Abstract
Objectives
Immigration into Europe has raised contrasting concerns about increased pressure on health services and equitable provision of health care to immigrants or ethnic minorities. Our objective was to find out if there were important differences in hospital use between the main ethnic groups in Scotland.
Study design
A census-based data linkage cohort study.
Methods
We anonymously linked Scotland's Census 2001 records for 4.62 million people, including their ethnic group, to National Health Service general hospitalisation records for 2001–2013. We used Poisson regression to calculate hospitalisation rate ratios (RRs) in 14 ethnic groups, presented as percentages of the White Scottish reference group (RR = 100), for males and females separately. We adjusted for age and socio-economic status and compared those born in the United Kingdom or the Republic of Ireland (UK/RoI) with elsewhere. We calculated mean lengths of hospital stay.
Results
9.79 million hospital admissions were analysed. Compared with the White Scottish, unadjusted RRs for both males and females in most groups were about 50–90, e.g. Chinese males 49 (95% confidence interval [CI] = 45–53) and Indian females 76 (95% CI 71–81). The exceptions were White Irish, males 120 (95% CI 117–124) and females 115 (95% CI 112–119) and Caribbean females, 103 (95% CI 85–126). Adjusting for age increased the RRs for most groups towards or above the reference. Socio-economic status had little effect. In many groups, those born outside the UK/RoI had lower admission rates. Unadjusted mean lengths of stay were substantially lower in most ethnic minorities.
Conclusions
Use of hospital beds in Scotland by most ethnic minorities was lower than by the White Scottish majority, largely explained by their younger average age. Other countries should use similar methods to assess their own experience.
Keywords: Ethnic groups, Hospitalisation, Data linkage cohort, Scotland
Highlights
-
•
We compared hospital use by ethnic groups via linkage to the Scotland Census 2001.
-
•
Hospital use by most ethnic groups was lower than hospital use by the White Scottish majority.
-
•
Younger average age and better health are probably the main explanations.
-
•
No evidence of overuse or underuse of hospital beds compared to the majority.
-
•
Other countries should similarly study healthcare use by migrants and ethnic groups.
Introduction
Most European countries are becoming ethnically more diverse because of an increase in arrivals of migrants. There is concern on the one hand about the consequent pressure on health services1, 2 and, on the other, about whether healthcare services are being equitably provided to migrants and ethnic minorities.3 However, information about health service use by migrants or ethnic minority groups in Europe is patchy and typically limited to specific services.4 To the best of our knowledge, only Spain and Norway have published recent analyses of actual health service use by migrants or ethnic minority groups across a regional or national health service.5, 6
As part of the United Kingdom (UK), Scotland carries out a census every 10 years. It should be completed by everyone who, on the day of the census, has lived or intends to live in the country for at least 3 months. Since 1991, self-defined ethnic group has been requested. The National Health Service in Scotland (NHS Scotland) generally offers free healthcare services to everyone, ‘ordinarily resident’, in the country. Thus, almost everyone completing the census should be eligible for free NHS health care.
The Scottish Health and Ethnicity Linkage Study (SHELS) has created a retrospective cohort of about 4.62 million people by linking Scotland's Census 2001 to NHS hospitalisation and other health records, thus enabling the relationship between ethnic group and health service use to be studied in detail.7 SHELS has found complex differences between ethnic groups in a wide range of specific conditions as measured by age-adjusted rates for hospitalisations and deaths combined.8, 9, 10 In this analysis, we aimed to find out if there are important differences between ethnic groups by overall general hospital admission rates and lengths of stay in Scotland. We judged that differences of more than 10% would be potentially important from a policy perspective.
Methods
Approvals and safeguards
Full ethical and other approvals for the data linkage, security and analyses in this study were granted by the Scottish Multicentre Ethics Committee and the Privacy Advisory Committee of NHS National Services Scotland. The anonymised data sets were only made available to named researchers with appropriate clearance and training in a secure environment at National Records of Scotland (NRS). All analyses and outputs followed the NRS Disclosure Control Guidance for SHELS and were cleared for release by its Disclosure Committee.
Study population
Methods used to develop the SHELS cohort have previously been described in detail.7 Individuals completing Scotland's Census 2001 form were asked to choose their ethnic group and those of household members from a list of 14 predefined categories. This was a legally required field and had a high completion rate (95.7%), with 100% availability following imputation carried out by NRS. Names, addresses, sex and dates of birth from Scotland's Census 2001 were confidentially linked to the Community Health Index (CHI), a register of people using the Scottish NHS with a unique number for each individual. The resulting look-up table had encrypted CHI and census numbers that could be used as a key to anonymously link the census to other health-related databases that included CHI numbers. About 4.62 million people whose census record included their ethnic group were linked, representing 91.3% of the estimated population of Scotland at the time and 95.1% of those completing the census. Supplementary Table 1 provides more detail.
