Abstract
Despite the various advantages of femtosecond laser-assisted cataract surgery (FLACS), pupillary constriction during laser photodisruption is considered one of the most unfavorable events. This study aimed to investigate the efficacy of intracameral 0.015% epinephrine injection for miosis after laser pretreatment during FLACS.
A total of 82 patients who underwent FLACS for age-related cataracts were investigated in this retrospective study. The epinephrine group included patients who received intracameral epinephrine injection for miosis after femtosecond laser pretreatment, while the no-epinephrine group included the patients who underwent FLACS without intracameral epinephrine due to minimal miosis. Quantitative pupil area measurements were performed through the analysis of captured images extracted from surgical videos of both femtosecond laser pretreatment and phacoemulsification.
Laser photodisruption induced miosis in both groups, although the degree of miosis was greater in the epinephrine group (4.65 ± 0.87 mm) than in the no-epinephrine group (6.30 ± 0.65 mm; P < .001). The intracameral epinephrine injection significantly increased the pupil diameter from 4.65 ± 0.87 to 5.49 ± 0.76 mm (21.61 ± 22.68%; P < .001) and the pupil area from 70.28 ± 24.46 to 96.49 ± 25.24 mm2 (52.89 ± 63.54%; P < .001). After additional viscomydriasis, there was no difference between groups in pupil diameter (epinephrine vs no-epinephrine group; 6.10 ± 0.77 vs 6.39 ± 0.65 mm; P = .073).
A single intracameral injection of 0.015% epinephrine provided immediate and appropriate redilation of pupil in patients with significant miosis after femtosecond laser photodisruption. Intracameral epinephrine is a simple and practical option for pupil redilation in case of miosis during FLACS.
Keywords: cataract surgery, femtosecond laser-assisted, intracameral epinephrine, miosis
1. Introduction
Since the introduction of femtosecond laser technology for cataract surgery procedures in 2009,[1] the efficacy and safety of femtosecond laser-assisted cataract surgery (FLACS) in comparison with those of manual cataract surgery have been demonstrated. Precise and predictable capsulotomy,[2–4] accurate and stable corneal incisions,[5,6] and low erroneous astigmatic keratotomies during laser pretreatments[7,8] with FLACS have been reported. In addition, the effective phacoemulsification time can be significantly decreased by laser fragmentation during FLACS.[9,10]
Despite the various advantages of FLACS, pupillary constriction induced by prostaglandin release during laser photodisruption is considered one of the most unfavorable events.[11,12] Early studies on the complications of FLACS have reported that the incidence of intraoperative miosis due to femtosecond laser pretreatment is approximately 9.5% to 32%,[13–15] and we reported that the pupil area can be decreased by nearly 30% after femtosecond laser photodisruption.[16] Schultz et al[17–19] suggested that laser capsulotomy is associated with prostaglandin release and hypothesized that lower pulse energy and reduced incision depth during capsulotomy could prevent miosis because shockwaves delivered to the ciliary body might induce prostaglandin release. Recent trials have reported the efficacy of pretreatment with nonsteroidal anti-inflammatory drug (NSAID) eye drops for the prevention of miosis after femtosecond laser procedures. In these studies, NSAID pretreatment effectively minimized the elevation of prostaglandin E2 concentrations in the aqueous humor. However, we observed that significant miosis still occurred at a constant rate after this pretreatment, and that the pupil area decreased after the laser procedure even if the degree of miosis was lowered.[20–23]
There are 2 solutions for miosis occurring after the laser procedure despite pretreatment with NSAID eye drops. One is mechanical redilation with iris retractors or expansion rings, which is an easily applicable and effective solution. However, pupillary constriction interferes with observation of the laser capsulotomy margin, and capsulotomy using a mechanical device results in more easy tearing compared with continuous curvilinear manual capsulotomy. In addition, the use of a mechanical device can increase surgical costs. Therefore, redilation using mydriatics or intracameral injection of adrenergic receptor agonists such as epinephrine or phenylephrine would be a more efficient, cost-effective, and easily applicable strategy compared with mechanical dilation in patients undergoing FLACS. However, the actual efficacy of intracameral mydriatics for the redilation and maintenance of mydriasis in pupillary constriction after femtosecond laser photodisruption was not fully elucidated and analyzed yet.
