Abstract
Context:
The orthodontic treatment in adult for the treatment of malocclusion is becoming more common. However, the disadvantages of conventional orthodontics are the time consumed for the treatment (18–24 months), root resorption, and formation of fenestrations and dehiscence. Periodontally accelerated osteogenic orthodontics (PAOO) is a surgical technique resulting in increased alveolar bone width, shorter treatment time, increase posttreatment stability, and decrease amount of apical root resorption.
Aim:
The aim of the study is to compare the treatment time, root resorption, bone density, and presence/absence of fenestrations and dehiscence after PAOO with surgical bur and PAOO with piezocision.
Materials and Methods:
Forty participants with bimaxillary protrusion undergoing orthodontic treatment were randomly selected and divided into two groups. Group I: 20 participants selected for PAOO with surgical bur and Group II: 20 participants selected for PAOO with piezocision. Patients were recalled at baseline 3, 6, 9, and 12 months and evaluated for treatment time and bone density, root resorption, and detection of fenestration and dehiscence using cone-beam computerized tomography (CBCT).
Results:
Participants in Group I had less treatment time compared to Group II. Rate of retraction was 7.07 mm/20.81 weeks and 5.99 mm/28.48 weeks in Group I and Group II, respectively. CBCT showed a statistically significant increase in bone density in both groups, 12 months after the surgery. Root resorption was negligible in Group I (0.34 mm) and in Group II (0.51 mm). CBCT revealed increase in thickness of alveolar bone and coverage of fenestrations and dehiscence.
Conclusion:
PAOO provides an efficient and stable orthodontic tooth movement.
Key words: Corticotomy, orthodontics, osteogenic, piezosurgery, protrusion
INTRODUCTION
Conventional orthodontic treatment for the correction of malocclusion is accepted worldwide, but the major drawback of it is the time taken for the treatment which is around 18–24 months.
Conventional orthodontic movements cause periodontal ligament compression and produce histological and biomolecular modifications. Orthodontic tooth movement is achieved by a balance between bone resorption on pressure side and deposition on the tension side of the tooth during the application of optimum orthodontic force. During orthodontic treatment, increased time duration has been linked to an increased risk of root and bone resorption which may arise due to inappropriate force magnitude or tooth movement into dense or altered bone.[1]
The tooth movement is enhanced by procedures that elevate the remodeling of alveolar bone, periodontal, and gingival fibrous tissues by disrupting the continuity of cortical bone, thereby orthodontic is completed in much less time than normally expected.[2] This procedure was termed as accelerated osteogenic orthodontics (AOO) and recently as periodontally AOO (PAOO) or Wilckodontics introduced by Dr. William Wilcko and Dr. Thomas Wilcko, in which teeth can be moved 2–3 times faster in (1/3) to (1/4) the time required for traditional orthodontic therapy. It helps orthodontic tooth movement by accelerated bone metabolism due to controlled surgical damage to the cortical bone. It utilizes the dynamics of bone physiology and emphasis on tooth movement, in which the supporting bone responds to orthodontic forces rather than just concentrating on the manner in which the forces are applied to the teeth. PAOO combines selective alveolar corticotomy, particulate bone grafting and the application of orthodontics forces. This procedure is theoretically based on a bone healing pattern known as regional acceleratory phenomenon (RAP).[3]
The aim of the study is to compare the treatment time, root resorption, bone density, and presence or absence of fenestrations and dehiscence after PAOO with surgical bur and PAOO with piezocision.
Subject
This is a randomized case-controlled clinical trial performed on 40 participants.
Group I: Twenty participants selected for PAOO with surgical bur
Group II: Twenty participants selected for PAOO with piezocision.
Inclusion criteria
Both male and female participants with age group of 20–40 years
Systemically healthy individuals
Participants with at least 20 permanent teeth
Participants with Angel's Class I malocclusions with bimaxillary protrusion.
Exclusion criteria
Participants with active periodontal disease
Participants with severe Class III malocclusion
Participants indicated for orthognathic surgery
Participants who have undergone any periodontal surgery within 6 months
Smokers
Participants using corticosteroids or bisphosphonates
Participants with bleeding disorders and any other systemic diseases
Pregnant and lactating women.
MATERIALS AND METHODS
Written consent was obtained from all the participants. Ethical clearance was obtained from the Ethical Committee of the Institute.
