Abstract
Introduction
Although poverty is an established correlate of poorer mental health for pregnant women, limited research has examined the mental health effects of material hardship (i.e., difficulties meeting basic needs such as for food, transportation, or stable housing) during pregnancy.
Method
The current research examined rates of material hardship among pregnant women seeking prenatal care and the relationships of both income and material hardship with depression and anxiety during pregnancy. Pregnant women (N = 892) responded to self-report measures of mental health symptoms, annual household income, and current material hardship in the waiting areas of community-based obstetrics/gynecology practices serving primarily financially disadvantaged patients.
Results
About 56% of the sample reported some form of material hardship. About 19% of the sample reported elevated depression, and 17% reported elevated anxiety. Both depression and anxiety were uniquely associated with lower income and greater material hardship, even after controlling for age, race/ethnicity, relationship status, and number of children in the home. Furthermore, material hardship partially mediated the effect of income on mental health symptoms.
Discussion
The physical, emotional, and social effects of deprivation of basic daily needs may contribute to pregnant women’s experiences of mental health symptoms. These results converge with the broader literature focused on the social determinants of physical and mental health. When symptoms of depression and anxiety reflect distress related to material hardship, addressing unmet social needs may be more effective than mental health treatment.
Significance
To our knowledge, the current study is the first to investigate material hardship as related to mental health symptoms among pregnant women in the U.S. These data show that hardship is not uncommon and many pregnant women who face difficulties meeting basic daily needs experience depression and anxiety. As such, material hardship promotes risk for poorer maternal and child well-being. A focus on the roles of social determinants of mental health, including income and material hardship, expands our understanding of ways in which pregnant woman are vulnerable to mental health problems that will likely affect their maternal functioning.
Keywords: pregnancy, depression, anxiety, income, material hardship
Introduction
Pregnancy involves physical and psychological changes that may render women vulnerable to developing mental health symptoms. Depression and anxiety during pregnancy are associated with risky health behaviors such as smoking and with adverse pregnancy outcomes such as low birth weight (e.g., Grote et al., 2010; Marcus, 2009; Räisänen et al., 2014). Symptoms of depression and anxiety during pregnancy also predict increased risk for poorer postpartum mental health and mother-infant attachment (e.g., Norhayati, Hazlina, Asrenee, & Emilin, 2015; Rich-Edwards et al., 2006). Studies of antenatal mental health are important because many pregnant women regularly interact with health care professionals who might identify problems and offer support, treatment, or referrals. Addressing depression and anxiety during pregnancy also capitalizes on the opportunity to improve birth outcomes and child development trajectories.
Researchers seeking to understand antenatal (and maternal) mental health can draw on a broader theoretical and empirical framework based on the social determinants of health (Lynch et al., 2004; Mechanic, 2001). The World Health Organization (WHO) describes how structural inequalities in power, income, and other resources lead to “the unequal distribution of health-damaging experiences” that affect “the conditions of daily life” (CSDH, 2008, p. 1), including mental health (WHO & Calouste Gulbenkian Foundation, 2014). Consistent with this broader framework, individuals who have lower incomes also have higher lifetime and 12-month incidences of depressive, anxiety, and substance use disorders (e.g., Kessler et al., 1994; Muntaner, Eaton, Miech, & O’Campo, 2004). Similarly, among pregnant women, those with lower incomes also report greater symptoms of depression (Fellenzer & Cibula, 2014; Koleva, Stuart, O’Hara, & Bowman-Reif, 2011), anxiety (Bödecs et al., 2013; Faisal-Cury & Menezes, 2007; Fisher et al., 2013), and poor birth outcomes (Blumenshine, Egerter, Barclay, Cubbin, & Braveman, 2010).
One common correlate of low income that may help explain why income adversely affects pregnant women’s mental health is material hardship, also known as financial hardship or social deprivation (e.g., Butterworth, Rodgers, & Windsor, 2009). Material hardship refers to difficulties in meeting basic daily needs such as food, housing, or transportation (Boushey, Brocht, Gundersen, & Bernstein, 2001). To the degree that low income interferes with the ability to meet basic needs, an individual’s health may be disrupted. Material hardship may both directly and indirectly lead to health problems. That is, health is directly compromised by the effects of deficient nutrition, exposure to dangerous or unhealthy environments, and other deprivations (e.g., Lynch et al., 2000). Health also is indirectly compromised by stress and worry about the perceived inability to meet basic needs (Butterworth et al., 2009). Material hardship may be particularly devastating for pregnant women given that thriving during a healthy pregnancy requires access to adequate nutrition, a safe and reliable place to sleep, transportation to medical appointments, and an ability to communicate by phone with health providers and other sources of social support.