In the present study, we investigated the efficacy of a single intracameral injection of 0.015% epinephrine for pupil redilation in patients with significant miosis induced by femtosecond laser pretreatment during FLACS and quantitatively analyzed its effects on both the pupil diameter and area.
2. Methods
This retrospective study enrolled patients who underwent FLACS from December 2013 to September 2015 at Seoul St. Mary's Hospital, Seoul, South Korea. Institutional Review Board (IRB) approval was obtained (IRB no. KC14RISI0570), and the study was performed in accordance with the tenets of the Declaration of Helsinki. The patients were divided into 2 groups. The epinephrine group included patients who received a single bolus intracameral injection of 0.015% epinephrine for significant pupillary constriction to cover the capsulotomy margin at the initiation of phacoemulsification, while the no epinephrine group included patients with minimal miosis after femtosecond laser pretreatment who did not require epinephrine.
Patients with a history of intraocular surgery or a significant previous history of ocular trauma, those with pseudoexfoliation syndrome, those using glaucoma medications, and those with preoperative zonular weakness or poor pupil dilation (measured pupil diameter <5.5 mm) were excluded. Patients who had consumed systemic or topical steroids or NSAIDs within the previous 2 weeks or a systemic α1A-adrenoceptor antagonist such as tamsulosin were also excluded. All patients with available data pertaining to age, sex, the laterality of surgery, suction duration, and laser treatment duration were included.
2.1. Pupil dilation regimen
All patients in both groups received a mydriatic fixed-combination eye drop containing sympathomimetics and parasympatholytics (0.5% tropicamide and 0.5% phenylephrine; Mydrin-P, Santen Pharmaceutical Co., Ltd., Osaka, Japan) for preoperative mydriasis 3 or 4 times in the hour before femtosecond laser pretreatment. In case of insufficient pupil dilation (<5.5 mm), a dilating eye drop was administered once or twice. Preoperative NSAIDs were not used in the present study.
2.2. Intracameral epinephrine injection
Preservative-free (bisulfite-free) epinephrine is not available in South Korea. Therefore, preservative (bisulfite)-containing epinephrine was used. To minimize bisulfite toxicity in the corneal endothelium, 0.3 mL of bisulfite-containing (preservative-containing) 1:1000 (0.1%) epinephrine (DAIHAN Pharm., Seoul, South Korea) was diluted in 1.7 mL of balanced salt solution (BSS, Alcon Laboratories Inc., Fort Worth, TX)[24,25] to achieve a final concentration of 0.015%. In the epinephrine group, approximately 0.1 mL of diluted epinephrine was injected into the anterior chamber.
2.3. Parameters of femtosecond laser pretreatment
Following confirmation of sufficient pupillary dilation (≥5.5 mm), femtosecond laser pretreatment using the Catalys Precision Laser System (Johnson & Johnson Vision Care Inc., Jacksonville, FL) was performed for all patients. All laser procedures and cataract surgeries were performed under topical anesthesia. The capsulotomy size ranged from 4.9 to 5.8 mm, and the pulse energy was set at 4.0 μJ with a depth of 600 μm. Lens fragmentation was performed quadrant-wise with an 8/10 (anterior/posterior)-μJ pulse energy. The arcuate incision was created with an energy of 5 μJ. The primary and secondary laser incisions were created with a pulse energy of 6 μJ. Spot spacing (horizontal/vertical) of capsulotomy, lens fragmentation, and arcuate, primary, and sideport incision were 5/10, 10/40, 5/10, 4/8, and 3/5 μm, respectively. Width/length of primary and sideport incision were 2.3/1.1 and 1.1/1.1 mm, respectively. Following completion of the entire laser emission procedure, each patient was transferred to a day-surgery operation room. The phacoemulsification procedure was performed using the Infiniti Vision System (Alcon Laboratories, Fort Worth, TX) with the conventional technique. All femtosecond laser pretreatments and phacoemulsifications were performed by the same experienced surgeon (C-KJ).