Data selection and analysis
We selected all Scottish NHS general hospital admission records from 1 May 2001 to 30 April 2013 that could be linked to the census cohort. The denominators were person-years (PY), censored for death or transfer of registration from the NHS in Scotland to elsewhere in the UK and stratified by sex. We used Poisson regression with robust variance to calculate admission rates per 100,000 PY and unadjusted rate ratios (RRs) for each ethnic group with the White Scottish majority as the reference group. We multiplied RRs by 100 to be interpretable as percentages. The ‘All other ethnic group’ category in the census was not used because of its heterogeneity.
Using our standard method, we examined whether the associations between indicators of socio-economic position and outcome were similar across ethnic groups before entering them as confounding variables.11 The two indicators consistently associated in the same direction with the likelihood of admission across ethnic groups were highest educational qualification (individual level for people aged 16–74 years and household level for children and elderly) and housing tenure (owning or renting). We therefore adjusted rates for age, then, in addition, for education and housing tenure combined. We also calculated age-adjusted rates for each ethnic group and whether born in the United Kingdom and Republic of Ireland (UK/RoI) or elsewhere. We calculated geometric mean lengths of stay due to the high positive skew of the distribution. Day cases were counted as 0.5 days. Data were analysed using SAS V9.4 (SAS Institute Inc, Cary, North Carolina, USA).
Results
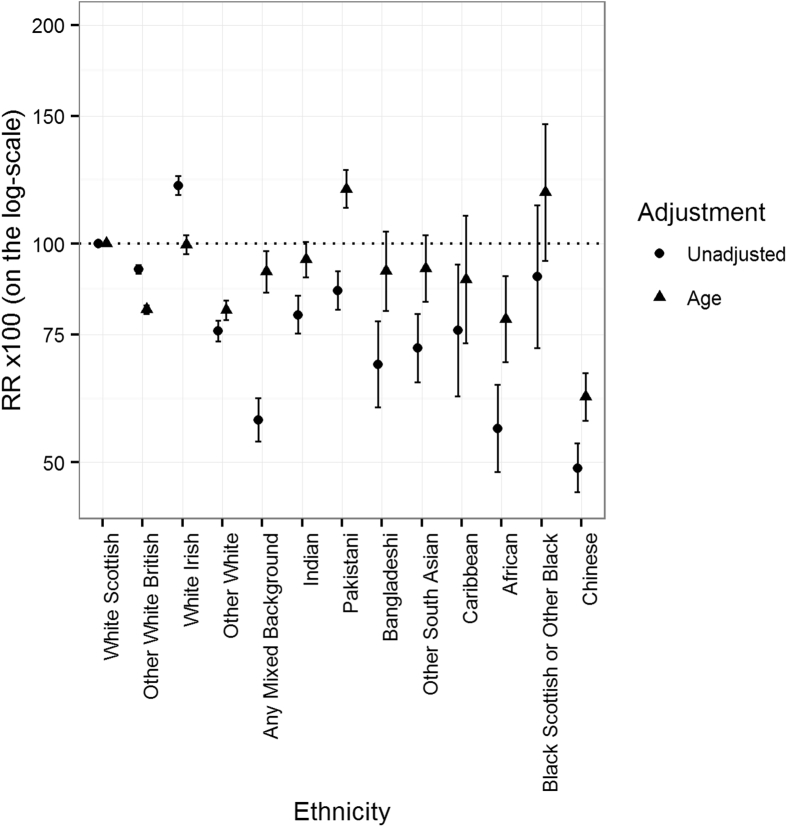
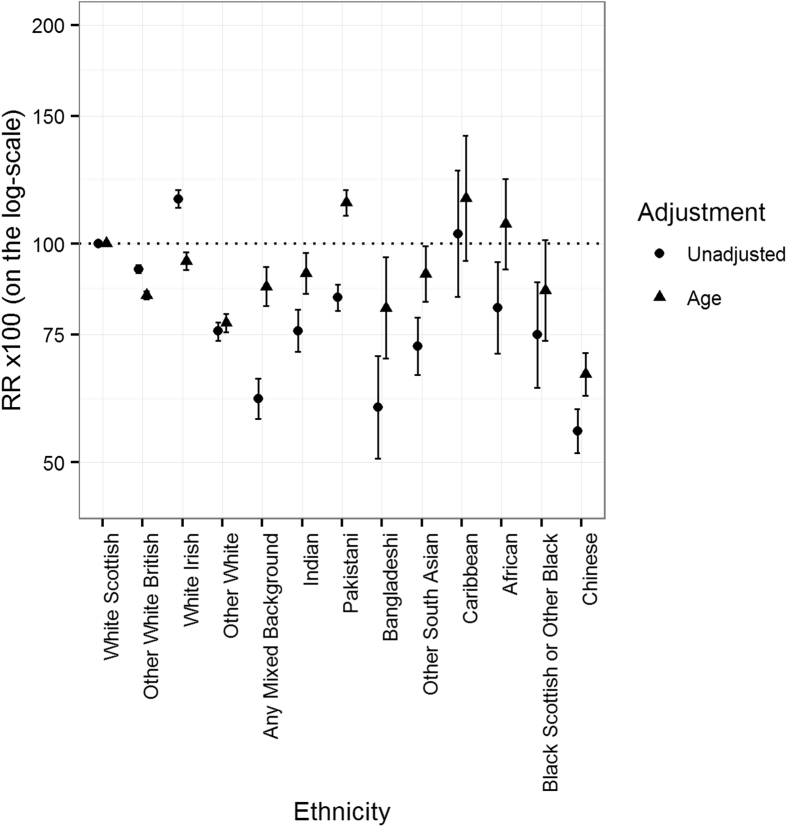
In 12 years of follow-up, there were 9.79 million hospital admissions of cohort members during 48.8 million PY of observation. Table 1 shows the number of admissions in each ethnic group by sex. Fig. 1, Fig. 2 show the unadjusted RRs for hospital admissions, comparing the other groups with the White Scottish (100), with 95% confidence intervals (CIs). Among males, the RRs of most groups