Some evidence suggests that material hardship, in addition to low income, adversely affects the mental health of new and expecting mothers. Among new mothers in the U.S, postpartum material hardship (difficulties accessing infant formula, baby food, diapers, food, or paying one’s rent/mortgage) was linked to postpartum depressive symptoms (Rich-Edwards et al., 2006). Furthermore, in studies of pregnant women outside of the U.S, indicators of material hardship have been negatively associated with antenatal mental health. Among women in a poor rural province in Vietnam, socioeconomic adversity (defined in terms of income insecurity and food insecurity) was associated with elevated symptoms of anxiety and depression (Fisher et al., 2013). Similarly, among pregnant women living in a semi-urban community in Swaziland, food insecurity was associated with elevated depressive symptoms (Målqvist, Clarke, Matsebula, Bergman, & Tomlinson, 2016).
These latter two studies provide preliminary evidence that material hardship, specifically food insecurity, adversely affects antenatal mental health. Yet this evidence is based on studies of women in low-income countries with difficulties accessing resources. Because it is unclear whether these patterns of findings generalize across countries with different cultural, social, and economic conditions, studies of women in middle or upper income countries who have difficulties accessing resources also are needed. Although mothers and infants in urban cities in the U.S. show high levels of poverty and concomitant health problems (Save the Children, 2015), to our knowledge, the current study is the first to investigate material hardship in relation to antenatal mental health in the U.S.
The current study also investigated maternal hardship as a potential mediating variable accounting for the effect of income on antenatal mental health. Studying the effects of antenatal material hardship on women’s mental health expands upon the existing literature on hardship and maternal mental health. In a study of U.S. mothers of young children, Heflin and Iceland (2009) operationalized material hardship by quantifying problems across multiple areas: access to food, paying bills (rent, electricity), lack of medical care, no telephone, and unstable housing. When both income and material hardship were included as predictors of a positive screen for depression, material hardship partially mediated the effect of income on depression. Similarly, in a study of Australian women with at least one child in the home, Crosier, Butterworth, and Rodgers (2007) defined material hardship in terms of difficulties paying bills (i.e., rent/mortgage, electricity, gas or telephone, food, heat), having pawned or sold belongings, or having asked for financial help (from friends, family, or from welfare/community agencies). These authors found that material hardship partially mediated the effect of income on the presence of disabling mental health symptoms. If these observed patterns of relationship found among mothers also exist among pregnant women, material hardship may partially or fully account for the effect of income on antenatal mental health.
In summary, we investigated the associations among income, material hardship and mental health (i.e., depression and anxiety) among primarily low income pregnant women served by women’s health practices. Our aims were a) to assess rates of different types of antenatal material hardship/unmet needs (i.e., for food, transportation, clothing, housing, and phone access), and b) to test a mediational model examining the role of material hardship in accounting for the effect of lower income on antenatal mental health symptoms.
Methods
Participants and Procedure
We recruited 3698 study participants from the waiting areas of three community-based practices providing routine and specialty women’s health care to primarily low income patients in upstate New York from 12/2013 to 10/2015. Trained research assistants approached patients waiting for appointments to invite participation in a brief, anonymous screening for a study on mood and quality of life for obstetrics/gynecology patients. The use of an electronically-administered screening allowed women to respond to items privately without being observed. Only those who were pregnant at the time of the screening (N = 892) were included in the present analysis.
Measures
Depression was assessed with Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001), a 9-item self-report measure of symptoms over the past two weeks. Items are rated on 4 point scale (0 = not at all, 3 = nearly every day). Possible scores range from 0 to 27 (M = 5.70, SD = 4.82, range 0 – 26, Cronbach’s α = .83). This screening tool has been validated in obstetrics/gynecology settings, including with pregnant women (Sidebottom, Harrison, Godecker, & Kim, 2012). Multiple studies report evidence for the psychometric properties of the PHQ-9 in samples of women who are pregnant, and the PHQ-9 shows adequate concordance with the Edinburgh Postnatal Depression Scale (e.g., Flynn et al, 2011; Zhong et al., 2014). The PHQ-9 authors suggest that scores of 10 or greater suggest moderately elevated depressive symptoms; this threshold was our indicator of depression.