Pre- and post-operative study models, photographs, and radiographs such as orthopantamograph were recorded for each participant in baseline, 3, 6, and 12 months' intervals.
Participants were given a presurgical rinse with 0.2% chlorhexidine for 1 min and were anesthetized with the help of 2% lignocaine with 200,000 adrenaline.
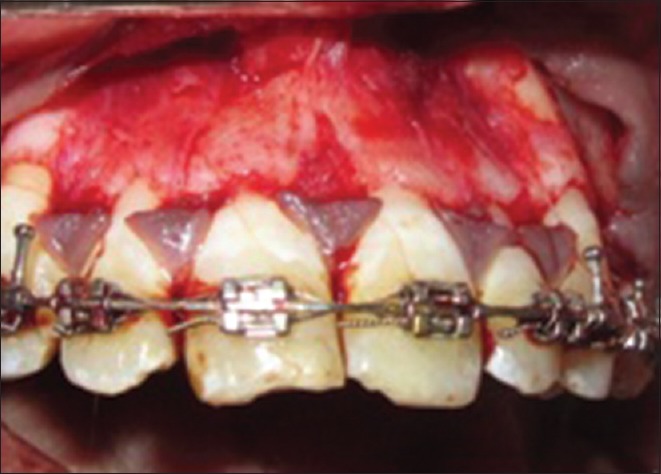
In Group I – Sulcular releasing incisions and incisions to preserve the papilla were done labially [Figure 1]. A full-thickness flap from premolar extraction site of one side to other, both in the maxillary and mandibular region, was done to expose the underlying alveolar bone to provide access [Figure 2]. Decortication in alveolar bone was using No. 1 or 2 round tungsten-carbide bur in a high-speed handpiece with saline irrigation [Figure 3]. Guiding pilot perforations were given in the interradicular area; these were joined to create vertical corticotomy grooves which are about 1.5–2 mm in depth. This groove was extended from a point 2–3 mm away from the crest of the alveolar bone to a point 2 mm beyond the apices of the roots. If the alveolar bone was of sufficient thickness (more than 1–2 mm), solitary perforations were placed in the alveolar bone over the radicular surface [Figure 4].
Figure 1.

Intracrevicular incisons and incisions to preserve the interdental papilla given
Figure 2.

Full-thickness mucoperiosteal flap elevated (Group I)
Figure 3.
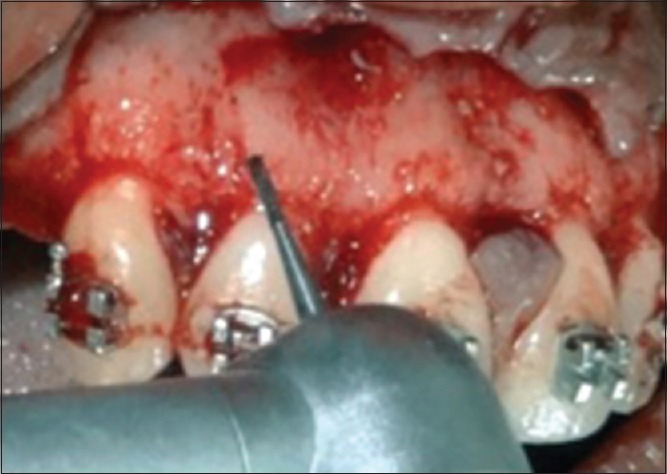
Corticotomy done with surgical bur (Group I)
Figure 4.

Vertical corticotomies and perforations given (Group I)
In Group II – Sulcular releasing incisions and incisions to preserve the papilla were done labially [Figure 5]. A full-thickness flap from premolar extraction site of one side to other, both in maxillary and mandibular region, was done to expose the underlying alveolar bone to provide access [Figure 6]. Decortication in alveolar bone was done using piezotome handpiece with piezo surgical knife [Figure 7]. Guiding pilot perforations were given in the interradicular area these were joined to create vertical corticotomy grooves which are about 1.5–2 mm in depth [Figure 8].
Figure 5.

Sulcular incisions and incisions to preserve interdental papilla given (Group II)
Figure 6.
Full-thickness mucoperiosteal flap elevated (Group II)
Figure 7.
