Highlights
-
•
PMMA-based bone cement proved effective in esthetic smile rehabilitation.
-
•
The technique is operator-sensitive.
-
•
The thickness of the PMMA implant is also paramount.
-
•
PMMA is non-toxic, biocompatible with human tissues.
Keywords: Case report, Gummy smile, PMMA, Surgery
Abstract
Introduction
One of the most common esthetic complaints among dental patients is a gingival smile, which may be of multifactorial etiology, e.g. gingival hyperplasia, skeletal deformities featuring overgrowth of the anterior maxilla, altered passive eruption, maxillary alveolar tooth extrusion, fine lip and hypermobility of lip elevator muscles, which must be diagnosed prior to treatment so that the appropriate management approach can be selected. Maxillary overgrowth may give rise to subnasal skeletal depression where the upper lip retracts to during smiling, causing gingival exposure. The objective of this case report was to describe a lip repositioning technique using polymethylmethacrylate (PMMA)-based bone cement for esthetic smile rehabilitation.
Case report
A 23-year-old female attended the Esthetic Dentistry Clinic of our institute, reporting dissatisfaction with her smile, due to the size of her teeth and the amount of gingiva exposed when smiling. A rehabilitation planning was designed, which was performed with periodontal surgical intervention to fill the subnasal depression with PMMA-based bone cement. After crown lengthening, the PMMA-based bone cement was prepared with gentamicin in a sterile surgical bowl. When the mixture stopped sticking to the surgical gloves, it was then positioned into the subnasal pit, under constant and copious saline irrigation. With the cement in place, the prosthesis was shaped in a maximum thickness of 7-mm. After complete polymerization and under abundant cooling, refinement and finishing of the PMMA prosthesis was performed. The prosthesis was fixed onto the bone with two titanium-based bone graft fixation screws. The smile aesthetic rehabilitation was complemented using 10 lithium disilicate-based ceramic veneers.
Discussion and conclusion
PMMA-based bone cement proved effective when combined to clinical crown lengthening for esthetic smile rehabilitation, acting as a filling material for subnasal depression, providing new lip support.
1. Introduction
The esthetic evaluation of a patient should include extra-oral, labial, periodontal and dental examination. The so-called beautiful attractive and healthy smile is a balance between the shape and symmetry of the teeth, lips and gingival tissues, as well as the way they relate and harmonize with the patient’s face [1]. The assessment of the frontal and lateral views of the aforementioned structures should be peformed aiming at determining labial positioning, vertical dimension and delimiting the facial proportions [2].
A gingival smile is one of the most common complaints among patients seeking esthetic rehabilitation treatment, and indication for correction of a gingival smile has become the most frequent dental esthetic rehabilitation. Characterized by excessive gingival exposure (above 3 mm), gingival smile affects approximately 10% of the population between 20 and 30 years [[3], [4], [5]].
The etiology of a gingival smile is multifactorial, for instance gingival hyperplasia, altered passive teeth eruption, skeletal deformities of excessive maxillary growth, lack of lip support resulting from a marked depression of the anterior process of the maxilla and a hyperactive and/or asymmetric upper lip. It is imperative that these etiologies are identified before rehabilitation treatment [4]. Accurate facial analysis is crucial to determine the most appropriate surgical periodontal treatment. Clinical crown lengthening is the commonest esthetic treatment in cases of abnormal passive teeth eruption and mild skeletal deformity. In some situations, a lack of lip support due to marked depression of the anterior process of the maxilla is the culprit. In these cases, esthetic clinical crown lengthening may be combined with lip repositioning using Polymethylmethacrylate (PMMA)-based orthopedic cement. This material has a good degree of compatibility with human tissues, acting as a filler material for subnasal depression and may be an innovative way to tackle gingival smile [4].