Anxiety was assessed with the Generalized Anxiety Disorder scale (GAD-7; Spitzer Kroenke, Williams, & Lowe, 2006), a validated 7-item screening measure for the presence of an anxiety disorder. Items assess symptoms over the past two weeks. Ratings are made on a 4 point scale (0 = not at all, 3 = nearly every day). Possible scores range from 0 to 21 (M = 4.86, SD = 5.46, range 0 – 21, Cronbach’s α = .93). The standard threshold score of 10, suggested by Kroenke, Spitzer, Williams, Monahan, and Lowe (2007), was our indicator of anxiety. This screening tool has been validated for use with antenatal populations (e.g., Zhong et al., 2015).
Household income was assessed with the following item: “Approximately what was your total household income last year (include income from all sources, such as Social Security, child support) for everyone in your household)?” on a six point scale (0 = $0 to $9,999; 5 = $50,000 or greater).
Material hardship was assessed with items adapted from past studies (e.g., Heflin & Iceland, 2009) in which similar items were meaningfully associated with both income and with mental health symptoms. The six items used in the current study reflected current basic needs important for health during pregnancy: “I have enough food in the house,” “I have transportation to get to and from my medical appointments,” “I have appropriate clothing,” “My housing is safe,” “My housing is stable,” and “I have access to a working phone.” Participants rated each item on a five point scale from 0 (not at all true) to 4 (very true). As in past research (e.g., Crosier et al., 2007), responses to each item were scored to reflect whether respondents reported any need in each area. The number of areas of any need (0 = no need, 1 = need) were summed so possible scores ranged from 0 to 6 (Cronbach’s α = .89).
Demographic variables assessed were age, relationship status (separated/divorced, single, or widowed = 0, married or living with partner = 1), self-identified racial/ethnic minority (White = 0, Asian/Pacific Islander/Native American, Black, Hispanic, Native American, or “other” = 1), and number of children under age 18 at home.
Data Analytic Plan
Correlational analyses (Pearson’s r for continuous variables and Spearman’s rho for categorical variables) were conducted to examine associations among depression, anxiety, income, material hardship, and demographic variables. Potential indirect (i.e., mediating) effects of material hardship linking income to clinically meaningful mental health symptoms were tested using logistic regressions and bootstrapping procedures from Hayes’ (2013) PROCESS macro. We planned to include income, level of material hardship, and demographic variables into separate logistic regressions for depression and anxiety to calculate the odds ratios for each independent variable adjusted for each other independent variable. An indirect effect of hardship is estimated using regression to quantify how much two cases that differ by a unit on income also differ in mental health as a result of the joint influence of a) the association between income and hardship and b) the association between hardship and mental health. Bootstrapping uses repeated random resampling with replacement from the available data to approximate a sampling distribution of the indirect effect. The significance of the indirect effect, based on the 95% confidence interval (CI) derived from 5,000 bootstrap resamples, is indicated when the bias-corrected CI values do not include zero.
Results
Table 1 lists the sample demographic characteristics. As shown, the majority of women were between 20 and 29 years old. The modal participant (49.9%) was single, not cohabiting, and never married. About half identified as Black, about a third identified as White, and 16.5% identified as Hispanic. Roughly 75% of participants reported having at least one child under the age of 18 at home. Almost 60% reported a household income of less than $20,000/year.
Table 1.
Demographic characteristics of the 892 participants.
| N | % | Mean | SD | Range | |
|---|---|---|---|---|---|
| Age | 26.34 | 5.01 | 18–43 | ||
| 18–19 | 72 | 8.1% | |||
| 20–29 | 547 | 61.3% | |||
| 30–39 | 206 | 23.1% | |||
| 40–49 | 15 | 1.7% | |||
| Not reported | 52 | 5.8% | |||
| Race/Ethnicity | |||||
| Black | 447 | 50.1% | |||
| White | 300 | 33.6% | |||
| Hispanic | 147 | 16.5% | |||
| Other | 52 | 5.8% | |||
| Relationship Status | |||||
| Married | 165 | 18.5% | |||
| Living w/ Partner | 221 | 24.8% | |||
| Separated/Divorced | 42 | 4.7% | |||
| Single | 445 | 49.9% | |||
| Widowed | 1 | 0.01% | |||
| Not reported | 18 | 2.0% | |||
| Children in home | 1.32 | 1.26 | 0–8 | ||
| 0 | 245 | 27.6% | |||
| 1 | 267 | 29.9% | |||
| 2 | 174 | 19.5% | |||
| 3 or more | 133 | 14.8% | |||
| Not reported | 72 | 8.1% | |||
| Income | 1.33 | 1.50 | 0–5 | ||
| Less than $10,000 | 324 | 36.3% | |||
| $10,000–$19,999 | 202 | 22.6% | |||
| $20,000–$29,999 | 140 | 15.7% | |||
| $30,000–$39,999 | 71 | 8.0% | |||
| $40,000–$49,999 | 32 | 3.6% | |||
| $50,000 or greater | 57 | 6.4% | |||
| Not reported | 66 | 7.4% |
On average, respondents reported 1.58 (SD = 1.93, range 0 to 6) unmet needs, reflecting considerable variability in material hardship. Although the modal respondent reported no unmet needs (44.3%), about 7.6% reported at least some need in all six areas. Specific forms of material hardship experienced, in descending order of frequency, involved transportation to medical appointments (37.3%), food (36%), clothing (31.6%), stable housing (22.6%), access to a working phone (16.9%) and safe housing (15.1%). About 19% of the sample scored at or above the screening threshold of 10 on the PHQ-9 for depression, and about 17% scored at or above the screening threshold of 10 on the GAD-7 for anxiety.