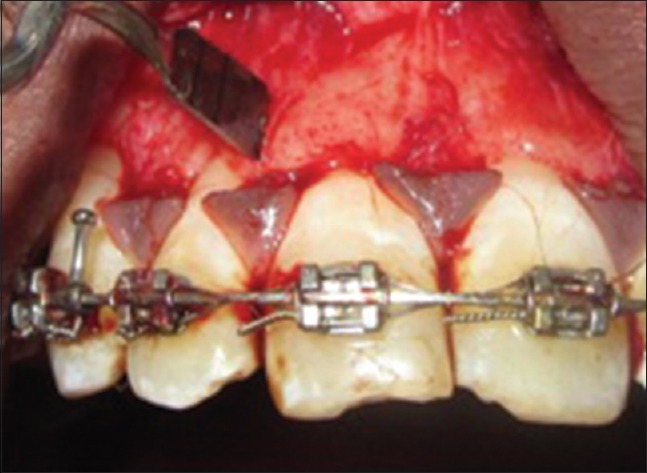
Corticotomy done with piezocision (Group II)
Figure 8.

Vertical corticotomies and perforations given (Group II)
In both the groups, the volume of the graft material in the corticotomy areas was dictated by the pretreatment thickness of the alveolar bone and the need for labial support by the alveolar bone. A typical volume used was 0.25–0.5 ml of graft material per tooth. Primary closure of the flaps with interrupted sutures was done using 4.0 silk sutures and periodontal dressing was placed. Sutures were removed after 2-week postsurgically. Participants recalled at 1, 3, 6, and 12 months.
In both the groups, bonding of MBT 0.022” slot bracket was done. Nickel–titanium wire was used in the initial phase of leveling and aligning. Following which stainless steel wire (0.019” × 0.025”) was placed in participant before retraction was initiated. Extraction space was measured with digital caliper before initiating retraction in both the groups.
In both the groups, after corticotomy procedure, the participants were recalled at an interval of 2 weeks for replacement of active tiebacks.
Statistical analysis used: Student's t-test and unpaired t-test.
RESULTS
A total of 43 participants were recruited for the study, in which three dropped out from continuing the treatment for personal issues, in which 1/3 underwent surgery of maxilla. A total of 40 participants completed the entire duration of the study and divided into two groups: 20 participants in Group I and 20 participants in Group II participated in the study.
The statistical power of the study when comparing 40 participants (20 in each group) with the data obtained from measuring treatment time and retraction rate was found to be 90%.
Table 1 shows the total measurement for the closure of extraction space during retraction of teeth in maxilla and mandible in Group I and Group II. Mean retraction of 7.07 ± 0.5 mm in Group I and 5.99 ± 0.35 mm in Group II after 12 months, with higher mean retraction in Group I than Group II and was found to be statistically significant (P < 0.001).
Table 1.
Comparison of retraction (mm)
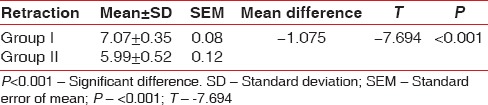
Table 2 shows the mean retraction time in weeks for Group I: 20.81 ± 1.08 weeks (5 months and 2 weeks) while for Group II: 28.48 ± 1.70 weeks (7 months and 1 week) (P < 0.001). These findings were statistically highly significant (P < 0.001).
Table 2.
Comparison of retraction time (weeks)
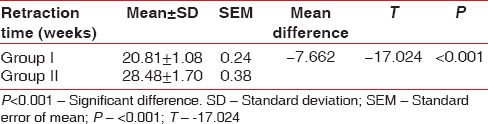
Table 3 shows root resorption measured as total lengths of each tooth from canine to canine by cone-beam computerized tomography (CBCT) at baseline and 12 months. There was a decrease in mean tooth length from pre- to post-operative time interval at maxilla and mandible region in Group I and Group II which was found to be statistically significant (P < 0.001).
Table 3.
