Abstract
Systemic lupus erythematosus (SLE) is an autoimmune inflammatory disease, characterized by the involvement of multiple organ systems. Ocular involvement, being one of the manifestations, contributes to the assessment of disease activity. Purtscher-like retinopathy has been reported as a manifestation of SLE. An otherwise healthy 21-year old female presented with a bilateral rapid decrease in vision for 1 month. Fundus examination revealed multiple cotton wool spots and flame-shaped hemorrhages in both eyes. Optical coherence tomography displayed bilateral severe macular edema. Fundus fluorescein angiography showed multiple retinal arteriolar occlusions. A rheumatologist was consulted for investigation. Based on the American College of Rheumatology 1982 Revised Criteria for diagnosing SLE, a diagnosis of SLE was made. She was subsequently treated with corticosteroids and immunosuppressive medication. Although vaso-occlusive retinopathy is a rare presentation of SLE, it is significant in diagnosing SLE in a patient, to promptly initiate proper treatment.
Systemic lupus erythematosus (SLE) is a complex autoimmune inflammatory disease of unknown etiology. It is characterized by involving multiple organ systems, often with a relapsing and remitting clinical course. Almost one third of SLE patients demonstrate an array of ocular manifestations. The most common manifestation is SLE retinopathy. This typically presents with cotton wool spots with or without flame-shaped hemorrhages.1 SLE retinopathy is usually manifested in patients with active disease, and is more common when associated with antiphospholipid syndrome. The presence of antiphospholipid antibodies, in isolation or in association with SLE, increases the risk of retinopathy.2 Purtscher-like retinopathy (PLR) has been reported to be associated with SLE. This report describes the development of PLR in a young female as a first manifestation of SLE.
CASE
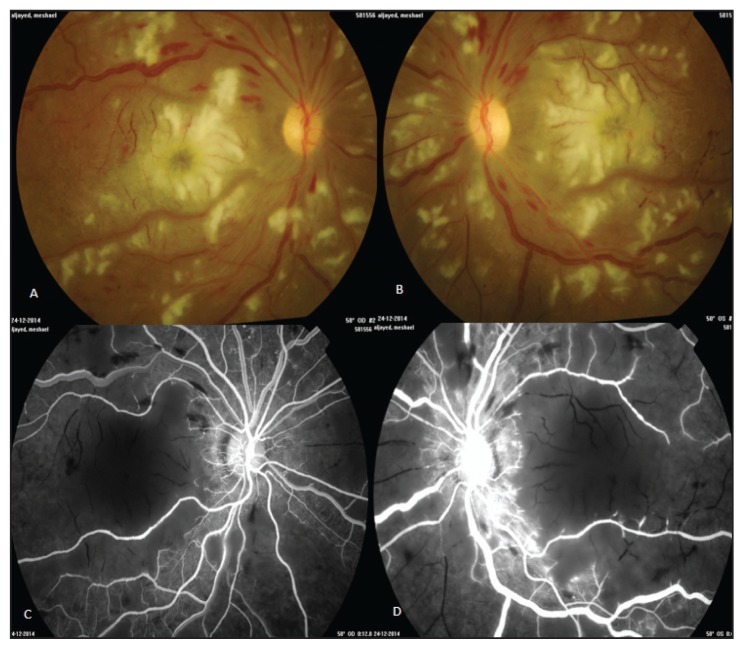
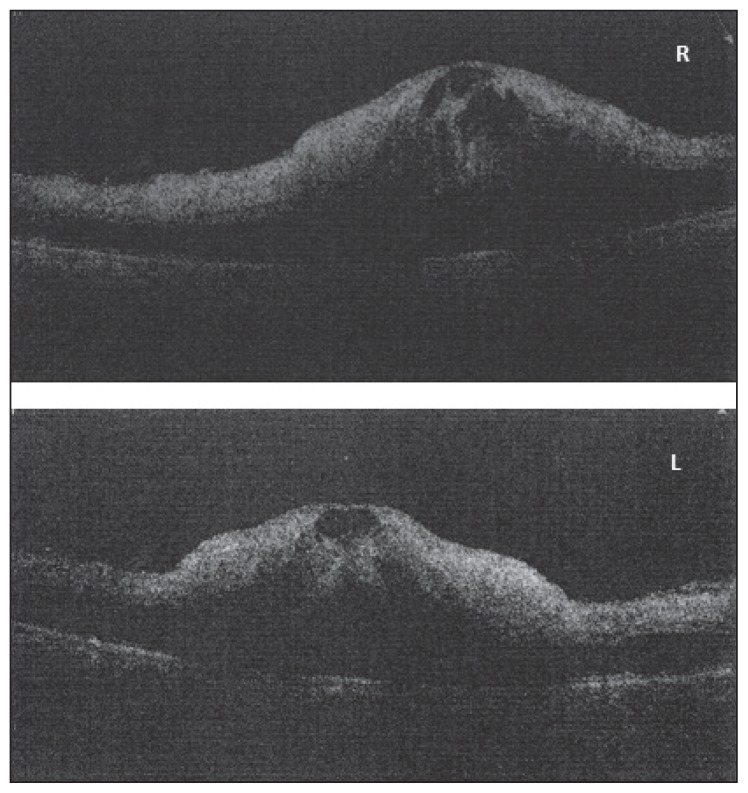
A 21-year-old female presented to the emergency department of King Abdulaziz University Hospital (KAUH), Jeddah, Saudi Arabia with rapid, painless decreased vision in both eyes for 1 month. Ophthalmic examination showed a best-corrected visual acuity of counting fingers at 3 feet for both eyes. The pupils were found to be regular and reactive, with no afferent pupillary defect in both eyes. External eye examination was normal. Slit-lamp examination revealed an unremarkable anterior segment. The intraocular pressure was within the normal