2.4. Pupil area measurement
Measurements of the pupil area before femtosecond laser pretreatment and after each individual procedure of phacoemulsification were obtained using a previously described method.[16] Captured images derived from surgical video files of the femtosecond laser and phacoemulsification procedures were used. The pupil area during phacoemulsification was calculated before and after intracameral injection of 0.015% epinephrine, after injection of the ocular viscoelastic device, at the initiation and termination of phacoemulsification, at the removal of the lens cortex, and at the insertion of the intraocular lens (IOL). Both the pupil and capsulotomy areas for analysis of the actual pupil area were measured using ImageJ software (National Institutes of Health, Bethesda, MD).[26] To overcome the error of pupil area measurement according to magnification, we recalculated pupil area and diameter in video capture images at every time the surgeon adjusted the magnification during phacoemusification. The pupil area was calculated using the following proportional equation:
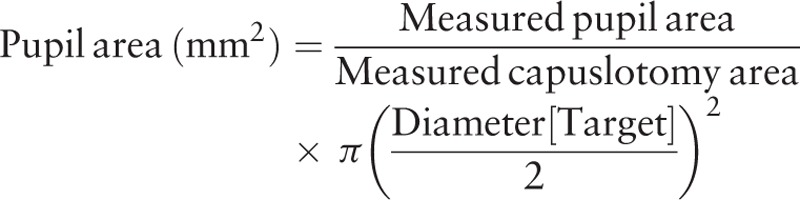 |
2.5. Statistical analyses
A paired t test was used to evaluate the efficacy of the single intracameral epinephrine injection for pupil redilation in the epinephrine group. An independent t test was used to compare the pupil areas before and after femtosecond laser pretreatment and after each phacoemulsification procedure. A chi-squared test was used to compare parameters such as sex and laterality of surgery. A P-value of <.05 was considered statistically significant, and all statistical analyses were performed using SPSS Statistics for Windows Version 12.0 (SPSS, Inc., Chicago, IL).
3. Results
3.1. Patient characteristics
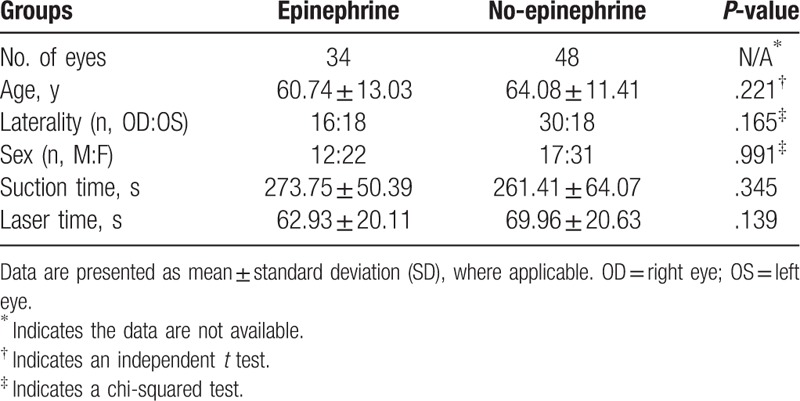
A total of 82 eyes of 82 patients, including 34 in the epinephrine group and 48 in the no epinephrine group, was included. The mean patient ages were 60.74 ± 13.03 and 64.08 ± 11.41 years in the epinephrine and no epinephrine groups, respectively, with no significant difference between groups (P = .221). Surgery was performed on the right side in 16 and 30 patients and the left side in 18 and 18 patients in the epinephrine and no epinephrine groups, respectively. The sex distribution (male/female) was 12/22 in the epinephrine group and 17/31 in the no epinephrine group. There were no significant differences in the laterality of surgery and sex distribution between the 2 groups (P = .165 and 0.991, respectively). The suction and laser treatment durations were 273.75 ± 50.39 and 261.41 ± 64.07 seconds, respectively, in the epinephrine group and 62.93 ± 20.11 and 69.96 ± 20.63 seconds, respectively, in the no epinephrine group, with no significant differences between groups (P = .345 and .139, respectively). The patient characteristics are shown in Table 1.