Comparison of tooth length in each group between preoperative and postoperative
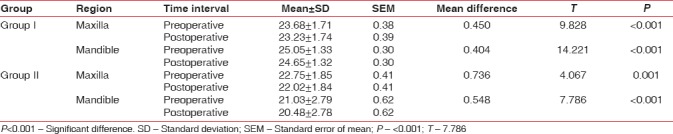
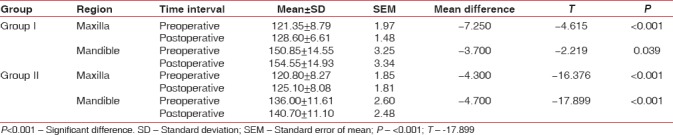
Table 4 shows the bone densities in both groups that were assessed at baseline and 12 months with significant increase in both the groups: in Group I – maxilla (121.35 ± 8.79–128.60 ± 6.61) (P > 0.005) and mandible (150.85 ± 14.55–154.55 ± 14.93) (P < 0.001) and in Group II – maxilla (120.80 ± 8.27–125.10 ± 8.08) (P > 0.05) and mandible (136.35 ± 11.61–140.70 ± 11.10) (P < 0.01). All the values in both groups in the mandible region were highly statistically significant (P < 0.01).
Table 4.
Comparison of bone density in each group between preoperative and postoperative: Paired t-test
DISCUSSION
PAOO helps to overcome the drawbacks of conventional orthodontic treatment, including lengthy duration, potential for periodontal complications, lack of growth, and the limited envelope of tooth movement.
In the late 1990s, the Wilcko brothers developed the AOO procedure and added the alveolar augmentation to the corticotomies performed both buccally and lingually and concluded 75% reduction in orthodontic treatment.[4] A modified corticotomy technique was introduced in which labial and lingual supraapical horizontal and lingual vertical cuts were not performed.[5] In 2007, Vercellotti and Podesta introduced the use of piezosurgery instead of burs, in conjunction with the conventional flap elevations to create an environment conducive to rapid tooth movement.[6] In 2009, Dibart et al. described a new minimally invasive procedure called piezocision.[7]
PAOO causes the induction of bone metabolism through decortication lines and points around the teeth to be moved to enhance bone and periodontal turnover, resulting in a transient stage of osteopenia during treatment thus accelerating tooth movement.[2,8,9,10,11,12]
The total treatment time for Group I was 20.81 weeks (5 months and 2 weeks) and for Group II was 28.48 weeks (7 months and 1 week). This is in accordance with the clinical observations by Wilcko et al. and Hajji,[4,13,14,15] who reported similar significant reductions in treatment time with stable orthodontic tooth movement and also certain case reports of piezocision in humans with moderate to light crowding showed increased rate of acceleration of orthodontic tooth movement to be approximately 5–7 months.[16,17,18] The rapid tooth movement in piezocision-assisted corticotomy is due to the micrometric and selective cuts and producing a safe and precise osteotomies without osteonecrotic damage in contrast to rotary burs.[19,20] This is not in accordance with the study done by Abbas and Moutamed which concluded that surgical control for piezosurgery was easier than conventional surgical burs for selective alveolar corticotomies.[21] Piezosurgery provided more favorable osseous repair and remodeling than with conventional surgical burs with surgical ostectomy and osteoplasty procedures.[6] Histological studies have shown minimal cellular damage to the respected bone margins, bony matrix, and underlying marrow spaces by piezosurgery.[22,23,24]
A minimal amount of root resorption was 0.34 and 0.51 mm in Group I and Group II, respectively, which is in accordance to findings by Kurol and Owman-Moll and Wilcko et al.,[13,25] whereas Ong and Wang showed mean shortening of root in central incisors to be 0.23 mm in PAOO group and 0.52 mm in conventional orthodontic group.[26] The theoretical linear rate of resorption for osteoclasts during cortical bone remodeling is 0.6 mm/month through cortical bone.[27,28]
The presence of fenestrations and dehiscence during the elevation of full thickness was seen in all participants while 12 months after surgery as assessed by CBCT, no fenestrations and dehiscence were noted, and this finding is supported by study done by Wilcko et al.[4]
An increase in bone density was observed in both the groups, especially Group I, which is attributed to the presence of the combination of bone grafting material and the transient osteopenia leading to increase in bone turnover, rapid removal of the hyalinized areas, and decrease of bone density in the region of tooth movement. This condition favors tooth movement with reduced root resorption.[29]
Retraction in the present study was started 2-week postsurgery as recommended by Wilcko et al. On contrary, Chung et al. and Sanjideh et al.[30,31] started retraction immediately after corticotomy. Two week delay between surgery and initiation of retraction was followed so that the postoperative pain and swelling could subside in subject.