range. Fundoscopy revealed a clear vitreous and the presence of large, multiple cotton wool spots and flame-shaped hemorrhages in both eyes. The optic disk was normal (Figure 1). Fundus fluorescein angiography revealed multiple arteriolar occlusions and large areas of capillary drop out (Figure 2). Optical coherence tomography (OCT) displayed severe macular edema of 826 and 853 μm for the right eye and left eye, respectively (Figure 3). The diagnosis of bilateral PLR was made, and an underlying systemic vasculitis entity was suspected. The patient was referred to a rheumatologist.
Figure 1.
A 21-year old woman with decreased vision in both eyes for 1 month. (A, B) Fundus photographs show multiple cotton wool spots and flame-shaped hemorrhages. (C, D) Fluorescein angiography shows multiple arteriolar occlusions and large areas of capillary drop-out.
Figure 2.
Optical coherence tomography (OCT) of a 21-year old female with rapid decreased vision. OCT displayed severe macular edema of 826 and 853 μm for the right (R) eye and left (L) eye, respectively.
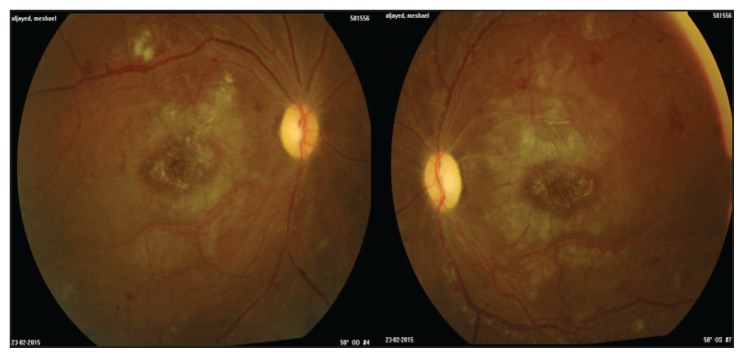
Figure 3.
Fundus photograph of a woman with systemic lupus erythematosus retinopathy 1 month post treatment. Fundus photograph shows a decrease in number and size of cotton wool spots and resolved macular edema bilaterally.
A detailed medical history revealed that the patient had contracted persistent low-grade fever, rigors, night sweats, anorexia, fatigue, and complaints of oral ulceration and erythema over the cheeks, suggestive of malar rash 2 months prior to presentation. She had an unremarkable medical history and was not on any medication. On examination, she was 60 inches (1.5 meters) tall and weighed 110 lbs (50 kilograms). She was found to have generalized lymphadenopathy and subungual pre-gangrene, later affirmed as a sign of vasculitis. The remainder of the physical examination was unremarkable with no signs of skin manifestations, mucocutaneous ulcers, or arthritis.
Initial laboratory investigations showed evidence of pancytopenia: leukocytes 1.9×109/L, neutrophils 1.4×109/L, hemoglobin 81 g/L, reticulocytes 1.1%, and platelets 71×109/L. Mid-stream urine and dipstick were significant for +2 protein, +2 hemoglobin, 42 white blood cells, and 51 red blood cells with no growth recorded. Twenty-hour urine samples revealed a total protein loss of 0.43 g/L and serum albumin of 23 g/L. Computed tomography demonstrated few tiny mediastinal lymph nodes. Axillary lymph node biopsy reported lymphoid hyperplasia, with no malignant cells.
