Abstract
Purpose:
Binocular summation (BiS) occurs when binocular visual function surpasses that of the better eye alone. We sought to evaluate whether strabismic amblyopia reduces BiS more than strabismus alone, and determine whether BiS improves in strabismic amblyopes after strabismus surgery.
Methods:
We prospectively recruited 15 patients with strabismic amblyopia who then underwent strabismus surgery. Thirty age-matched normal subjects and 30 non-amblyopic strabismic patients served as controls. Subjects underwent binocular and monocular visual acuity testing on high-contrast Early Treatment Diabetic Retinopathy Study (ETDRS) as well as 2.5% and 1.25% Sloan low contrast acuity (LCA) charts. BiS was calculated as the difference between better eye and binocular scores.
Results:
Strabismic amblyopes and strabismic controls did not significantly differ in preoperative BiS, but both had subnormal BiS preoperatively on LCA charts. Among 11 strabismic amblyopes with preoperative and postoperative BiS measurements, average postoperative BiS was not significantly different from preoperative. Improved LCA BiS postoperatively occurred in some patients and was associated with measurable preoperative stereoacuity (p = 0.02), older age at strabismus onset (p = 0.02), and larger preoperative angle of strabismus (p = 0.0043).
Conclusions:
In this preliminary study, strabismic amblyopes experienced subnormal BiS, but amblyopia generally did not further impair BiS beyond that due to strabismus alone. Some strabismic amblyopes experienced improved low-contrast BiS after strabismus surgery. This suggests that further investigations in larger groups of patients should be undertaken to analyze a previously unrecognized functional benefit of strabismus surgery in strabismic amblyopes.
Keywords: Amblyopia, binocularity, strabismus, strabismus surgery, stereopsis
INTRODUCTION
Binocular summation (BiS) occurs when visual function when viewing with both eyes is superior to the better eye alone,7, 23 and is best demonstrated at low contrast.4, 24 Studies have previously shown that strabismus is associated with diminished binocular summation,23, 27 but can improve in some cases after strabismus surgery.22 Moreover, decreased binocular summation in strabismic patients is associated with worse quality of life, emphasizing the importance of improving binocularity.29 Our previous studies, however, deliberately excluded patients with strabismic amblyopia because of known impairment by amblyopia of binocular summation,11, 28 and it is unknown if amblyopia further degrades binocular summation beyond that due to strabismus alone.
Prior investigators have established that both strabismic and anisometropic amblyopia are associated with decreased binocular summation.11, 14, 15, 20, 21, 28 However, a growing body of evidence suggests that the visual system in amblyopes may retain structural binocularity, despite being functionally monocular due to suppression from the fellow eye.4 For example, when visual acuity and contrast are balanced between the eyes by diminishing luminance for better eye, binocular summation improves to normal in strabismic amblyopes.5 This evidence for preserved binocularity in amblyopes is the basis for dichoptic treatment of amblyopia,10 and also raises the question of whether BiS can improve in strabismic amblyopes with strabismus surgery.
In this preliminary study, we sought to determine whether BiS in strabismic amblyopes is more decreased than in strabismus alone. Additionally, we evaluated whether strabismus surgery in strabismic amblyopes improves BiS, and if so, which factors are associated with improvement.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of the University of California, Los Angeles, and conformed to the requirements of the US Health Insurance Portability and Accountability Act and the Declaration of Helsinki. Fifteen patients with strabismic amblyopia due to esotropia or exotropia were consecutively recruited from September 1, 2014, to February 28, 2016, from the preoperative clinics of four of the coauthors (M.Y.C., J.L.D., F.G.V., and S.J.I.). Strabismic controls without amblyopia were recruited from the same clinics from 2011 to 2013. Patients were included if age at surgery was between 3 and 65 years, and visual acuity in amblyopic eyes was between 20/40 and 20/200. Visual acuity was required to be 20/40 or worse because interocular difference in visual acuity is related to the degree of binocularity,2 and prior studies that demonstrated preserved binocular summation in strabismic amblyopes included visual acuity in this range.5 Additionally, 20/200 was the worst vision acceptable for this study due to the requirement for patients to read the ETDRS chart at standard distance in order to calculate BiS. We did not include patients with dissociated deviation as the only form of strabismus, nystagmus, or neurologic disease. Dissociated strabismus was excluded owing to the difficulty in obtaining accurate measurements of the deviation. Strabismic controls without history of amblyopia but with interocular visual acuity difference exceeding 10 ETDRS letters (2 lines) were excluded due to the possibility of undiagnosed amblyopia. Strabismic amblyopes and controls who missed their post-operative visits were included in comparisons of preoperative binocular summation, but excluded from analyses of postoperative change in binocular summation. Nonstrabismic control participants were recruited from among staff at the Stein Eye Institute, as well as family members of patients seen between 2010 and 2011. Control participants were included only if they had no history of ocular disease other than refractive error.