The adverse effect of corticotomy on the periodontium ranges from no problem to gingival recession and decrease in width of attached gingiva. In the present study, all the participants were given NSAID'S and antibiotics after the surgery, and the incisions were modified which preserve the interdental papilla, so no recession reported in any of the cases but 3 out of 20 participants in Group II reported with pain, swelling, and hematoma of chin for 2–3 days which gradually subsided. The reason could increase working pressure which impedes the vibration of devices that transform the vibrational energy into heat which damages the tissue.[22]
Since most of the decortication procedures are based on case reports, more laboratory and clinical studies are necessary to better explain the biological mechanisms involved at both the tissue and molecular level and to investigate the long-term effects of this procedure since 12 months is not sufficient to analyze the long-term effects of PAOO.
CONCLUSION
PAOO with surgical bur gives significant reduction in treatment time and increase in retraction rate when compared with PAOO with piezosurgery and conventional orthodontic treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ristic M, Vlahovic Svabic M, Sasic M, Zelic O. Clinical and microbiological effects of fixed orthodontic appliances on periodontal tissues in adolescents. Orthod Craniofac Res. 2007;10:187–95. doi: 10.1111/j.1601-6343.2007.00396.x. [DOI] [PubMed] [Google Scholar]
- 2.Yamasaki K, Shibata Y, Fukuhara T. The effect of prostaglandins on experimental tooth movement in monkeys (Macaca fuscata) J Dent Res. 1982;61:1444–6. doi: 10.1177/00220345820610121401. [DOI] [PubMed] [Google Scholar]
- 3.Ferguson DJ, Al-Harbi MS, Wilcko WM, Wilcko MT, Erie P. Lower dental arch decrowding comparing non-extraction accelerated osteogenesis and distraction techniques. J Dent Res. 2001;80:181–3. [Google Scholar]
- 4.Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21:9–19. [PubMed] [Google Scholar]
- 5.Germeç D, Giray B, Kocadereli I, Enacar A. Lower incisor retraction with a modified corticotomy. Angle Orthod. 2006;76:882–90. doi: 10.1043/0003-3219(2006)076[0882:LIRWAM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Vercellotti T, Podesta A. Orthodontic microsurgery: A new surgically guided technique for dental movement. Int J Periodontics Restorative Dent. 2007;27:325–31. [PubMed] [Google Scholar]
- 7.Dibart S, Sebaoun JD, Surmenian J. Piezocision: A minimally invasive, periodontally accelerated orthodontic tooth movement procedure. Compend Contin Educ Dent. 2009;30:342. [PubMed] [Google Scholar]
- 8.Nishida M, Iizuka T, Itoi S, Hyo Y, Ono T. Clinical study of corticotomy by Kole's method. J Jpn Oral Surg Soc. 1986;3:81–4. [Google Scholar]
- 9.Bell WH, Levy BM. Revascularization and bone healing after maxillary corticotomies. J Oral Surg. 1972;30:640–8. [PubMed] [Google Scholar]
- 10.Gantes B, Rathbun E, Anholm M. Effects on the periodontium following corticotomy-facilitated orthodontics. Case reports. J Periodontol. 1990;61:234–8. doi: 10.1902/jop.1990.61.4.234. [DOI] [PubMed] [Google Scholar]
- 11.Suya H. Corticotomy in orthodontics. In: Hosl E, Baldauf A, editors. Mechanical and Biological Basis in Orthodontic Therapy. Huthig Buch Verlag; Heidelberg, Germany: 1991. pp. 207–26. [Google Scholar]
- 12.McFadden WM, Engstrom C, Engstrom H, Anholm JM. A study of the relationship between incisor intrusion and root shortening. Am J Orthod Dentofacial Orthop. 1989;96:390–6. doi: 10.1016/0889-5406(89)90323-5. [DOI] [PubMed] [Google Scholar]
- 13.Wilcko WM, Ferguson DJ, Bouquot JE, Wilcko MT. Rapid orthodontic decrowding with alveolar augmentation: Case report. World J Orthod. 2003;4:197–205. [Google Scholar]