Associations among the study variables are reported in Table 2. Depression and anxiety each were negatively associated with income and positively associated with material hardship. Demographic correlates of income and hardship were also observed. Women with relationship partners tended to report greater income, less material hardship, and to be older than women without relationship partners. Women who identified as part of a racial/ethnic minority group tended to report less income, more material hardship, and also tended to be younger, not cohabiting/married, and to have more children in the home than those who identified as White.
Table 2.
Zero-order correlations among study variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Depression + | – | ||||||
| 2. Anxiety + | .55*** | – | |||||
| 3. Income+ | −.18*** | −.18*** | – | ||||
| 4. Material hardship | .29*** | .31*** | −.28*** | – | |||
| 5. Age | −.08* | −.07 | .27*** | −.10** | – | ||
| 6. Number of children | .07 | .06 | −.03 | −.01 | .23*** | – | |
| 7. Racial/ethnic minority | .07 | .02 | −.21*** | .08** | −.19*** | .14** | – |
| 8. Relationship status+ | −.16*** | −.12** | .28*** | −.26*** | .15*** | .00 | −.20*** |
Note: +denotes categorical variable: depression (0 = low or absent, 1 = elevated), anxiety (0 = low or absent, 1 = elevated), income (0 = less than $10,000, 5 = $50,000 or greater), racial/ethnic minority (0 = no, 1 = yes), relationship status (0 = single, widowed, or divorced, 1 = married or cohabiting),
p < .05;
p < .01;
p < .001
The potential indirect (i.e., mediating) effects of material hardship linking income to mental health symptoms were tested using logistic regression analyses and Hayes’ (2013) PROCESS macro. The results of the logistic regression analysis for depression are presented in Table 3. As can be seen, lower income increased the odds of depression, as did the measure of material hardship. None of the demographic variables were associated with a greater likelihood of depression. The analysis also showed a significant bootstrapped estimate for an indirect path linking income to depression via hardship (ab = -.08, 95% CI [-.12, -.05]), and furthermore, there was also a significant direct effect of income on depression (c’ = -.18, p = .037, 95% CI [-.36, -.01]), suggesting partial mediation. Figure 1 shows the significant direct and indirect paths linking income and material hardship to depression after controlling for demographic variables.
Table 3.
Logistic regression model predicting elevated depression on the PHQ-9
| Variable | Coefficient | Standard | P | Odds Ratioa | 95% Confidence |
|---|---|---|---|---|---|
| Error | Interval | ||||
| Income | −0.18 | 0.09 | .037 | 0.83 | 0.70, 0.99 |
| Material hardship | 0.32 | 0.05 | .000 | 1.37 | 1.24, 1.52 |
| Age | −0.01 | 0.02 | .63 | 0.99 | 0.95, 1.03 |
| Number of children | 0.13 | 0.08 | .10 | 1.14 | 0.98, 1.33 |
| Racial/ethnic minority | 0.12 | 0.25 | .64 | 1.13 | 0.69, 1.83 |
| Relationship status | −0.36 | 0.23 | .11 | 0.70 | 0.45, 1.08 |
Odds ratios are adjusted for other terms included in the model, and odds ratios for continuous independent variables reflect the multiplicative increase in odds for elevated symptoms associated with a one point change in the independent variable; full model χ2(6) = 69.17, p < .001, Nagelkerke R2 = .16.
Figure 1.