Strabismic and nonstrabismic controls were recruited as part of a larger study on binocular summation. For each of the normal and strabismic control groups, two controls were selected for each amblyopic patient. Normal controls were matched to amblyopic patients based on age. Strabismic controls were matched based on distance angle of strabismus and subtype of strabismus; if multiple controls were available based on these criteria, the control subject closest in age was selected. The following data were collected for strabismic participants: strabismus subtype, age of onset of strabismus, age at which strabismus surgery was performed, and presence or absence of diplopia. Age of onset of strabismus was established by history divulged by the patient or parent, in the case of younger children.
All subjects underwent measurement of best-corrected visual acuity (VA) using the Early Treatment Diabetic Retinopathy Study (ETDRS) protocol1 at 3 m in a dimly lit room. The maximum possible score was 100 letters (Snellen equivalent, 20/12.5). Young subjects untestable with the ETDRS chart were tested with Lea symbols on an ETDRS-style chart (Precision Vision, La Salle, IL) at 3 m. Testing was performed by trained technicians experienced in research studies with standard protocols. Right eye, left eye, and binocular visual acuities were measured at high- and low-contrast. Testing order (right eye, left eye, or binocular) was randomly assigned and maintained for each subject. Tests were performed preoperatively within 1 month of surgery and 6 to 10 weeks postoperatively. Low-contrast visual acuity was tested using Sloan acuity charts (Precision Vision, La Salle, IL) at 3 m at contrast levels of 2.5% and 1.25%. Sloan charts had format similar to the ETDRS charts (5 letters per line). The maximum low-contrast acuity (LCA) score was 100 letters.
Binocular alignment was measured at far (6m) and near (30 cm) using cover/uncover and alternate prism cover testing. Distance and near stereoacuity were evaluated using the Randot Stereotest (Stereo Optical Co., Chicago, Il).
Analysis
Binocular summation (BiS) was calculated by subtracting the better eye score from the binocular score in number of chart letters. A BiS score greater than 0 indicates the presence of binocular summation, while a score less than 0 signifies binocular inhibition, in which visual acuity with both eyes viewing is worse than the better eye alone. BiS in strabismic amblyopes was compared to that of normal and strabismic controls using two-tailed t tests. Preoperative and postoperative BiS scores were compared using the Wilcoxon test. Linear regression was used to evaluate the effect of continuous variables on change in BiS (difference between post- and preoperative scores). The Mann Whitney test was used for dichotomous variables, and the Kruskal Wallis test was used for non-dichotomous categorical variables. Surgical success was defined as distance horizontal deviation less than 10 prism diopters (PD) and vertical deviation less than 4 PD.
Variables significant on univariate analysis were included in multiple regression analysis. P values less than 0.05 were deemed statistically significant.
RESULTS
Demographic and Clinical Features
Fifteen strabismic amblyopes were recruited, as well as 30 age-matched normal controls and 30 strabismic controls. Demographic and clinical characteristics are summarized in Table 1. There were no significant age differences among groups. Normal controls, but not strabismic controls, had significantly better binocular visual acuity compared to strabismic amblyopes (p = 0.0014). The mean (SD) interocular difference in visual acuity was 14 (9) letters in strabismic amblyopes; 3.6 (2.4) letters in normal controls (p < 0.0001, strabismic amblyopes vs. normal controls); and 3.8 (4.2) letters in strabismic controls (p < 0.0001, strabismic amblyopes vs. strabismic controls). The mean absolute angle of horizontal strabismus at distance was 26.5 PD in both strabismic amblyopes and strabismic controls. Two patients (13%) in the strabismic amblyopia group reported subjective diplopia, not significantly different from 8 (27%) strabismic controls. Four strabismic amblyopes were lost to follow-up after strabismus surgery, so 11 strabismic amblyopes had follow-up data available at 2 months postoperatively. The patients who were lost to follow-up did not differ from the other strabismic amblyopes on any preoperative measure, including age, binocular visual acuity, preoperative BiS on any chart, interocular difference in acuity, preoperative angle of strabismus, strabismus subtype, and presence or absence of stereoacuity or diplopia. All 22 matched strabismic controls completed 2 month postoperative follow-up visits.