Table 1.
Characteristics of epinephrine and no-epinephrine patients who received femtosecond laser-assisted cataract surgery.
3.2. Efficacy of the single intracameral injection of 0.015% epinephrine
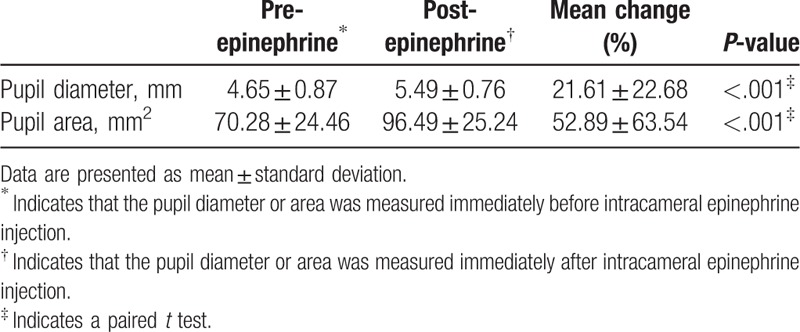
The mean pupil diameter significantly increased from 4.65 ± 0.87 to 5.49 ± 0.76 mm (21.61%) after the intracameral epinephrine injection (P < .001), while the mean pupil area significantly increased from 70.28 ± 24.46 to 96.49 ± 25.24 mm2 (52.89%; P < .001; Table 2).
Table 2.
Mean pupil diameter of the epinephrine group before and after the intracameral epinephrine injection.
3.3. Comparison of pupil diameters from femtosecond laser pretreatment to IOL implantation
The mean pupil diameters before laser pretreatment were not different between groups. Laser photodisruption induced miosis in both groups (epinephrine group: 7.13 ± 0.75–4.65 ± 0.87 mm, P < .001; no epinephrine group: 7.14 ± 0.61–6.30 ± 0.65 mm, P < .001). After laser pretreatment, the mean pupil diameter in the epinephrine group was significantly smaller than that in the no epinephrine group (6.30 ± 0.65 vs 4.65 ± 0.87 mm; P < .001). After intracameral epinephrine injection, the mean pupil diameter in the epinephrine group increased to 5.49 ± 0.76 mm. There was no significant difference between groups in the pupil diameter after additional viscomydriasis using ocular viscoelastic devices (epinephrine vs no epinephrine group: 6.10 ± 0.77 vs 6.39 ± 0.65, P = .073). The mean pupil diameter was additionally increased at the initiation of phacoemulsification by fluid infusion through the hand piece tubing to the anterior chamber, with the no epinephrine group exhibiting a slightly wider pupil (epinephrine group: 6.26 ± 0.99 mm, no epinephrine group: 6.74 ± 0.88 mm; P = .023). However, during phacoemulsification, the pupil diameter in the epinephrine and no epinephrine groups decreased to 6.01 ± 0.93 and 6.18 ± 0.94 mm, respectively (P = .418). At the end of phacoemulsification, there was no difference between the 2 groups (P = .418), and at the initiation of lens cortex removal and IOL implantation, the no epinephrine group exhibited wider pupils compared with the epinephrine group (cortex removal: P = .018, IOL implantation: P = .006). Although significant miosis occurred during femtosecond laser pretreatment, intracameral epinephrine induced redilation and maintained a pupil diameter of over 5.17 mm, which indicated the mean laser capsulotomy diameter (Fig. 1).
Figure 1.