PMMA-based bone cement has been used in several health specialties, such as neurosurgery since World War II for cranioplasties, secondary to decompressive craniectomy and is still the most used reconstructive material by many professionals because it is one of the most biocompatible alloplastic materials available to date, inducing low foreign body reaction and providing adequate protection to adjacent neural tissues. The first indication for its use in dentistry was for full dentures and it has since demonstrated positive results, including high biocompatibility with the oral tissues [6].
In this case, a successful management of sever gummy smile using gingivectomy surgical procedures combined with PMMA-based bone cement had achieved satisfactory results. This manuscript has been reported in accordance with the SCARE criteria [7]. The aim of this report was to present a clinical case of lip repositioning using PMMA-based bone cement for esthetic smile rehabilitation
2. Case report
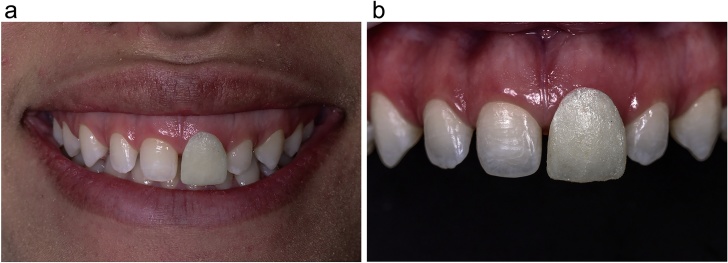
A 23-year-old female attended the Esthetic Dentistry Clinic of our institue, reporting dissatisfaction with her smile, due to the size of her teeth and the amount of gingiva exposed when smiling (Fig. 1). The patient wished to achieve a more harmonious smile.
Fig. 1.
Patient reporting dissatisfaction with her smile, due to the size of her teeth and the amount of gingiva exposed when smiling.
2.1. Clinical examination
The face, smile, gingival contour and teeth of the patient were analyzed both clinically and photographically (Fig. 2a–l). Radiographic examinations were then requested for periapicals bite-wings, cephalometric radiograph and computed tomography.
Fig. 2.
a, b, e, c – Initial Photographic protocol: Maximum smile. Front, left and right side views. d, e, e – Initial Photographic protocol: Lip sealing and incisal exposure Analysis. f – Initial Photographic protocol: Gingival exposure analysis at maximum smile. g, e, h – Initial Photographic protocol: Right and left half profile view. i – Initial photographic protocol: Maximum habitual intercuspation. j – Initial photographic protocol: Close-up of the anterior dentition, with contrast mirror, to evaluate shape, anatomical characteristics and arrangement of dental elements in the arch. k, e, l – Initial photographic protocol: Close-up of anterior dentition of left and right half-profile, with contrast mirror.
The patient was then diagnosed with excessive gingival exposure associated with depression of the subnasal region, in which the upper lip would lodge during smiling, lack of proportion of teeth as well as generalized diastemas.
A rehabilitation planning was designed, which was performed with periodontal surgical intervention to fill the subnasal depression with PMMA-based bone cement, clinical crown lengthening of teeth 15–25 in order to equalize the proportion between the teeth and esthetic rehabilitation of the smile using ceramic veneers.
2.2. Treatment considerations
To determine the correct proportion of the teeth, an acrylic resin device was fabricated on the upper central incisors for esthetic and functional evaluations, based on the patient’s interpupillary distance and described by Arcuri et al. [8] This device is used to evaluate the following: the correct proportion of the dimensions of the central incisor to be rehabilitated, involving its height and width, as well as its ideal spatial positioning in the arch; to predict the need for surgical intervention to lengthen the clinical crown and to provide an effective communication between the dental surgeon and the dental laboratory technician, guiding the diagnostic wax-up from the anatomical references obtained. (Fig. 3a and b).
Fig. 3.
a – Mini-Jig Aesthetic and Functional device to determining the ideal dimensions of the incisor to be rehabilitated on the upper central incisor. b – Mini-Jig Aesthetic and Functional device positioned and need for clinical crown lengthening evaluation.