Table 1.
Preoperative Data.
| Strabismic Amblyopes (n = 15) |
Normal Controls (n = 30) |
Strabismic Controls (n = 30) |
|
|---|---|---|---|
| Mean age in years (range, SD) | 30 (5–63, 21) | 31 (3–63, 20) |
22 (4–57, 15) |
| Mean binocular visual acuity, number of ETDRS letters (SD) | 81 (10) | 88 (5) p = 0.0014* |
83 (11) p = 0.58 |
| Mean interocular difference in visual acuity, number of ETDRS letters (SD) | 14 (9.0) | 3.6 (2.4) p < 0.0001* |
3.8 (4.2) p < 0.0001* |
| Mean angle of strabismus at distance, prism diopters (SD) | 26.5 (13.6) | 0 | 26.5 (13.0) p = 0.99 |
The subtypes of strabismus represented in each strabismic group included infantile esotropia (27%), childhood esotropia (33%), consecutive exotropia (27%), and intermittent exotropia (13%). There was no difference in distribution of strabismus subtypes between the strabismic amblyopia and control groups.
Preoperative Binocular Summation
Binocular summation scores for all subjects are displayed in Fig. 1. On the high-contrast ETDRS or Lea charts, BiS was only slightly greater than zero but did not significantly differ among subject groups (p > 0.08). Normal controls demonstrated mean (standard error of mean, SEM) BiS of 5.7 (0.93) letters on the 2.5% LCA chart, and 5.4 (1.1) letters on the 1.25% LCA chart. In normal controls, BiS for low contrast acuity was significantly greater than zero (p < 0.0001 for both charts), and also significantly better than in preoperative strabismic amblyopes and strabismic controls (p < 0.03). Low contrast acuity BiS in preoperative strabismic amblyopes and strabismic controls was not significantly different from zero (p > 0.10), indicating neither binocular summation nor binocular inhibition. There was no difference in low contrast BiS between strabismic amblyopes and strabismic controls (p > 0.09).
Figure 1.
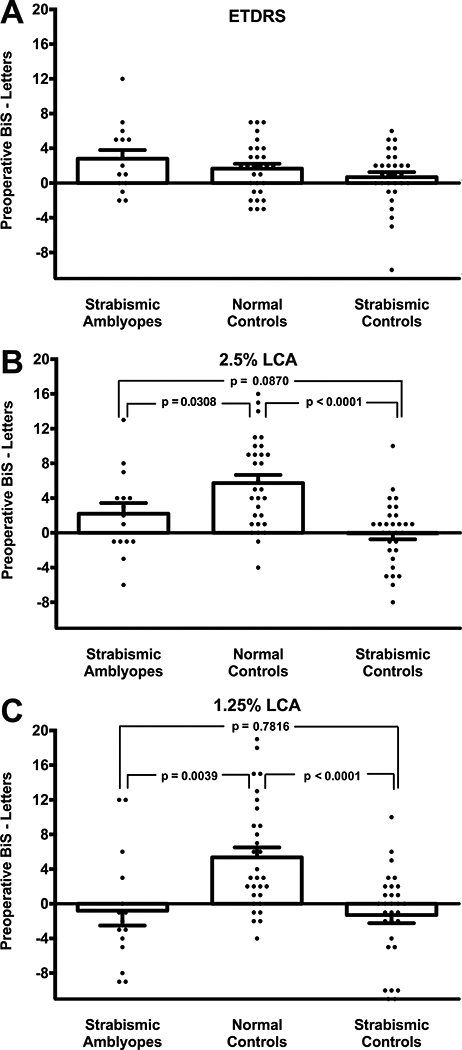
Mean preoperative binocular summation (BiS) for high-contrast Early Treatment of Diabetic Retinopathy Study (ETDRS) acuity (A), 2.5% low-contrast acuity (LCA, B), and 1.25% LCA (C). Error bars indicate standard error of mean.
Postoperative Binocular Summation
Mean postoperative change in BiS (post-minus preoperative score) in strabismic amblyopes is compared with strabismic controls in Figure 2. Postoperative BiS was not significantly different from preoperative in either group on any chart, except in strabismic controls on the 2.5% LCA chart (mean preoperative BiS of −0.41 letters (SEM 0.86) improved postoperatively to 2.2 letters (SEM 0.97, p = 0.02)). Among strabismic amblyopes, postoperative change in BiS ranged from −12 to +11 letters for 2.5% LCA, and −14 to +15 letters for 1.25% LCA, indicating that some patients experienced improved BiS after surgery, while others experienced worsening, and on average there was no change.