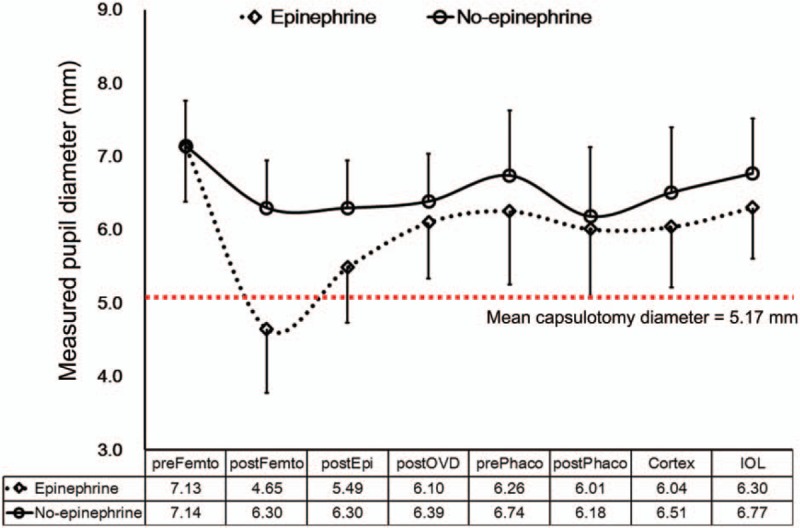
Serial measurements of the pupil diameter (mm) from femtosecond laser pretreatments to phacoemulsification procedures in patients who required 0.015% intracameral epinephrine (epinephrine group) for intraoperative miosis and those who did not (no epinephrine group). A single intracameral injection of 0.015% epinephrine resulted in significant redilation of miotic pupils in the epinephrine group. The degree of mydriasis after the intracameral injection of ocular viscoelastic devices until intraocular lens implantation was similar in the epinephrine and no epinephrine groups. preFemto indicates the pupil diameter calculated at the initiation of femtosecond laser pretreatment; postFemto indicates the pupil diameter measured immediately before epinephrine injection; postEpi and postOVD indicate the pupil diameter measured after intracameral epinephrine and ocular viscoelastic device injection, respectively; prePhaco and postPhaco indicate the pupil diameter at the initiation and termination of phacoemulsification, respectively; and Cortex and IOL indicate the pupil diameter calculated at the initiation of cortex fiber removal and intraocular lens implantation, respectively. IOL = intraocular lens.
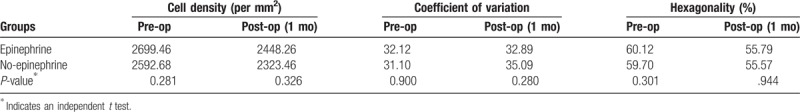
3.4. Comparisons of specular microscopy findings before and after FLACS
For evaluation of the toxicity of 0.015% intracameral epinephrine on corneal endothelial cells, we evaluated differences in cell density, the coefficient of variation, and hexagonality between the 2 groups using a specular microscope (Noncon ROBO-CA SP-8800, Konan Medical Inc., Tokyo, Japan). There were no significant differences between groups in the preoperative and 1-month postoperative endothelial cell density, coefficient of variation, and hexagonality (Table 3).
Table 3.
Comparisons of preoperative and 1-month postoperative specular microscope parameters between the epinephrine and no-epinephrine groups.
4. Discussion
Maintenance of adequate mydriasis is one of the most essential conditions necessary to perform cataract surgery without intraoperative complications and improve surgical outcomes. In the present study, we sought to confirm the efficacy of a single intracameral injection of 0.015% epinephrine for the maintenance of mydriasis during phacoemulsification and quantitatively determine its effects on pupillary constriction.
Relatively large-scale studies including early cases of FLACS have been reported,[1,13,14,16,27] and FLACS surgeons are aware of the occurrence of intraoperative miosis due to laser photodisruption. Therefore, to decrease the incidence of miosis during this procedure, modified dilating regimens or additional instillation of dilating agents between phacoemulsification and laser pretreatment have been suggested.[20,23,28–30] Nevertheless, intraoperative miosis still occurs. In the present study, we attempted to introduce and investigate the efficacy of a single intracameral epinephrine injection for the management of miosis caused by laser pretreatment, despite previously suggested preoperative modifications. To achieve our aim, we included patients with early FLACS who did not receive pretreatment with NSAID eye drops. Our findings suggested that miosis occurs at a greater rate and to a greater degree than usual, and we were able to evaluate the effects of intracameral epinephrine.