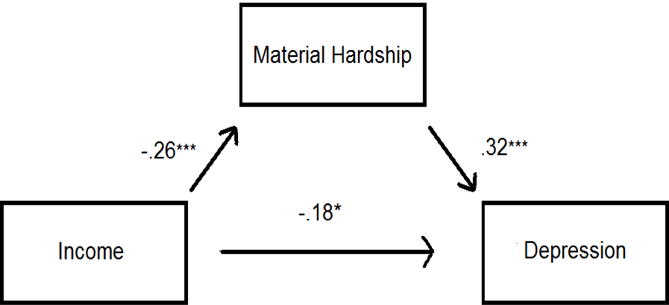
Direct and indirect paths linking income, material hardship, and depressive symptoms
The results of the logistic regression analysis for anxiety are presented in Table 4. The same pattern of results emerged. Both lower income and greater material hardship increased the odds of anxiety. None of the other demographic variables significantly added to the model. Again, there was a significant indirect path linking income to anxiety via hardship (ab = -.09, 95% CI [-.13, -.05]) as well as a significant direct effect of income on anxiety (c’ = -.24, p = .018, 95% CI [-.44, -.04]). Figure 2 shows the significant paths linking income and material hardship to anxiety after controlling for demographic variables.
Table 4.
Logistic regression model predicting elevated anxiety on the GAD-7
| Variable | Coefficient | Standard | P | Odds Ratioa | 95% Confidence |
|---|---|---|---|---|---|
| Error | Interval | ||||
| Income | −0.24 | 0.10 | .019 | 0.79 | 0.64, 0.96 |
| Material hardship | 0.34 | 0.06 | .000 | 1.41 | 1.26, 1.58 |
| Age | −0.02 | 0.02 | .43 | 0.98 | 0.94, 1.03 |
| Number of children | 0.14 | 0.09 | .13 | 1.15 | 0.96, 1.39 |
| Racial/ethnic minority | −0.29 | 0.27 | .28 | 0.75 | 0.44, 1.26 |
| Relationship status | −0.22 | 0.25 | .38 | 0.80 | 0.49, 1.32 |
Odds ratios are adjusted for other terms included in the model, and odds ratios for continuous independent variables reflect the multiplicative increase in odds for elevated symptoms associated with a one point change in the independent variable; full model χ2(6) = 63.44, p < .001, Nagelkerke R2 = .17.
Figure 2.
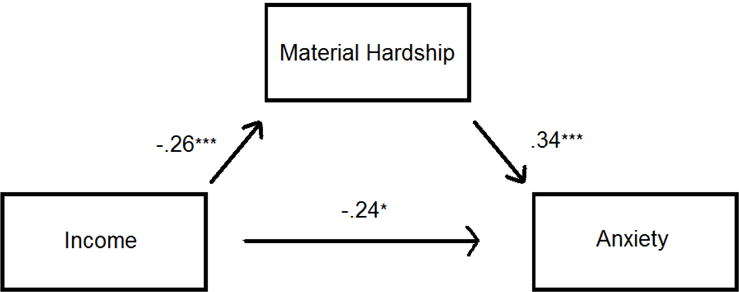
Direct and indirect paths linking income, material hardship, and anxiety symptoms
Discussion
We investigated antenatal material hardship among a predominantly low income sample of pregnant women. Most of the sample reported some type of hardship, and the most common unmet needs involved transportation and food insecurity. Overall level of material hardship was positively associated with antenatal mental health symptoms across both univariate and multivariate analyses controlling for relevant demographic variables. Therefore, the current results suggest that many pregnant women within low income areas are unable to meet basic daily needs directly related to antenatal health; furthermore, being unable to meet daily needs is significantly associated with antenatal depression and anxiety.
The current findings also suggest that material hardship partially mediated the association between lower income and poorer antenatal mental health. Logistic regression analyses showed that both income and hardship uniquely predicted clinically meaningful symptoms. Path analyses showed that there was a significant indirect effect of marital hardship linking lower income to clinically meaningful mental health symptoms, as well as a significant direct effect of income. These patterns replicate past research with mothers (Crosier et al., 2007; Heflin & Iceland, 2009). Despite differences in operational definitions for both income and material hardship across each study, the current results extend this pattern to expectant mothers, some of whom were already parenting. The reliability of the partial mediating effect of hardship is important because of different operational definitions across studies and because of a potential mismatch between income and hardship documented among low income mothers (e.g., Heflin, Corcoran, & Siefert, 2007), which also may be likely during pregnancy. That is, some pregnant women may receive material help from the government, families, or partners because of their pregnancy, despite low income. Such help is important because income alone may not sufficiently address the basic needs of new or expecting mothers and thus may not fully protect against mental health problems.