Figure 2.
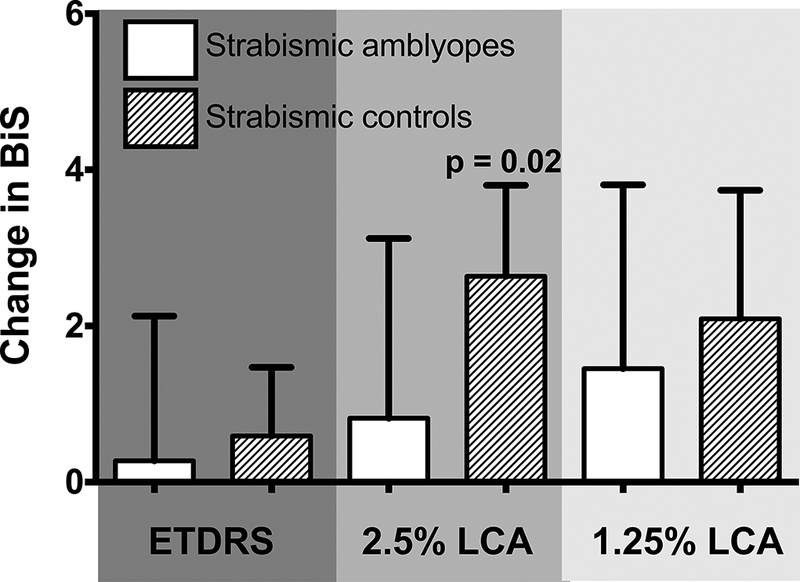
Postoperative change in binocular summation (BiS) in strabismic amblyopes and strabismic controls for high-contrast Early Treatment of Diabetic Retinopathy Study (ETDRS) acuity, 2.5% low-contrast acuity (LCA), and 1.25% LCA. Error bars indicate standard error of mean.
Factors Associated with Improved Postoperative Binocular Summation in Strabismic Amblyopes
Postoperative change in high-contrast BiS was not associated with any of the clinical variables evaluated, including presence of measurable stereoacuity, interocular difference (IOD) in visual acuity, age of surgery, age of onset of strabismus, angle of strabismus, and strabismus subtype (Figs. 3–5). The only factor significantly associated with improved 2.5% LCA BiS postoperatively was presence of measurable stereoacuity preoperatively (p = 0.02, Fig. 3).
Figure 3.
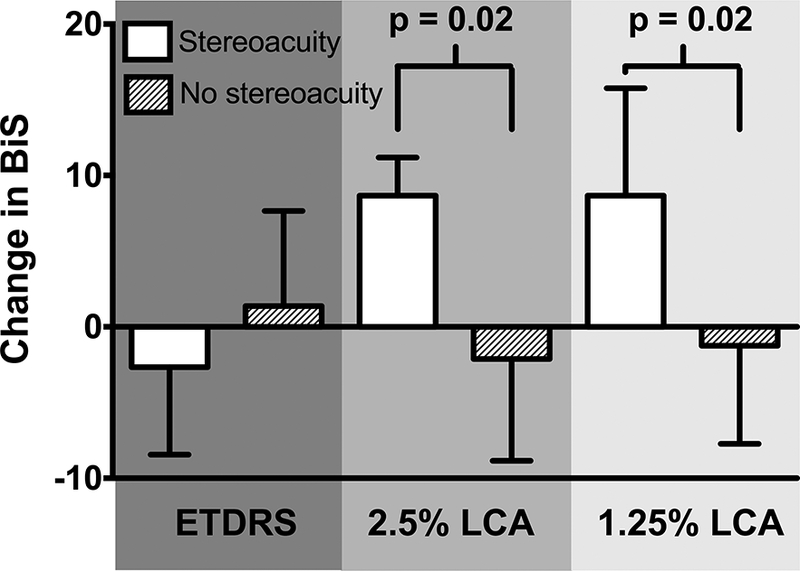
Mean postoperative change in binocular summation (BiS) in patients with and without measurable stereoacuity preoperatively at distance or near for high-contrast Early Treatment of Diabetic Retinopathy Study (ETDRS) acuity, 2.5% low-contrast acuity (LCA), and 1.25% LCA. Error bars indicate standard error of mean.
Figure 5.