Miosis occurred after femtosecond laser pretreatment in all our patients, as reported previously. Compared with the mean pupil diameter of 6.30 ± 0.65 mm in the no epinephrine group, that in the epinephrine group decreased to 4.65 ± 0.87 mm and was significantly smaller than the established femtosecond laser capsulotomy diameter of 5.17 mm. However, immediately after intracameral epinephrine injection, pupil diameter increased to an average of 5.49 ± 0.76 mm, an increase of 21.6%. The average pupil area increased from 70.28 ± 24.46 to 96.49 ± 25.24 mm2, indicating that >50% of the surgical field was secured. With additional injection of ocular viscoelastic devices (viscomydriasis), the pupil diameter was further increased, with no statistically significant difference between the 2 groups. These results suggest that the intracameral epinephrine injection was very effective for redilation in patients with significant intraoperative miosis immediately after laser pretreatment.
Following redilation of miotic pupils with a single intracameral epinephrine injection, maintenance of adequate mydriasis would be another concern with regard to appropriate phacoemulsification of the lens nucleus or cortex cleavage. In the present study, pupil diameters were calculated sequentially after each procedure. Although the mean pupil diameter in the epinephrine group was significantly smaller than that in the no epinephrine group after each procedure during FLACS, a mean diameter of approximately 6.0 mm was maintained after the single epinephrine injection. Because the mean planned laser capsulotomy diameter is 5.17 mm, a 6.0-mm pupil diameter is adequate for cataract surgery procedures such as phacoemulsification, cortex removal, and IOL implantation.
Intracameral epinephrine injection, particularly in patients with intraoperative miosis, has been associated with endothelial toxicity due to preservatives and bisulfite-containing epinephrine.[31,32] However, bisulfite-free or preservative-free epinephrine is unavailable in South Korea and other countries.[33] Fortunately, direct intracameral injection of a 1:4 dilutions of bisulfite-containing epinephrine is not toxic to the corneal endothelium.[24,25] In the present study, we administered a single bolus intracameral injection of 0.3 mL epinephrine diluted with 1.7 mL of balanced salt solution (>5-fold dilution, 0.015% epinephrine hydrochloride). In addition, we evaluated the findings of specular microscopy to identify the effects of our regimen and found no significant difference in cell density, the coefficient of variation, and hexagonality between the 2 groups after 1 month.
One limitation of this study is that epinephrine was used to resolve the complication of intraoperative miosis, which is a surgical complication of FLACS. Therefore, it was not possible to conduct a prospective controlled study because the incidence was low. Therefore, the results of this study provide limited information on the efficacy of intracameral injection of 0.015% epinephrine for introperative miosis. Follow up studies such as prospective, multicenter study will be needed as the incidence of intraoperative miosis is low.
In conclusion, this study demonstrated the effectiveness of a single intracameral injection of 0.015% epinephrine for significant miosis due to femtosecond laser photodisruption during FLACS. The single injection could maintain the pupil diameter during the entire phacoemulsification procedure. Our findings suggest that this technique is practical and safe for the successful and uneventful completion of phacoemulsification in patients with significant miosis during FLACS.
Author contributions
Conceptualization: Jong Hwa Jun, Choun-Ki Joo.
Formal analysis: Seung Pil Bang, Young-Sik Yoo.
Investigation: Jong Hwa Jun, Young-Sik Yoo.
Methodology: Seung Pil Bang, Young-Sik Yoo.
Project administration: Choun-Ki Joo.
Visualization: Seung Pil Bang.
Writing – original draft: Jong Hwa Jun.
Footnotes
Abbreviations: FLACS = femtosecond laser-assisted cataract surgery, IOL = intraocular lens, NSAID = nonsteroidal anti-inflammatory drug.
Funding: This study was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2016R1A6A1A03010528) and the Korea Government (MSIP) (No. 2014R1A52010008).