- 14.Hajji SS. The influence of accelerated osteogenic response on mandibular decrowding. J Dent Res. 2001;80:180. [Google Scholar]
- 15.Wilcko MT, Wilcko WM, Pulver JJ, Bissada NF, Bouquot JE. Accelerated osteogenic orthodontics technique: A 1-stage surgically facilitated rapid orthodontic technique with alveolar augmentation. J Oral Maxillofac Surg. 2009;67:2149–59. doi: 10.1016/j.joms.2009.04.095. [DOI] [PubMed] [Google Scholar]
- 16.Dibart S, Surmenian J, Sebaoun JD, Montesani L. Rapid treatment of class II malocclusion with piezocision: Two case reports. Int J Periodontics Restorative Dent. 2010;30:487–93. [PubMed] [Google Scholar]
- 17.Keser EI, Dibart S. Piezocision-assisted invisalign treatment. Compend Contin Educ Dent. 2011;32:46. [PubMed] [Google Scholar]
- 18.Brugnami F, Caiazzo A, Dibart S. Lingual orthodontics: Accelerated realignment of the “social six” with piezocision. Compend Contin Educ Dent. 2013;34:608–10. [PubMed] [Google Scholar]
- 19.Kotrikova B, Wirtz R, Krempien R, Blank J, Eggers G, Samiotis A, et al. Piezosurgery – A new safe technique in cranial osteoplasty? Int J Oral Maxillofac Surg. 2006;35:461–5. doi: 10.1016/j.ijom.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Robiony M, Polini F, Costa F, Vercellotti T, Politi M. Piezoelectric bone cutting in multipiece maxillary osteotomies. J Oral Maxillofac Surg. 2004;62:759–61. doi: 10.1016/j.joms.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 21.Abbas I, Moutamed G. Acceleration of orthodontic tooth movement by alveolar corticotomy using piezosurgery. J Am Sci. 2012;8:13–9. [Google Scholar]
- 22.Chung KR, Oh MY, Ko SJ. Corticotomy-assisted orthodontics. J Clin Orthod. 2001;35:331–9. [PubMed] [Google Scholar]
- 23.Chiriac G, Herten M, Schwarz F, Rothamel D, Becker J. Autogenous bone chips: Influence of a new piezoelectric device (Piezosurgery) on chip morphology, cell viability and differentiation. J Clin Periodontol. 2005;32:994–9. doi: 10.1111/j.1600-051X.2005.00809.x. [DOI] [PubMed] [Google Scholar]
- 24.Happe A. Use of a piezoelectric surgical device to harvest bone grafts from the mandibular ramus: Report of 40 cases. Int J Periodontics Restorative Dent. 2007;27:241–9. [PubMed] [Google Scholar]
- 25.Kurol J, Owman-Moll P. Hyalinization and root resorption during early orthodontic tooth movement in adolescents. Angle Orthod. 1998;68:161–5. doi: 10.1043/0003-3219(1998)068<0161:HARRDE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Ong MM, Wang HL. Periodontic and orthodontic treatment in adults. Am J Orthod Dentofacial Orthop. 2002;122:420–8. doi: 10.1067/mod.2002.126597. [DOI] [PubMed] [Google Scholar]
- 27.Roberts WE, Goodwin WC, Jr, Heiner SR. Cellular response to orthodontic force. Dent Clin North Am. 1981;25:3–17. [PubMed] [Google Scholar]
- 28.Roberts WE, Arbuckle GR, Analoui M. Rate of mesial translation of mandibular molars using implant-anchored mechanics. Angle Orthod. 1996;66:331–8. doi: 10.1043/0003-3219(1996)066<0331:ROMTOM>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Sebaoun JD, Ferguson DJ, Kantarci A, Carvalho RS, Van Dyke TE. Catabolic modeling of trabecular bone following selective alveolar decortication. Dentofac Orthop. 2009;136:570–2. doi: 10.1902/jop.2008.080024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chung KR, Kim SH, Lee BS. Speedy surgical-orthodontic treatment with temporary anchorage devices as an alternative to orthognathic surgery. Am J Orthod Dentofacial Orthop. 2009;135:787–98. doi: 10.1016/j.ajodo.2007.03.036. [DOI] [PubMed] [Google Scholar]
- 31.Sanjideh PA, Rossouw PE, Campbell PM, Opperman LA, Buschang PH. Tooth movements in foxhounds after one or two alveolar corticotomies. Eur J Orthod. 2010;32:106–13. doi: 10.1093/ejo/cjp070. [DOI] [PubMed] [Google Scholar]