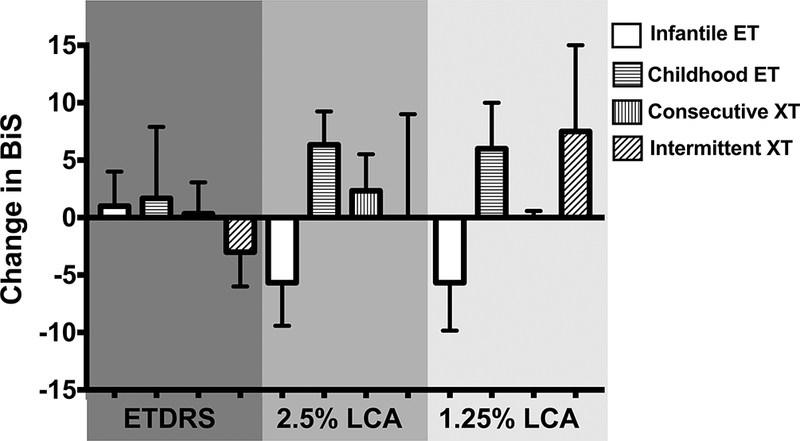
Mean postoperative change in binocular summation (BiS) in strabismic amblyopes by strabismus subtype for high-contrast Early Treatment of Diabetic Retinopathy Study (ETDRS) acuity, 2.5% low-contrast acuity (LCA), and 1.25% LCA. Error bars indicate standard error of mean. There was no significant effect of strabismus subtype on postoperative change in BiS on any chart.
On univariate analysis, variables significantly associated with improved postoperative 1.25% LCA BiS included measurable stereoacuity preoperatively (p = 0.02, Fig. 3); older age of strabismus onset (p = 0.02, Fig. 4C); and larger preoperative angle of strabismus at distance (p = 0.004, Fig. 4D). On multiple regression analysis, the only factor that remained significantly associated with improved BiS postoperatively on the 1.25% LCA chart was presence of measurable stereoacuity preoperatively.
Figure 4.
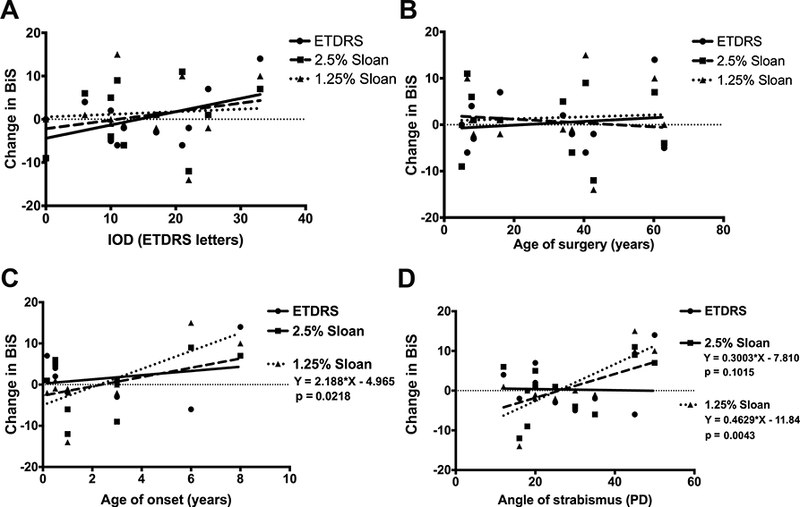
Linear regression models for change in binocular summation (BiS) in strabismic amblyopes on high-contrast Early Treatment of Diabetic Retinopathy Study (ETDRS) acuity, 2.5% low-contrast acuity (LCA), and 1.25% LCA. Variables evaluated included: A) interocular difference (IOD) in visual acuity; B) age of strabismus surgery; C) age of onset of strabismus; and D) preoperative angle of strabismus at distance.
There was no significant effect of IOD in visual acuity (Fig. 4A), age at strabismus surgery (Fig. 4B), or strabismus subtype (Fig. 5) on change in BiS for any condition.
All strabismic amblyopes met the definition of surgical success, so the effect of surgical success or failure on change in BiS could not be evaluated.
Factors Associated with Worse Postoperative Binocular Summation in Strabismic Amblyopes
Of three strabismic amblyopes who experienced postoperative worsening of BiS of 5 letters or more on LCA charts, one was a child who had intermittent exotropia with no vertical deviation preoperatively and developed a small hypertropia of 3 PD after surgery. The second was an adult with infantile esotropia whose postoperative deviation was 8 PD of exotropia. Finally, the third patient was an adult with consecutive exotropia whose deviation measured 2 PD of esotropia after surgery.