Impressions for study models were taken using addition silicone (Virtual, Ivoclar Vivadent AG, Liechtenstein) (Fig. 4a and b). The esthetic and functional device positioned in the model aided the technician in building a diagnostic wax-up based on the anatomical references provided by the device (Fig. 5a and b). From the wax-up, a dense silicone dam (Zetalabor, Zhermack, Badia Polesine, Italy) was also made in the laboratory, which was later refined using a fluid silicone wash (Oranwash L, Zhermack, Badia Polesine, Italy) for accurate copying of the details of the teeth. This silicone dam was used to obtain a guide for the diagnostic restorative test (mock-up) (Fig. 6). Once the mock-up was tried in, the need for clinical crown lengthening was established aiming to reestablish the height and width proportions of the upper anterior teeth (Fig. 7).
Fig. 4.
a, e, b – Impressions for study models were taken using addition silicone.
Fig. 5.
a, e, b – Diagnostic wax-up based on the anatomical references provided by the device.
Fig. 6.
Silicone dam was used to obtain a guide for the diagnostic restorative test (mock-up).
Fig. 7.
Mock-up to patient approval.
2.3. Surgical procedures
An acetate surgical guide was made from a copy of the diagnostic wax-up model to serve as a parameter during osteotomy.
The periodontal surgery was performed based on the mock-up and using local anesthesia. Incisions were made using an internal bevel blade #15 from the mesial aspect of the first right upper molar to the mesial aspect of the first upper left molar, accompanying the cervical margin of the mock-up, which corresponded to the future margins of the prosthetic rehabilitation (Fig. 8). Subsequently, intra-sulcular incisions were made from 15 to 25 to remove the gingival margin collar (Fig. 9). A Molt 2–4 instrument was used to raise a full thickness flap and expose the entire frontal region of the maxilla, granting access to the subnasal depression and the anterior nasal spine (Fig. 10a). Osteotomy and osteoplasty were performed using large spherical burs at high speed and copious saline irrigation. Excess bone tissue was removed to a distance of 3 mm between the bony crest and the new gingival margin, to safeguard the biological width, as recommended by Gargiulo et al. [9] (Fig. 10b).
Fig. 8.
Clinical crown lengthening Incisions guided.
Fig. 9.
Incisions from 15 to 25 to remove the gingival margin collar.
Fig. 10.
a, e, b – Full thickness flap and Osteotomy and osteoplasty guided by the transparent guide.
2.4. Use of PMMA
After crown lengthening, the PMMA-based bone cement was prepared with gentamicin (Aminofix 1, Groupe Lépine, France) in a sterile surgical bowl following the manufacturer’s instructions. When the mixture stopped sticking to the surgical gloves, it was then positioned into the subnasal pit, under constant and copious saline irrigation. With the cement in place, the prosthesis was shaped in a maximum thickness of 7-mm, as recommended in the literature [10]. After complete polymerization and under abundant cooling, refinement and finishing of the PMMA prosthesis was performed using a Maxicut and Minicut handpiece burs. The prosthesis was verified for passive adaptation and fixed onto the bone with two titanium-based bone graft fixation screws, measuring 1.6 mm × 10 mm (Neodent, Group Straumann, Curitiba, Brazil). One screw was fixed between teeth 11 and 12 and the other between teeth 21 and 22 (Fig. 11).
Fig. 11.
PMMA prosthesis was fixed by screw between teeth 11 and 12 and the other between teeth 21 and 22.
At the end of the surgical procedure, the gingival flap was repositioned and a simple 6-0 nylon suture was placed (Fig. 12). Antibiotics, an anti-inflammatory and pain-killers were prescribed and the patient was instructed regarding postoperative care. At the 16-day follow-up of the surgical procedure, the patient was reassessed and the sutures removed, revealing a more harmonious smile than before, with reduction of the exposed gingiva, secondary to an increased clinical crown length and new support and repositioning of the upper lip (Fig. 13a and b).
Fig. 12.
Simple 6-0 nylon suture Sutura.
