Figure 1.
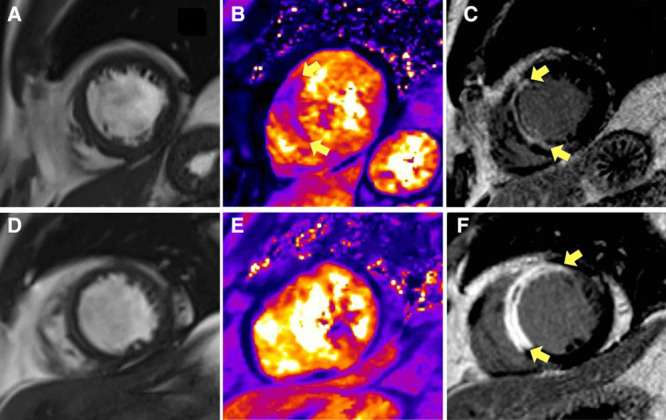
Two patients, one with a history of hypertension (A) and the other without (B) presented similarly with acute anterior ST-segment–elevation myocardial infarction and were treated by primary percutaneous coronary intervention (PCI) with stents. The antithrombotic therapies, including aspirin, clopidogrel, and unfractionated heparin, were similar. Each patient had normal antegrade flow in the culprit coronary artery (Thrombolysis In Myocardial Infarction grade 3) at the end of PCI. Multiparametric cardiovascular magnetic resonance (CMR) imaging was performed 2 d and 6 mo later. Top, A, Imaging obtained from a 52-year-old man with a history of current hypertension. The symptom-to-balloon time was 1.4 h. The coronary angiogram revealed a proximal occlusion of the left anterior descending artery. Blood pressure before coronary angioplasty was 200/125 mm Hg and measured 181/117 mm Hg postcoronary angioplasty. Two days later, CMR disclosed myocardial hemorrhage specifically revealed by T2* mapping (yellow arrows) and transmural infarction of the anteroseptal wall of the left ventricle (LV; yellow arrows) associated with microvascular obstruction revealed by contrast CMR. Invasive assessment of microvascular function using a diagnostic guidewire placed in the culprit coronary artery at the end of primary PCI indicated severe microvascular injury. The index of microvascular resistance measured 92 which is substantially increased (reference range <25). The initial infarct size was 38.9%, and the LV ejection fraction (LVEF) and LV end-diastolic volume indexed to body surface area (LVEDVi) were 48.5% and 90.2 mL/m2, respectively. Six months later, infarct size was 26.7% of LV mass, and the LVEDVi was 127 mL/m2. This is in-keeping with >20% in LVEDVi, that is, adverse remodeling. This patient went to have an unplanned admission for heart failure treatment on day 493 of follow-up. Bottom, B, Imaging obtained from a 58-year-old man with no prior history of hypertension. The symptom-to-balloon time was 2.2 h. The angiogram also revealed a proximal occlusion of the left anterior descending artery. Blood pressure before coronary angioplasty was 109/71 mm Hg and measured 99/60 mm Hg postcoronary angioplasty. Microvascular resistance in the culprit coronary artery was normal. Two days later, there was a small amount of microvascular obstruction as revealed by contrast-enhanced CMR (yellow arrows), and no evidence of myocardial hemorrhage (T2 star parametric map). The initial infarct size was 32.4%, and the LVEF and LVEDVi were 36.9% and 126.4 mL/m2, respectively. Six months later, infarct size was 15.2% of left ventricular mass, and the LVEDVi was 98.2 mL/m2. This patient had an uncomplicated clinical course.