DISCUSSION
Our study confirms prior findings of diminution in low-contrast BiS in amblyopic and non-amblyopic strabismic patients.11, 23 The current study extends these findings to show that strabismic amblyopes have binocular summation at low contrast similar to subjects with strabismus alone, suggesting that amblyopia did not further reduce binocular summation beyond that due to strabismus. There was no significant change in average BiS postoperatively in strabismic amblyopes.
Our finding that strabismic amblyopes did not have worse binocular summation than non-amblyopic strabismic patients suggests that there was no additive decremental effect of strabismus and amblyopia on BiS. The reduction in BiS associated with amblyopia is believed related to interocular differences in visual acuity and contrast sensitivity.2, 17, 20 In strabismus, we theorize that decreased BiS is related to the effective decrease in visual acuity in the deviated eye when viewing eccentrically.23, 27 It is likely that the decrement in visual acuity related to non-foveal viewing was greater than the reduction in visual acuity due to amblyopia in our cohort. The decline in acuity due to eccentric viewing can be estimated based on the work of Ludvigh, who found that viewing at 10° eccentric to the fovea reduced visual acuity from approximately 20/12 to 20/80 corresponding to about 8 ETDRS lines.16 The mean distance angle of strabismus in both of our strabismic groups was greater than this at 26.5 PD, or 14.8°, and therefore would correspond to even further reduction in acuity. By comparison, the mean IOD in visual acuity in the strabismic amblyopia group was 14 letters, or about 3 ETDRS lines. The greater reduction in acuity caused by non-foveal viewing probably rendered insignificant the contribution of amblyopia to interocular acuity difference, creating a floor effect for BiS in strabismic amblyopia compared to strabismus alone. If this is the case, BiS might be more affected by amblyopia than strabismus only in patients with a smaller strabismic angle and deeper amblyopia.
In keeping with previous studies suggesting intact neural mechanisms for binocularity in amblyopes,5, 11 we found that some patients with strabismic amblyopia experienced improved binocular summation after strabismus surgery. Evidence for intact binocular function in amblyopes stems from experiments in which neutral density filters or Bangerter filters over the fellow eye reduced interocular difference in visual acuity and contrast, and resulted in normal binocular summation in both strabismic and anisometropic amblyopes.5, 8 Binocular oculomotor responses in amblyopes may also improve with reduction in contrast for the better eye.25 Raveendran et al found that balanced contrast resulted in improved fixational stability of the amblyopic eye during binocular viewing.25 Additionally, these investigators found that bifoveal fixation established using a haploscope also improved fixational stability of the amblyopic eye under binocular conditions. However, bifoveal fixation could only be transiently maintained with this technique.25
In our study, although there was on average no significant change in BiS postoperatively in strabismic amblyopes, some subgroups of patients did show improvement, particularly those with measurable stereoacuity preoperatively. To our knowledge, ours is the first study to show improvement on a binocular measure in strabismic amblyopes after strabismus surgery. Although Mollenhauer and Haase found that dynamic stereopsis improved after strabismus surgery in some strabismic patients, they did not separately analyze those with amblyopia but reported that 42% of patients had no dynamic stereopsis before or after surgery, and this group included many patients with severe amblyopia.18 We previously found that some non-amblyopic strabismic patients experience improved binocular summation after strabismus surgery, and hypothesized that this was related to improved relative visual acuity in the deviated eye with foveal rather than eccentric viewing.22 We believe that this mechanism may also apply to the strabismic amblyopes in our cohort whose binocular summation scores improved after surgery.
Stereoacuity was the only association with improved low contrast BiS in strabismic amblyopes that was significant on multiple regression analysis, and was also the only variable to show significant improvement in BiS for both 2.5% and 1.25% LCA. We previously demonstrated significant correlation between stereoacuity and low contrast binocular summation after strabismus surgery.13 In the current study, some strabismic amblyopes demonstrated measurable stereoacuity without BiS preoperatively, and experienced improvement of LCA BiS with strabismus surgery. This suggests that although stereoacuity and LCA BiS are correlated, they may be differentially affected by strabismus. Preoperative measurements of BiS in addition to stereoacuity may be useful to assess response to strabismus surgery, even in amblyopes.
Older onset of strabismus was associated with more postoperative improvement in binocular summation for 1.25% LCA. Prior investigations have shown that in normal subjects, younger age is associated with greater levels of binocular summation.19, 24 Other measures of binocularity, such as stereopsis and fusion, have critical periods of development, such that early disruption by strabismus causes permanent binocular sensory deficits.6, 9, 12 Although the deficits in binocular summation in both strabismus and amblyopia are reversible to some extent (with strabismus surgery and reduction of the interocular difference in acuity, respectively),5, 22 the degree of reversibility may be related to age of onset.
