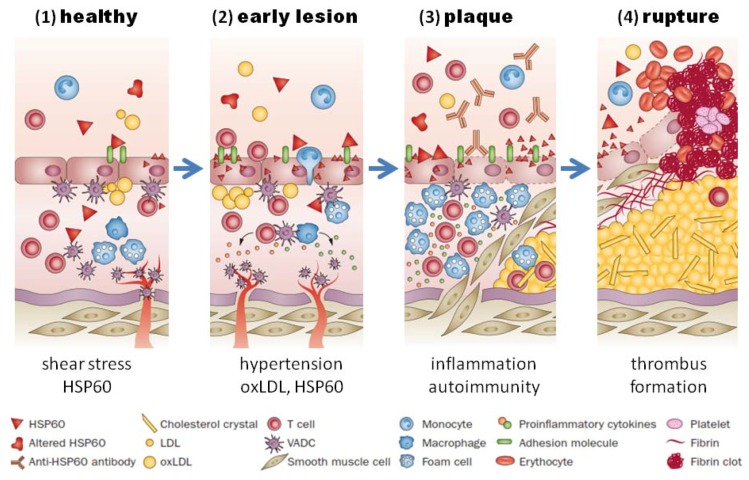
Figure 2.
HSP60-induced atherosclerosis. (1) Healthy arteries are exposed to hemodynamic turbulences leading to shear stress at curves and branching points, which are prone to atherosclerosis; (2) classic risk factors (i.e., high blood pressure) may aggravate the stress response in endothelial cells, which leads to more surface expression of adhesion molecules and HSP60. This, together with secreted HSP60, attracts T cells and other proinflammatory cells to infiltrate the intima. Binding of cross-reactive antibodies to HSP60 to endothelial cells induce an autoimmune response, which promotes endothelial dysfunction and migration of mononuclear cells into the intima; (3) plaques start to develop, when macrophages and vascular smooth muscle are transformed to foam cells and produce proinflammatory cytokines. Soluble HSP60 is further released from damaged cells. If the inflammation persists, the lesion becomes more complex and a necrotic core composed of necrotic and apoptotic cells is formed. Cell debris, cholesterol crystals accumulate, and a fibrous cap is formed; (4) unstable plaques can rupture which leads to exposure of the core to the blood followed by thrombus formation. Abbreviations: HSP, heat shock protein; oxLDL, oxidized LDL; SMC, smooth-muscle cell; VADC, vascular-associated dendritic cell. Adapted from Servier Medical Art. creative commons license http://creativecommons.org/licenses/by/3.0/legalcode ©Servier.