Fig. 13.
a, e, b – At the 16-day follow-up of the surgical procedure, the patient was reassessed and the sutures removed, revealing a more harmonious smile than before, with reduction of the exposed gingiva, secondary to an increased clinical crown length and new support and repositioning of the upper lip.
2.5. Prosthetic rehabilitation
The smile aesthetic rehabilitation was complemented using 10 lithium disilicate-based ceramic veneers (IPS Emax, Ivoclar Vivadent AG, Liechtenstein) (Fig. 14a–g). Twenty months after treatment completion, a new clinical evaluation was performed, on which occasion the esthetic results and periodontal health were reported to be maintained (Fig. 15).
Fig. 14.
a–g – The smile aesthetic rehabilitation was complemented using 10 lithium disilicate-based ceramic veneers.
Fig. 15.
Twenty months follow-up, on which occasion the esthetic results and periodontal health were reported to be maintained.
3. Discussion
In the treatment of a gingival smile, accurate diagnosis is fundamental to select the most appropriate strategy to tackle the problem on an individual basis. When the gingival smile is secondary to altered passive teeth eruption, gingivectomy and/or clinical crown lengthening may be indicated [10,11]. For lip hypermobility, both botulinum toxin and myotomy of lip-elevating muscles are used [10,11]. When the cause of the gingival smile is vertical maxillary excess, the treatment may be orthodontic intrusion, orthognathic surgery and even in such cases, if there is a lack of lip support, lip repositioning can be achieved using bone cement combined with clinical crown lengthening [2]. As mentioned above and in the light of the case reported herein, surgical guide-assisted clinical crown lengthening significantly improved smile harmony, reducing the gingival exposure presented by patient when smiling.
PMMA properties, such as inertness, low cost, rigidity, easy preparation, biocompatibility etc., make PMMA-based bone cements suitable for use in different health-related situations, body areas and procedures, such as in cranioplasty, in which it has been used since the second world war [[12], [13], [14]]. PMMA has been the most widely used material for correction of bony defects of the skull and face, mainly for cosmetic reasons [14].
In dentistry, PMMA has been used in several fields. Frazer et al. [6], described the use of PMMA for orthodontic appliances, dentures, definitive and temporary partial and full prostheses, as well as for maxillofacial prostheses and fixation of mandibular fractures. The authors also speculated that without the development of PMMA, it would not have been possible to provide the quality dental care that is available today.
According to Amer et al. [16], PMMA is used as a prosthetic material when the aim is dental corrections. PMMA bone cement can also be used as graft material for extraction sites, furcation lesions, correction of maxillary and mandibular contours and is also currently used to fill craniofacial defects such as subnasal depression [4].
In the clinical case presented herein, the PMMA-based bone cement was used to fill the subnasal maxillary skeletal depression, repositioning and allowing a new support to the upper lip, contributing to harmonization of the smile, initially conquered using clinical crown lengthening. No intraoperative and/or postoperative complications were detected.
The use of PMMA-based bone cement to fill subnasal depression in cases of vertical maxillary excess is a new strategy, first published by Torres et al. [4]. Its purpose is to support the upper lip, reducing its mobility and esthetically improving a gingival smile. The authors believe that the lip vermilion may be augmented due to new lip support. In the same study, the authors report that bone cement featuring PMMA microspheres does not induce any complications, compared to injectable PMMA used in permanent soft tissue filling, which is associated with complications such as tissue necrosis, granulomas, infections and lymphedemas, as described by Salles et al. [17].
Among the complications associated with PMMA, the long-term infection rate was 13.9% in the study by Kim et al. [18] Cheng et al. [19] detected approximately 6.25% of infections in their patients. Kumar et al. [20], however, found no complications in any of their 15 patients, a result similar to that of Rotaru et al. [21], where none of the patients presented complications.
The mixture of n-dimethyl-p-toluidine and benzoyl peroxide results in the cure of PMMA and during that process heat is released [22]. The temperatures released during curing of PMMA may vary, with reports showing exothermic reactions of 70 °C, 80 °C, 81.4 °C and 100 °C [23].