Patients with a larger preoperative angle of strabismus also experienced more improvement in binocular summation postoperatively on 1.25% LCA charts. Since all horizontal devitions in strabismic amblyopes were corrected to within 10 PD of orthotropia, larger preoperative angle of strabismus corresponded to a greater postoperative change in the angle of strabismus. As discussed previously, we theorize that the decrement in binocular summation in strabismic patients is due to the relative decreased visual acuity of the deviated eye with eccentric viewing and a form of an induced interocular difference.23 Previous studies have shown that visual acuity progressively worsens with increased eccentricity of viewing.3, 16 Therefore, the patients with the largest angle of strabismus preoperatively likely had the greatest decrement in visual acuity from eccentric viewing, and the most improvement in effective visual acuity with foveal fixation. This would translate to less interocular difference in visual acuity postoperatively, and more improvement in binocular summation scores.
Three strabismic amblyopes experienced worse LCA BiS after surgery. Of these, one patient had intermittent exotropia without a preoperative vertical deviation and developed a 3 PD hypertropia after surgery, and two patients had horizontal deviations preoperatively which reversed direction after surgery (overcorrection). None of the other patients experienced change in direction of strabismus postoperatively. It is possible that changing the direction of strabismus altered the pattern of retinal correspondence, resulting in more inhibition from the amblyopic eye than before surgery. Prior investigators have demonstrated that patients who experience a change in the direction of strabismus are more likely to have altered retinal correspondence after surgery.26
This study has several limitations. Because our study was preliminary, designed to introduce the concept that strabismus surgery may improve BiS in some amblyopes, the study size was small. This may have limited our ability to detect small differences among study groups. Additionally, given the small sample size and preliminary nature of our study, statistical correction for multiple comparisons was not performed. This may cause overestimation of some effects. Furthermore, the age of onset of strabismus was established by patient history, which is liable to uncertainty especially in the case of adults with childhood onset of strabismus. However, of the eight adults included in this study, five had either infantile esotropia or consecutive exotropia, for which the timing of strabismus onset could be established fairly accurately as less than 12 months of age or the date of surgery, respectively.
In conclusion, we report that while strabismic amblyopes and non-amblyopic strabismic patients have subnormal BiS at low contrast, strabismic amblyopes have BiS no worse than with strabismus alone. Strabismus surgery may improve low-contrast BiS in some patients with strabismic amblyopia. This suggests that further investigations in larger groups of patients should be undertaken to analyze a previously unrecognized functional benefit of strabismus surgery in strabismic amblyopes. If such a benefit is validated by future studies, it may influence counseling of patients with strabismic amblyopia who are considering whether to undergo surgery.
Acknowledgments
Financial disclosures: SLP - NIH/NEI Grant K23EY021762, Research to Prevent Blindness, Walt and Lily Disney Award for Amblyopia Research, Knights Templar Eye Foundation, Oppenheimer Family Foundation. JLD - NIH Grant EY008313.
REFERENCES
- 1.Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics. ETDRS report number 7. Ophthalmology 1991;98:741–56. [DOI] [PubMed] [Google Scholar]
- 2.Agrawal R, Conner IP, Odom JV, Schwartz TL, Mendola JD. Relating binocular and monocular vision in strabismic and anisometropic amblyopia. Arch Ophthalmol 2006;124:844–50. [DOI] [PubMed] [Google Scholar]
- 3.Anstis SM. Letter: A chart demonstrating variations in acuity with retinal position. Vision Res 1974;14:589–92. [DOI] [PubMed] [Google Scholar]
- 4.Baker DH, Meese TS, Hess RF. Contrast masking in strabismic amblyopia: attenuation, noise, interocular suppression and binocular summation. Vision Res 2008;48:1625–40. [DOI] [PubMed] [Google Scholar]