Because the current findings are based on cross-sectional data, neither causality nor temporality can be established. Although these data do not show that income and material hardship lead to antenatal mental health problems, other longitudinal studies do suggest that hardship predicts subsequent depressive symptoms (Butterworth et al., 2009; Butterworth, Cherbuin, Sachdev, & Anstey, 2012). Prospective studies are needed to identify whether and how pregnancy affects experiences of hardship and risk for mental health problems over time. Pregnancy itself may create material hardship. For example, pregnant women may need access to different types of foods, different sized clothing, and more frequent transportation to health care appointments. Pregnancy may also create or exacerbate perceptions of unmet material needs; for example, a woman’s perception of the adequacy of her access to food or the safety of her housing may decline after learning she is pregnant. The current results may be limited by our lack of assessment of potentially relevant variables such as history of depression, duration of time at the annual income level, and gestational age. Possibly, perceptions of hardship vary based on current depression and anxiety. It is also possible that women may have experienced other types of material hardship that affect their antenatal mental health.
From a social determinants of health perspective, antenatal patient care requires a consideration of patient access to resources that directly affect a patient’s ability to thrive during pregnancy. When mental health symptoms reflect distress related to material hardship, addressing unmet social needs may be more effective than mental health treatment. Material hardship also may create barriers to successful engagement in mental health treatment. Our findings support the need for structural competency among providers; that is, patients benefit when providers identify symptoms as well as connections to structural inequalities (Metzl & Hansen, 2014). Our findings also underscore the importance of following expert guidance on antenatal screening for mental health problems (ACOG 2015) and material hardship (ACOG 2018) and for screening results to be included in patient records and as part of clinical care decision-making. For example, providers may “prescribe” contact with social workers who can assist women in obtaining resources to promote a healthy pregnancy (ACOG, 2018). At an organizational level, information about resources to address social needs could be incorporated into standard clinic paperwork. Establishing multidisciplinary teams that include ob/gyn, mental health, and social work clinicians who coordinate care for antenatal patients with mental health problems and unmet social needs may improve outcomes as well as reduce long term costs (Bourgois, Holmes, Sue, & Quesada, 2017). Other innovative approaches to service delivery include medical legal partnerships to address patients’ legal needs (Teufel, Heller, & Dausey, 2014), and co-locating health and social service provisions, such as when health clinics operate food, diaper, and formula pantries (Gottlieb, Sandel, & Adler, 2013).
Practitioners working with low income pregnant women should also consider the indirect effects of hardship on mental health, including how pregnant women perceive and cope with hardship, the effects of hardship on self-appraisals, their views about being mothers or mothers-to-be, and general stress. Community-based psychoeducation and interventions during pregnancy that explicitly incorporate social determinants of health may be important to facilitate women’s coping and self-efficacy. For example, practitioners may normalize stress and stigma related to material hardship, provide information about community resources, and engage in collaborative problem solving to help women access these resources.
In conclusion, a focus on the roles of social determinants of mental health, such as income and material hardship, helps us to expand our understanding of how and why pregnant woman may be vulnerable to mental health problems. The current study suggests that incorporating models of care with pregnant or parenting women that address basic needs (e.g., Healthleadsusa.org) may be important to combat mental health problems and to promote other types of health. This understanding may inform research as well as practice by encouraging scholars and clinicians to attend to the social determinants of mental health during pregnancy.
Acknowledgments
The authors thank Iwona Juskiewicz, MD, MPH for her contributions to this project. This research was supported by Patient Centered Outcomes Research Institute award number AD-12-4261 and by the University of [redacted] CTSA award number UL1 TR000042 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Patient Centered Outcomes Research Institute nor the National Institutes of Health.
Footnotes
The authors report no conflicts of interest.