During intraoperative manipulation of the PMMA cement, tissues can be damaged when exposed to such high temperatures, in which exposure time is determinant [16]. Exothermic reaction can trigger inflammatory events and necrosis of tissues adjacent to PMMA, according to Khader and Towler [24].
To avoid complications from exothermic reactions, prefabricated plates are used, based on tomographic data from the bone defect or from previously obtained models [15]. In order to minimize the risk of tissue necrosis when using PMMA intra-operatively, irrigation is recommended repeatedly and constantly with cooled saline and to ensure the presence of a wet interface between the PMMA and the tissues [15,23].
The chemical reaction and the amount of heat released correlate positively with the thickness and volume of the PMMA bone cement [24]. Higher temperatures are associated with increased PMMA thickness in vitro [15].
It is important to be aware of the ultimate thickness of the PMMA implant, since the exothermic temperature is directly influenced by the PMMA thickness. A thickness of 7 mm is generally safe to work in procedures where the cement will be manipulated and shaped intra-operatively [25].
Abundant irrigation of PMMA removes all residual monomers, preventing not only damages caused by the exothermic reaction, but also the potential toxicity caused by the monomer [14]. Residual monomer may cause aseptic loosening of the prosthesis due to bone resorption around the PMMA cement [23]. Fixation of the PMMA prosthesis with plates and screws may be suitable to prevent aseptic loosening and to stabilize the prosthesis to the bone [12,13].
Torres et al. [4] and Jaberi et al. [25], recommend the intraoperative technique when the objective is to reconstruct small bony defects, 5–15 cm². The use of rotating instruments for finishing of the PMMA prosthesis intraoperatively is thought to increase the risk of contamination of the operative field. The intraoperative technique has been used for a long time, it does not add costs to the procedure, it is safe, presents good clinical results and low complication rates [4,12,26].
4. Conclusion
Based on the aforementioned arguments, it can be stated that:
-
1
PMMA-based bone cement proved effective when associated with clinical crown lengthening in esthetic smile rehabilitation, acting as a filling material for subnasal depression, providing new lip support and satisfying the patient’s expectations.
-
2
The technique is operator-sensitive, as the manufacturer's instructions should be strictly followed in order to avoid complications during the curing of the material, such as high exothermic reactions. The thickness of the PMMA implant is also paramount, since temperature is directly influenced by it.
-
3
PMMA is non-toxic, biocompatible with human tissues and is therefore used in various specialties for different procedures. This bone cement is regarded as an alloplastic material, used preferentially in reconstructions of craniofacial defects of variable sizes.
Conflicts of interest
The authors does not have any financial and personal relationships with other people or organisations that could inappropriately influence (bias) their work.
Funding
The authors states that the present study sponsors did not have any involvement in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Ethical approval
The authors state that the present study is exempt from ethical approval in their institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Toni Arcuri – First author, had contributed in the study concept, writing the paper and prosthetic reabilitation.
Maykson Feitosa Costa – Co-author, had contributed in data collection, analysis and interpretation and photograph documentation.
Iury Machado Ribeiro – Co-author, had contributed in the clinical surgery procedures.
Byron Daia Barreto Júnior – Co-author, had contributed in the data collection and in the clinical surgery procedures.
João Paulo Lyra e Silva – Co-author and corresponding author, had contributed in the study design and writing the paper.
Registration of research studies
researchregistry3952.
Unique Identifying Number: 3952.
Guarantor
Toni Arcuri, the first author, is the guarantor who accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Contributor Information
Toni Arcuri, Email: toniarcuri.odonto@yahoo.com.br.
Maykson Feitosa Pereira da Costa, Email: maykson.feitosa@gmail.co.
Iury Machado Ribeiro, Email: iury_machado@hotmail.com.
Byron Daia Barreto, Júnior, Email: byronhottestjr@hotmail.com.