- 5.Baker DH, Meese TS, Mansouri B, Hess RF. Binocular summation of contrast remains intact in strabismic amblyopia. Invest Ophthalmol Vis Sci 2007;48:5332–8. [DOI] [PubMed] [Google Scholar]
- 6.Birch EE. Marshall Parks lecture. Binocular sensory outcomes in accommodative ET. J AAPOS 2003;7:369–73. [DOI] [PubMed] [Google Scholar]
- 7.Campbell FW, Green DG. Monocular versus binocular visual acuity. Nature 1965;208:191–2. [DOI] [PubMed] [Google Scholar]
- 8.Chen Z, Li J, Thompson B, et al. The effect of Bangerter filters on binocular function in observers with amblyopia. Invest Ophthalmol Vis Sci 2015;56:139–49. [DOI] [PubMed] [Google Scholar]
- 9.Fawcett SL, Wang YZ, Birch EE. The critical period for susceptibility of human stereopsis. Invest Ophthalmol Vis Sci 2005;46:521–5. [DOI] [PubMed] [Google Scholar]
- 10.Hess RF, Mansouri B, Thompson B. Restoration of binocular vision in amblyopia. Strabismus 2011;19:110–8. [DOI] [PubMed] [Google Scholar]
- 11.Hess RF, Thompson B, Baker DH. Binocular vision in amblyopia: structure, suppression and plasticity. Ophthalmic Physiol Opt 2014;34:146–62. [DOI] [PubMed] [Google Scholar]
- 12.Hohmann A, Creutzfeldt OD. Squint and the development of binocularity in humans. Nature 1975;254:613–4. [DOI] [PubMed] [Google Scholar]
- 13.Kattan JM, Velez FG, Demer JL, Pineles SL. Relationship Between Binocular Summation and Stereoacuity After Strabismus Surgery. Am J Ophthalmol 2016;165:29–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lema SA, Blake R. Binocular summation in normal and stereoblind humans. Vision Res 1977;17:691–5. [DOI] [PubMed] [Google Scholar]
- 15.Levi DM, Harwerth RS, Smith EL. Binocular interactions in normal and anomalous binocular vision. Doc Ophthalmol 1980;49:303–24. [DOI] [PubMed] [Google Scholar]
- 16.Ludvigh E Extrafoveal visual acuity as measured with Snellen test-letters. Am J Ophthalmol 1941;24:303–310. [Google Scholar]
- 17.Mansouri B, Thompson B, Hess RF. Measurement of suprathreshold binocular interactions in amblyopia. Vision Res 2008;48:2775–84. [DOI] [PubMed] [Google Scholar]
- 18.Mollenhauer KA, Haase W. Preliminary report: Dynamic stereopsis in patients with impaired binocular function. Strabismus 2000;8:275–81. [DOI] [PubMed] [Google Scholar]
- 19.Pardhan S A comparison of binocular summation in the peripheral visual field in young and older patients. Curr Eye Res 1997;16:252–5. [DOI] [PubMed] [Google Scholar]
- 20.Pardhan S, Gilchrist J. Binocular contrast summation and inhibition in amblyopia. The influence of the interocular difference on binocular contrast sensitivity. Doc Ophthalmol 1992;82:239–48. [DOI] [PubMed] [Google Scholar]
- 21.Pardhan S, Whitaker A. Binocular summation in the fovea and peripheral field of anisometropic amblyopes. Curr Eye Res 2000;20:35–44. [PubMed] [Google Scholar]
- 22.Pineles SL, Demer JL, Isenberg SJ, Birch EE, Velez FG. Improvement in binocular summation after strabismus surgery. JAMA Ophthalmol 2015;133:326–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pineles SL, Velez FG, Isenberg SJ, et al. Functional burden of strabismus: decreased binocular summation and binocular inhibition. JAMA Ophthalmol 2013;131:1413–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pineles SL, Velez FG, Yu F, Demer JL, Birch E. Normative reference ranges for binocular summation as a function of age for low contrast letter charts. Strabismus 2014;22:167–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raveendran RN, Babu RJ, Hess RF, Bobier WR. Transient improvements in fixational stability in strabismic amblyopes following bifoveal fixation and reduced interocular suppression. Ophthalmic Physiol Opt 2014;34:214–25. [DOI] [PubMed] [Google Scholar]
- 26.Rutstein RP, Marsh-Tootle W, Scheiman MM, Eskridge JB. Changes in retinal correspondence after changes in ocular alignment. Optom Vis Sci 1991;68:325–30. [DOI] [PubMed] [Google Scholar]
- 27.Sireteanu R Binocular vision in strabismic humans with alternating fixation. Vision Res 1982;22:889–96. [DOI] [PubMed] [Google Scholar]
- 28.Sireteanu R, Fronius M, Singer W. Binocular interaction in the peripheral visual field of humans with strabismic and anisometropic amblyopia. Vision Res 1981;21:1065–74. [DOI] [PubMed] [Google Scholar]
- 29.Tandon AK, Velez FG, Isenberg SJ, Demer JL, Pineles SL. Binocular inhibition in strabismic patients is associated with diminished quality of life. J AAPOS 2014;18:423–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