Hematologic workup revealed antinuclear antibody titer levels of >1:2560 (N<1180) with speckled pattern, anti-deoxyribonucleic acid antibodies at 1734 IU/mL (N<200 IU/mL), and elevated levels of anticardiolipin antibodies (ACA) immunoglobulin M (IgM) 31 (N<18 MPL), ACA IgG 23 (N<14 GPL). Complement factors C3 and C4 decreased to 0.178 and 0.041, respectively. Ultrasound-guided kidney biopsy was obtained, and it confirmed class IV lupus nephritis with minimal disease activity, plus very early membranous changes class V.
Based on the American College of Rheumatology 1982 revised criteria for diagnosing SLE, a diagnosis of SLE with moderately elevated antiphospholipid antibody was made. The patient was treated with 20 mg intravenous methylprednisolone, to be tapered off for 3 months according to her response. She was discharged on 50 mg prednisone for 6 days, to be tapered down by 5 mg every week and maintained at 10 mg once daily for 2 months, 500 mg mycophenolate mofetil twice daily for 5 days, 200 mg hydroxychloroquine sulfate, and warfarin 2 mg for 3 months to be decreased to 1 mg, within 1 month, and to continue this dose for at least 2 years.
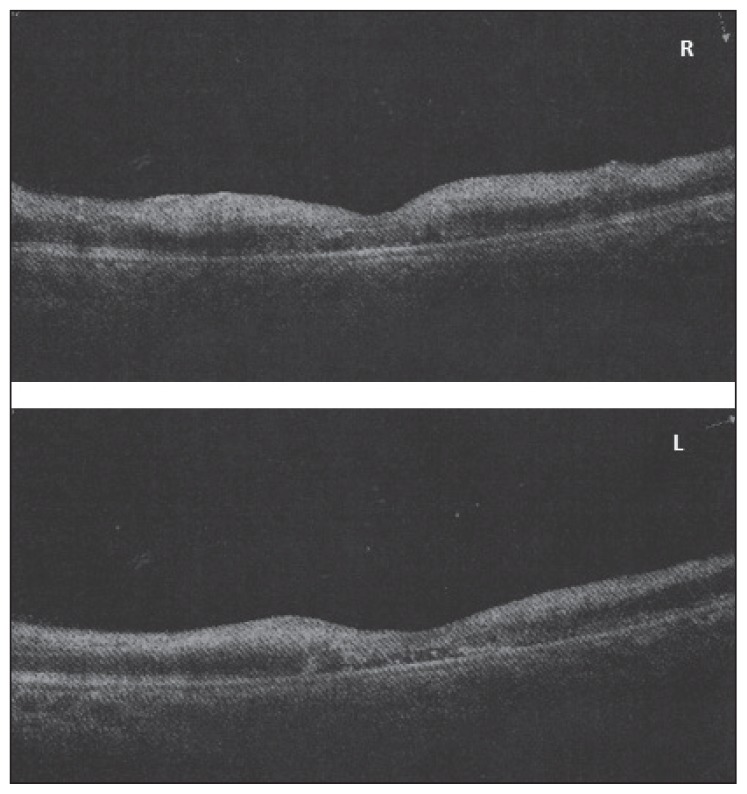
After 1-month, her follow-up at the ophthalmology clinic at KAUH revealed an improved visual acuity to 20/400 and 20/200 for the right eye and left eye, respectively. Fundus examination revealed a decrease in number and size of cotton wool spots and a pale optic nerve head for both eyes (Figure 3). OCT was performed, showing decreased retinal thickness and resolved macular edema to 226 μm and 169 μm for both the right eye and the left eye, respectively (Figure 4). Additional follow up with the eye clinic was recommended after 8 to 10 weeks of treatment for monitoring. No additional medication was prescribed.
Figure 4.
Optical coherence tomography (OCT) of a woman with PRL associated with systemic lupus erythematosus after treatment. OCT shows decreased retinal thickness and macular edema to 226 μm and 169 μm for both the right (R) eye and the left (L) eye, respectively.