There are no conflicts of interest to declare.
References
- [1].Nagy Z, Takacs A, Filkorn T, et al. Initial clinical evaluation of an intraocular femtosecond laser in cataract surgery. J Refract Surg 2009;25:1053–60. [DOI] [PubMed] [Google Scholar]
- [2].Friedman NJ, Palanker DV, Schuele G, et al. Femtosecond laser capsulotomy. J Cataract Refract Surg 2011;37:1189–98. [DOI] [PubMed] [Google Scholar]
- [3].Nagy ZZ, Kranitz K, Takacs AI, et al. Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. J Refract Surg 2011;27:564–9. [DOI] [PubMed] [Google Scholar]
- [4].Tackman RN, Kuri JV, Nichamin LD, et al. Anterior capsulotomy with an ultrashort-pulse laser. J Cataract Refract Surg 2011;37:819–24. [DOI] [PubMed] [Google Scholar]
- [5].Grewal DS, Basti S. Comparison of morphologic features of clear corneal incisions created with a femtosecond laser or a keratome. J Cataract Refract Surg 2014;40:521–30. [DOI] [PubMed] [Google Scholar]
- [6].Mastropasqua L, Toto L, Mastropasqua A, et al. Femtosecond laser versus manual clear corneal incision in cataract surgery. J Refract Surg 2014;30:27–33. [DOI] [PubMed] [Google Scholar]
- [7].Chan TC, Ng AL, Cheng GP, et al. Corneal astigmatism and aberrations after combined femtosecond-assisted phacoemulsification and arcuate keratotomy: two-year results. Am J Ophthalmol 2016;170:83–90. [DOI] [PubMed] [Google Scholar]
- [8].Wang L, Zhang S, Zhang Z, et al. Femtosecond laser penetrating corneal relaxing incisions combined with cataract surgery. J Cataract Refract Surg 2016;42:995–1002. [DOI] [PubMed] [Google Scholar]
- [9].Abell RG, Darian-Smith E, Kan JB, et al. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: outcomes and safety in more than 4000 cases at a single center. J Cataract Refract Surg 2015;41:47–52. [DOI] [PubMed] [Google Scholar]
- [10].Abell RG, Kerr NM, Howie AR, et al. Effect of femtosecond laser-assisted cataract surgery on the corneal endothelium. J Cataract Refract Surg 2014;40:1777–83. [DOI] [PubMed] [Google Scholar]
- [11].Chen X, Xiao W, Ye S, et al. Efficacy and safety of femtosecond laser-assisted cataract surgery versus conventional phacoemulsification for cataract: a meta-analysis of randomized controlled trials. Sci Rep 2015;5:13123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Popovic M, Campos-Moller X, Schlenker MB, et al. Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14 567 Eyes. Ophthalmology 2016;123:2113–26. [DOI] [PubMed] [Google Scholar]
- [13].Bali SJ, Hodge C, Lawless M, et al. Early experience with the femtosecond laser for cataract surgery. Ophthalmology 2012;119:891–9. [DOI] [PubMed] [Google Scholar]
- [14].Chang JS, Chen IN, Chan WM, et al. Initial evaluation of a femtosecond laser system in cataract surgery. J Cataract Refract Surg 2014;40:29–36. [DOI] [PubMed] [Google Scholar]
- [15].Nagy ZZ, Takacs AI, Filkorn T, et al. Complications of femtosecond laser-assisted cataract surgery. J Cataract Refract Surg 2014;40:20–8. [DOI] [PubMed] [Google Scholar]
- [16].Jun JH, Hwang KY, Chang SD, et al. Pupil-size alterations induced by photodisruption during femtosecond laser-assisted cataract surgery. J Cataract Refract Surg 2015;41:278–85. [DOI] [PubMed] [Google Scholar]