References
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 630. Screening for perinatal depression. Obstetrics and Gynecology. 2015;125:1268–1271. doi: 10.1097/01.AOG.0000465192.34779.dc. Retrieved from https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Screening-for-Perinatal-Depression. [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 729. Importance of social determinants of health and cultural awareness in the delivery of reproductive health care. Obstetrics and Gynecology. 2018;131:e43–e48. doi: 10.1097/AOG.0000000000002459. Retrieved from https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Importance-of-Social-Determinants-of-Health-and-Cultural-Awareness-in-the-Delivery-of-Reproductive. [DOI] [PubMed] [Google Scholar]
- Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: A systematic review. American Journal of Preventive Medicine. 2010;39:263–272. doi: 10.1016/j.amepre.2010.05.012. [DOI] [PubMed] [Google Scholar]
- Bödecs T, Szilagyi E, Cholnoky P, Sándor J, Gonda X, Rihmer Z, Horváth B. Prevalence and psychosocial background of anxiety and depression emerging during the first trimester of pregnancy: Data from a Hungarian population-based sample. Psychiatria Danubina. 2013;25:352–358. [PubMed] [Google Scholar]
- Bourgois P, Holmes SM, Sue K, Quesada J. Structural vulnerability: Operationalizing the concept to address health disparities in clinical care. Academic Medicine. 2017;92:299–307. doi: 10.1097/ACM.0000000000001294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boushey H, Brocht C, Gundersen B, Bernstein J. Hardships in America: The real story of working families. 2001 http://www.epinet.org/books/hardships.pdf Accessed 26 January 2017.
- Butterworth P, Cherbuin N, Sachdev P, Anstey KJ. The role of hardship in the association between socio-economic position and depression. Australian and New Zealand Journal of Psychiatry. 2012;46:364–373. doi: 10.1177/0004867411433215. [DOI] [PubMed] [Google Scholar]
- Butterworth P, Rodgers B, Windsor TD. Financial hardship, socio-economic position and depression: Results from the PATH through life survey. Social Science & Medicine. 2009;69:229–237. doi: 10.1016/j.socscimed.2009.05.008. [DOI] [PubMed] [Google Scholar]
- Crosier T, Butterworth P, Rodgers B. Mental health problems among single and partnered mothers: The role of financial hardship and social support. Social Psychiatry and Psychiatric Epidemiology. 2007;42:6–13. doi: 10.1007/s00127-006-0125-4. [DOI] [PubMed] [Google Scholar]
- CSDH. Closing the gap in a generation: Health equity through action on the social determinants of health Final report of the Commission on Social Determinants of Health. Geneva: World Health Organization; 2008. http://www.who.int/social_determinants/thecommission/finalreport/en/ Accessed 26 January 2017. [Google Scholar]
- Faisal-Cury A, Menezes PR. Prevalence of anxiety and depression during pregnancy in a private setting sample. Archives of Women’s Mental Health. 2007;10:25–32. doi: 10.1007/s00737-006-0164-6. [DOI] [PubMed] [Google Scholar]
- Fellenzer JL, Cibula DA. Intendedness of pregnancy and other predictive factors for symptoms of prenatal depression in a population based study. Maternal and Child Health. 2014;18:2426–2436. doi: 10.1007/s10995-014-1481-4. [DOI] [PubMed] [Google Scholar]
- Fisher J, Tran T, Duc Tran T, Dwyer T, Nguyen T, Casey GJ, Biggs B. Prevalence and risk factors for symptoms of common mental disorders in early and late pregnancy in Vietnamese women: A prospective population-based study. Journal of Affective Disorders. 2013;146:213–219. doi: 10.1016/j.jad.2012.09.007. [DOI] [PubMed] [Google Scholar]
- Flynn HA, Sexton M, Ratliff S, Porter K, Zivin K. Comparative performance of the Edinburgh Postnatal Depression Scale and the Patient Health Questionnaire-9 in pregnant and postpartum women seeking psychiatric services. Psychiatry Research. 2011;187:130–134. doi: 10.1016/j.psychres.2010.10.022. [DOI] [PubMed] [Google Scholar]
- Gottlieb L, Sandel M, Adler NE. Collecting and applying data on social determinants of health in health care settings. JAMA Internal Medicine. 2013;173:1017–1020. doi: 10.1001/jamainternmed.2013.560. [DOI] [PubMed] [Google Scholar]
- Grote NK, Bridge JA, Gavin AR, Melville JL, Ivengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Archives of General Psychiatry. 2010;67:1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- Heflin CM, Corcoran ME, Siefert KA. Work trajectories, income changes, and food insufficiency in a Michigan welfare population. Social Service Review. 2007;81:3–25. http://www.jstor.org/stable/10.1086/511162. [Google Scholar]
