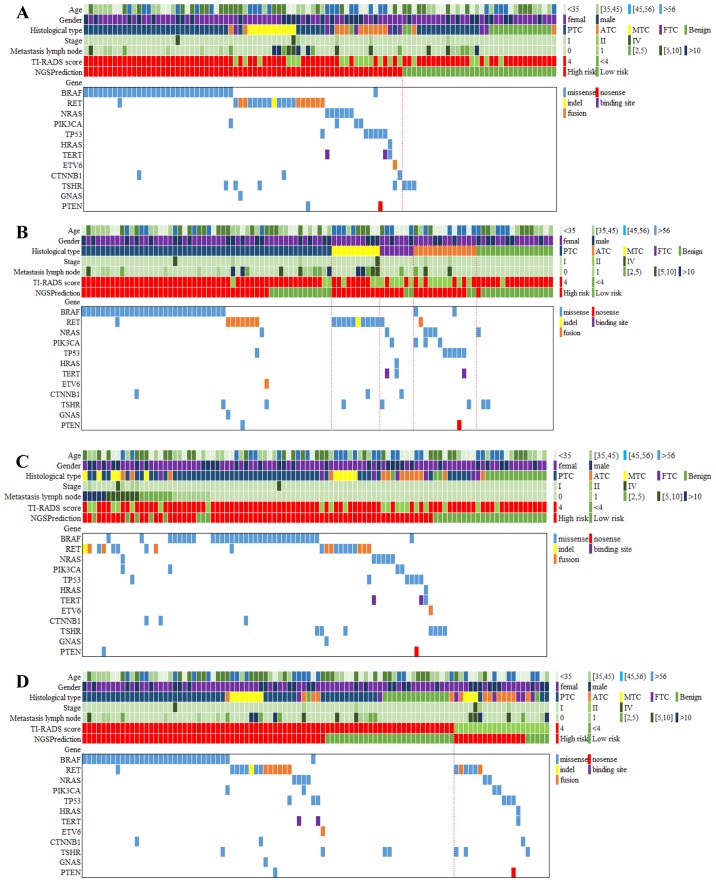
Figure 2.
Gene spectrum grouped by benign and malignant thyroid nodules, pathological subtypes, metastatic lymph nodes and TI-RADS. (A) The gene spectrum of the 98 patients contained age, sex, histological diagnosis of cancer type, tumor stage, metastasis lymph node number, TI-RADS category, NGS prediction result and detailed genetic information. (B) The gene spectra of the four TC subtypes varied. For PTC, BRAF mutations were predominant, while RET mutations were detected among all the MTC. A wide range of mutations were positive but none of them showed dominance in ATC and FTC. (C) A total of 27 patients had 1 or more metastasis lymph nodes, 19 of whom carried 23 mutations, including BRAF (n=8), RET (n=8), NRAS (n=1), PIK3CA (n=2), TP53 (n=1), CTNNB1 (n=2) and PTEN (n=1). (D) Among the 78 US-predicted high-risk patients, 63 cases were diagnosed with TC by histological examination. Out of the 20 US-predicted low-risk patients, only 1 case was diagnosed with benign thyroid nodule by histological examination. TI-RADS, Thyroid Imaging Reporting and Data System; NGS, next-generation sequencing; TC, thyroid cancer; PTC, papillary thyroid cancer; MTC, medullary thyroid cancer; ATC, anaplastic thyroid cancer; FTC, follicular thyroid cancer; US, ultrasound.