João Paulo Lyra eSilva, Email: joaodf22@hotmail.com.
References
- 1.Garber D.A., Salama M.A. The aesthetic smile: diagnosis and treatment. Periodontology 2000. 1996;11:18–28. doi: 10.1111/j.1600-0757.1996.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 2.Mostafa D. A successful management of sever gummy smile using gingivectomy and botulinum toxin injection: a case report. Int. J. Surg. Case Rep. 2018;42:169–174. doi: 10.1016/j.ijscr.2017.11.055. Epub 2017 Dec 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schertel Cassiano L., Barriviera M., Suzuki S., Giacomelli Nascimento G., Lourenço Januario A., Hilgert L.A., Rodrigues Duarte W. Soft tissue cone beam computed tomography (ST-CBCT) for the planning of esthetic crown lengthening procedures. Int. J. Esthet. Dent. 2016;11(4):482–493. [PubMed] [Google Scholar]
- 4.Torres ÉM., Naldi L.F., Bernades K.O., Carvalho A.L. Four-year follow-up of a polymethyl methacrylate-based bone cement graft for optimizing esthetics in maxillary anterior implants: a case report. Gen. Dent. 2017;65(July–August (4)):48–53. [PubMed] [Google Scholar]
- 5.Tjan A.H.L., Miller G.D., The J.G.P. Some esthetic factors in a smile. J. Prosthet. Dent. 1984;51:24–28. doi: 10.1016/s0022-3913(84)80097-9. [DOI] [PubMed] [Google Scholar]
- 6.Frazer R.Q., Byron R.T., Osborne P.B., West K.P. PMMA: an essential material in medicine and dentistry. J. Long-Term Eff. Med. Implants. 2005;15(6):629–639. doi: 10.1615/jlongtermeffmedimplants.v15.i6.60. [DOI] [PubMed] [Google Scholar]
- 7.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The Scare statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;27:187–189. doi: 10.1016/j.ijsu.2016.01.094. [DOI] [PubMed] [Google Scholar]
- 8.Arcuri T., Byron D.B., Junior, Ribeiro I.M., Celestrino M., Silva J.P.L. Mini-Jig estético-funcional: a chave para o planejamento da reabilitação oral. Int. J. Esthet. Dent. 2016;1:584–601. [Google Scholar]
- 9.Gargiulo A.W., Wentz F.M., Orban B. Dimensions and relations of the dentogingival junction in humans. J. Periodontol. 1961;32(3):261–267. [Google Scholar]
- 10.Kriegel R.J., Schaller C., Clusmann H. Cranioplasty for large skull defects with PMMA (polymethylmethacrylate) or tutoplast ® processed autogenic bone grafts. Zentralbl. Neurochir. 2007;68(4):182–189. doi: 10.1055/s-2007-985857. [DOI] [PubMed] [Google Scholar]
- 11.Mantovani M.B., Souza E.C., Marson F.C., Corrêa G.O., Progiante P.S., Silva C.O. Use of modified lip repositioning technique associated with esthetic crown lengthening for treatment of excessive gingival display: a case report of multiple etiologies. J. Indian Soc. Periodontol. 2016;20(1):82–87. doi: 10.4103/0972-124X.164746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tanner K.E. Optimising the properties of injectable materials for vertebroplasty and kyphoplasty. In: Ambrozio L., Tanner E., editors. Biomaterials for Spinal Surgery. Woodhead Publishing Limited; Sawston: 2012. pp. 385–403. [Google Scholar]
- 13.Kumar N.G., Rangarajan H., Shourie P. Cranioplasty of hemispherical defects using high impact methylmethacrylic plate. J. Craniofac. Surg. 2015;26:1882–1886. doi: 10.1097/SCS.0000000000002006. [DOI] [PubMed] [Google Scholar]