- Heflin CM, Iceland J. Poverty, material hardship, and depression. Social Science Quarterly. 2009;90:1051–1071. doi: 10.1111/j.1540-6237.2009.00645.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Kendler KS. Lifetime and 12-month prevalence of DSM-III—R psychiatric disorders in the United States: Results from the national comorbidity study. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Koleva H, Stuart S, O’Hara MW, Bowman-Reif J. Risk factors for depressive symptoms during pregnancy. Archives of Women’s Mental Health. 2011;14:99–105. doi: 10.1007/s00737-010-0184-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 - validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j1525-14972001016009606x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Lynch J, Smith GD, Harper S, Hillemeier M, Ross N, Kaplan GA, Wolfson M. Is income inequality a determinant of population health? part 1. A systematic review. Milbank Quarterly. 2004;82:5–99. doi: 10.1111/j.0887-378X.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch JW, Smith GD, Kaplan GA, House JS. Income inequality and mortality: Importance to health of individual income, psychosocial environment, or material conditions. British Medical Journal. 2000;320:1200–1204. doi: 10.1136/bmj.320.7243.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Målqvist M, Clarke K, Matsebula T, Bergman M, Tomlinson M. Screening for antepartum depression through community health outreach in Swaziland. Journal of Community Health. 2016;41:946–952. doi: 10.1007/s10900-016-0175-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus SM. Depression during pregnancy: Rates, risks and consequences – mother risk Update 2008. Canadian Journal of Clinical Pharmacology. 2009;16:e15–e22. [PubMed] [Google Scholar]
- Mechanic D. Rediscovering the social determinants of health. Health Affairs. 2001;19:269–276. doi: 10.1377/hlthaff.19.3.269. [DOI] [Google Scholar]
- Metzl JM, Hansen H. Structural competency: Theorizing a new medical engagement with stigma and inequality. Social Science and Medicine. 2014;103:126–133. doi: 10.1016/j.socscimed.2013.06.032. doi: 10.1016%2Fj.socscimed.2013.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntaner C, Eaton WW, Miech R, O’Campo P. Socioeconomic position and major mental disorders. Epidemiologic Review. 2004;26:53–62. doi: 10.1093/epirev/mxh001. [DOI] [PubMed] [Google Scholar]
- Norhayati MN, Hazlina NHN, Asrenee AR, Emilin WMA. Magnitude and risk factors for postpartum symptoms: A literature review. Journal of Affective Disorders. 2015;175:34–52. doi: 10.1016/j.jad.2014.12.041. [DOI] [PubMed] [Google Scholar]
- Räisänen S, Lehto SM, Nielsen HS, Gissler M, Kramer MR, Heinonen S. Risk factors for and perinatal outcomes of major depression during pregnancy: A population-based analysis during 2002-2010 in Finland. BMJ Open. 2014;4:1–8. doi: 10.1136/bmjopen-2014-004883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich-Edwards J, Kleinman K, Abrams A, Harlow BL, McLaughlin TJ, Joffe H, Gillman MW. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. Journal of Epidemiology and Community Health. 2006;60:221–227. doi: 10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Save the Children. State of the world’s mothers: The urban disadvantage. 2015 Retrieved from www.savethechildren.org. Accessed 16 March 2017.
- Sidebottom A, Harrison PA, Godecker AL, Kim H. Validation of the patient health screening questionnaire (PHQ-9) for prenatal depression screening. Archives of Women’s Mental Health. 2012;15:367–374. doi: 10.1007/s00737-012-0295-x. [DOI] [PubMed] [Google Scholar]
- World Health Organization and Calouste Gulbenkian Foundation. Social determinants of mental health Geneva. World Health Organization; 2014. Retrieved from http://apps.who.int/iris/bitstream/10665/112828/1/9789241506809_eng.pdf. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Teufel J, Heller SM, Dausey DJ. Medical-legal partnerships as a staregy to improve social causes of stress and disease. American Journal of Public Health. 2014;104:e6–e7. doi: 10.2105/AJPH.2014.302268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Q, Gelaye B, Rondon MB, Sanchez SE, Barrios YV, Simon GE, Henderson DC, Cripe SM, Williams MA. Comparative performance of Patient Health Questionnaire-9 and Edinburgh Postnatal Depression Scale for screening antepartum depression. Journal of Affective Disorders. 2014;162:1–7. doi: 10.1016/j.jad.2014.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong QY, Gelaye B, Zaslavsky AM, Fann JR, Rondon MB, Sanchez SE, Williams MA. Diagnostic validity of the Generalized Anxiety Disorder-7 (GAD-7) among pregnant women. PLoS One. 2015;10:e0125096. doi: 10.1371/journal.pone.0125096. [DOI] [PMC free article] [PubMed] [Google Scholar]