- [17].Schultz T, Joachim SC, Kuehn M, et al. Changes in prostaglandin levels in patients undergoing femtosecond laser-assisted cataract surgery. J Refract Surg 2013;29:742–7. [DOI] [PubMed] [Google Scholar]
- [18].Schultz T, Joachim SC, Stellbogen M, et al. Prostaglandin release during femtosecond laser-assisted cataract surgery: main inducer. J Refract Surg 2015;31:78–81. [DOI] [PubMed] [Google Scholar]
- [19].Cole DF, Unger WG. Proceedings: the involvement of prostaglandin in ocular trauma. Exp Eye Res 1973;17:395. [DOI] [PubMed] [Google Scholar]
- [20].Chen H, Lin H, Chen W, et al. Topical 0.1% bromfenac sodium for intraoperative miosis prevention and prostaglandin E2 inhibition in femtosecond laser-assisted cataract surgery. J Ocul Pharmacol Ther 2017;33:193–201. [DOI] [PubMed] [Google Scholar]
- [21].Diakonis VF, Kontadakis GA, Anagnostopoulos AG, et al. Effects of short-term preoperative topical ketorolac on pupil diameter in eyes undergoing femtosecond laser-assisted capsulotomy. J Refract Surg 2017;33:230–4. [DOI] [PubMed] [Google Scholar]
- [22].Schultz T, Joachim SC, Szuler M, et al. NSAID pretreatment inhibits prostaglandin release in femtosecond laser-assisted cataract surgery. J Refract Surg 2015;31:791–4. [DOI] [PubMed] [Google Scholar]
- [23].Jun JH, Yoo YS, Lim SA, et al. Effects of topical ketorolac tromethamine 0.45% on intraoperative miosis and prostaglandin E2 release during femtosecond laser-assisted cataract surgery. J Cataract Refract Surg 2017;43:492–7. [DOI] [PubMed] [Google Scholar]
- [24].Liou SW, Chiu CJ, Wang IJ. Effects of intraocular epinephrine on the corneal endothelium of rabbits. J Ocul Pharmacol Ther 2002;18:469–73. [DOI] [PubMed] [Google Scholar]
- [25].Hull DS. Effects of epinephrine, benzalkonium chloride, and intraocular miotics on corneal endothelium. South Med J 1979;72:1380–1. [DOI] [PubMed] [Google Scholar]
- [26].Hartig SM. Basic image analysis and manipulation in ImageJ. Curr Protoc Mol Biol 2013;102:14.15.1–2. Chapter 14:Unit14 15. [DOI] [PubMed] [Google Scholar]
- [27].Abell RG, Kerr NM, Vote BJ. Femtosecond laser-assisted cataract surgery compared with conventional cataract surgery. Clin Exp Ophthalmol 2013;41:455–62. [DOI] [PubMed] [Google Scholar]
- [28].Ventura BV, Ventura MC. Miosis secondary to femtosecond laser-assisted cataract surgery: redilation as a solution. J Refract Surg 2016;32:281–2. [DOI] [PubMed] [Google Scholar]
- [29].Yeoh R. Intraoperative miosis in femtosecond laser-assisted cataract surgery. J Cataract Refract Surg 2014;40:852–3. [DOI] [PubMed] [Google Scholar]
- [30].Kiss HJ, Takacs AI, Kranitz K, et al. One-day use of preoperative topical nonsteroidal anti-inflammatory drug prevents intraoperative prostaglandin level elevation during femtosecond laser-assisted cataract surgery. Curr Eye Res 2016;41:1064–7. [DOI] [PubMed] [Google Scholar]
- [31].Hull DS, Chemotti MT, Edelhauser HF, et al. Effect of epinephrine on the corneal edothelium. Am J Ophthalmol 1975;79:245–50. [DOI] [PubMed] [Google Scholar]
- [32].Edelhauser HF, Hyndiuk RA, Zeeb A, et al. Corneal edema and the intraocular use of epinephrine. Am J Ophthalmol 1982;93:327–33. [DOI] [PubMed] [Google Scholar]
- [33].Myers WG, Edelhauser HF. Shortage of bisulfite-free preservative-free epinephrine for intracameral use. J Cataract Refract Surg 2011;37:611. [DOI] [PubMed] [Google Scholar]