DISCUSSIONS
Based on the 1997 update of the 1982 American College of Rheumatology Revised Criteria for Classification of Systemic Lupus Erythematosus,3 retinopathy is not included in the diagnostic parameters. It is a well-known complication of SLE with an incidence of 29% in patients with active disease.1
Purtscher retinopathy (PR) generally occurs as a result of trauma or thoracic compression. A funduscopic picture virtually identical to that of PR may occur with non-traumatic causes and labeled PLR. The most frequently associated cause is acute pancreatitis. Autoimmune disorders such as SLE, dermatomyositis, and scleroderma have also been reported.4
The characteristic ophthalmic findings in PLR include multiple patches of superficial retinal whitening and retinal hemorrhages surrounding the optic nerve head, which usually appears normal. Fluorescein angiography usually demonstrates the leakage of dye from retinal arterioles, capillaries, and venules in patients with relatively mild PLR. In this case, the evidence of arteriolar obstruction and dye leakage was noted, which is characteristic of a severe form of PLR.5
This case has been identified for demonstrating PLR as a first manifestation of SLE. Chang-Wu et al reported 8 cases of PLR in patients previously diagnosed with SLE in an observational case series.6 The ophthalmic complication was attributed to central nervous lupus and highly active disease (>20). The patient in this report displayed disease activity of 41 according to the SLE disease activity index (SLEDAI). Also, a few others reported PLR associated with SLE,6–10 all of whom recorded good visual-acuity prognosis following corticosteroid treatment. However, patients with antiphospholipid antibodies had a more severe form of retinopathy and carried a worse visual prognosis.
The pathogenesis of PLR is still uncertain. It has been proposed that complement activation and leukoembolization by leukocyte aggregation with secondary lymph extravasation is implicated in the occurrence of PLR.7,11,12
In conclusion, a young female patient who presented with severe PLR, which led to the diagnosis of SLE, is reported. This case highlights the fact that ocular manifestation could precede the occurrence of a serious manifestation of SLE and the role ophthalmologists could play in the diagnosis of SLE.
Acknowledgments
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript. This manuscript describes the original work and is not under consideration by any other journal. All authors approved the manuscript and this submission.
REFERENCES
- 1.Palejwala NV, Walia HS, Yeh S. Ocular manifestations of systemic lupus erythematosus: a review of the literature. Hindawi Publishing Corporation, Autoimmune Diseases. 2012;2012(290898):9. doi: 10.1155/2012/290898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Au U, O’Day J. Review of severe vaso-occlusive retinopathy in SLE and the antiphospholipid syndrome; associations, visual outcomes, complications and treatment. Clin Experimint Ophthalmol. 2004;32:87–100. doi: 10.1046/j.1442-9071.2004.00766.x. [DOI] [PubMed] [Google Scholar]
- 3.Hochberg MC. Updating the American College of Rheumatology Revised Criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40:1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 4.Miguel AI, Henriques F, Azevedo LF, Loureiro AJ, Maberley DA. Systematic review of Purtscher’s and Purtscher-like retinopathies. Eye (Lond) 2013;27(1):1–13. doi: 10.1038/eye.2012.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gass JD. Stereoscopic atlas of macular diseases: diagnosis and treatment. (Third edition) 2 [AUTHOR: Details of publisher and location missing. Please provide the same] [Google Scholar]
- 6.Wu C, Dai R, Dong F, Wang Q. Purtscher-like retinopathy in systemic lupus erythematosus. Am J Ophthalmol. 2014;158(6):1335–41. doi: 10.1016/j.ajo.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Sellami D, Ben Zina Z, Jelliti B, Abid D, Feki J, Chaabouni M. Purtscher-like retinopathy in systemic lupus erythematosus. Two cases. J Fr Ophthalmol. 2002;25:52–5. [PubMed] [Google Scholar]
- 8.Kunavisarut P, Pathanapitoon K, Rothova A. Purtscher-like retinopathy associated with systemic lupus erythematosus. 2014. [DOI] [PubMed] [Google Scholar]
- 9.Prabhu Loss of vision following fever in a young female. AECS Illumin. :14–6. [AUTHOR: Please provide the year of publication] [Google Scholar]
- 10.Cruz FM, Chan I, Tee C, Gulay C, Dans L, Otadoy-Augustin J, Recto M. Retinopathy in a patient with systemic lupus erythematosus. Philipp J Ophthalmol. 2009;34(2):66–9. [Google Scholar]
- 11.Pedro G, Vinay A. Purtscher retinopathy and Purtscher-like retinopathy [Internet] 2014. [Accessed during April, 2014]. Available from Eyewiki.aao.org.
- 12.Agrawal A, Mckibbin M. Purtscher’s retinopathies: a review. Surv Ophthalmol. 2006;51:129–36. doi: 10.1016/j.survophthal.2005.12.003. [DOI] [PubMed] [Google Scholar]