- 14.Kim S.H., Kang D.S., Cheong J.H., Kim J.H., Song K.Y., Kong M.H. Comparison of complications following cranioplasty using a sterilized autologous bone flap or polymethyl methacrylate. Korean J. Neurotrauma. 2017;13(1):15–23. doi: 10.13004/kjnt.2017.13.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li C., Schmid S., Mason J. Effects of pre-cooling and pre-heating procedures on cement polymerization and thermal osteonecrosis in cemented hip replacements. Med. Eng. Phys. 2003;25(7):559–564. doi: 10.1016/s1350-4533(03)00054-7. [DOI] [PubMed] [Google Scholar]
- 16.Amer Z.J.A., Ahmed J.K., Abbas S.F. Chitosan/PMMA bioblend for drug release applications. J. Eng. Technol. Res. 2014;4(5):318–324. [Google Scholar]
- 17.Salles A.G., Lotierzo P.H., Gemperli R., Besteiro J.M., Ishida L.C., Gimenez R.P. Complications after polymethylmethacrylate injections: report of 32 cases. Plast. Reconstr. Surg. 2008;121(5):1811–1820. doi: 10.1097/PRS.0b013e31816b1385. [DOI] [PubMed] [Google Scholar]
- 18.Kim S.H., Kang D.S., Cheong J.H., Kim J.H., Song K.Y., Kong M.H. Comparison of complications following cranioplasty using a sterilized autologous bone flap or polymethyl methacrylate. Korean J. Neurotrauma. 2017;13(1):15–23. doi: 10.13004/kjnt.2017.13.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheng Y.K., Weng H.H., Yang J.T., Lee M.H., Wang T.C., Chang C.N. Factors affecting graft infection after cranioplasty. J. Clin. Neurosci. 2008;15(10):1115–1119. doi: 10.1016/j.jocn.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 20.Kumar N.G., Rangarajan H., Shourie P. Cranioplasty of hemispherical defects using high impact methylmethacrylic plate. J. Craniofac. Surg. 2015;26:1882–1886. doi: 10.1097/SCS.0000000000002006. [DOI] [PubMed] [Google Scholar]
- 21.Rotaru H., Stan H., Florian I.S., Schumacher R., Parque Y.T., Kim S.G. Cranioplasty with custom-made implants: analyzing the cases of 10 patients. J. Oral Maxillofac. Surg. 2012;70(2):169–176. doi: 10.1016/j.joms.2011.09.036. [DOI] [PubMed] [Google Scholar]
- 22.Shi M., Kretlow J.D., Spicer P.P., Tabata Y., Demian N., Wong M.E. Antibiotic-releasing porous polymethylmethacrylate/gelatin/antibiotic constructs for craniofacial tissue engineering. J. Control. Release. 2011;152:196–205. doi: 10.1016/j.jconrel.2011.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdo Filho R.C.C., Oliveira T.M., Neto N.L., Gurgel C., Abdo R.C.C. Reconstruction of bony facial contour deficiencies with polymethylmethacrylate implants: case report. J. Appl. Oral Sci. 2011;19(4):426–430. doi: 10.1590/S1678-77572011000400021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khader B.A., Towler M.R. Materials and techniques used in cranioplasty fixation: a review. Mater. Sci. Eng. 2016;66:315–322. doi: 10.1016/j.msec.2016.04.101. [DOI] [PubMed] [Google Scholar]
- 25.Jaberi J., Gambrell K., Tiwana P., Madden C., Finn R. Long-term clinical outcome analysis of poly-methyl-methacrylate cranioplasty for large skull defects. J. Oral Maxillofac. Surg. 2013;71:81–88. doi: 10.1016/j.joms.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 26.Unterhofer C., Wipplinger C., Verius M., Recheis W., Thomé C., Ortler M. Reconstruction of large cranial defects with poly-methyl-methacrylate (PMMA) using a rapid prototyping model and a new technique for intraoperative implant modeling. Neurol. Neurochir. Pol. 2017;291:1–7. doi: 10.1016/j.pjnns.2017.02.007. [DOI] [PubMed] [Google Scholar]