were about 50–90, e.g. Chinese 49 (95% CI 46–53), African 56 (95% CI 49–64) and Bangladeshi 68 (95% CI 59–78). The exceptions were White Irish 120 (95% CI 117–124). Among females, there was a similar picture, e.g. Chinese 55 (95% CI 52–59), Bangladeshi 60 (95% CI 51–70) and Pakistani 84 (95% CI 81–88). The exceptions were Caribbeans 103 (95% CI 85–126) and White Irish 115 (95% CI 112–119).
Table 1.
Rate ratios (RRs) for hospitalisation after adjustment for age and age combined with educational attainment and housing tenure. White Scottish are the reference RR = 100 (95% confidence intervals).
| Ethnicity | Male |
Female |
||||
|---|---|---|---|---|---|---|
| Number of admissions | Age | Age & education/housing | Number of admissions | Age | Age & education/housing | |
| White Scottish | 4,160,850 | 100 | 100 | 4,726,955 | 100 | 100 |
| Other White British | 282,010 | 81 (80, 82) | 88 (87, 89) | 314,865 | 85 (84, 86) | 91 (89, 92) |
| White Irish | 47,350 | 100 (97, 103) | 100 (97, 103) | 51,725 | 95 (92, 97) | 97 (94, 99) |
| Other White | 40,240 | 81 (79, 84) | 84 (81, 87) | 49,745 | 78 (76, 80) | 82 (80, 84) |
| Mixed background | 6265 | 92 (86, 98) | 92 (86, 99) | 7610 | 87 (82, 93) | 88 (82, 93) |
| Indian | 10,250 | 95 (89, 101) | 103 (97, 109) | 9465 | 91 (85, 97) | 96 (90, 102) |
| Pakistani | 24,900 | 119 (112, 126) | 120 (113, 127) | 25,515 | 114 (109, 119) | 114 (109, 119) |
| Bangladeshi | 1160 | 92 (81, 104) | 92 (81, 105) | 860 | 82 (70, 96) | 80 (68, 94) |
| Other South Asian | 3730 | 92 (83, 103) | 94 (84, 104) | 3265 | 91 (83, 99) | 90 (83, 99) |
| Caribbean | 1055 | 89 (73, 109) | 91 (74, 111) | 1670 | 116 (95, 141) | 121 (99, 148) |
| African | 2095 | 79 (69, 90) | 80 (70, 91) | 2650 | 107 (92, 123) | 106 (91, 122) |
| Black Scottish or other Black | 835 | 118 (95, 146) | 113 (91, 141) | 760 | 86 (74, 101) | 83 (71, 98) |
| Chinese | 6460 | 62 (57, 66) | 61 (57, 66) | 7690 | 66 (62, 71) | 67 (63, 72) |
Fig. 1.
Unadjusted and age-adjusted ratios for all-cause hospitalisations of males by sex and ethnic group. The bars show the 95% CIs; the dotted line is the White Scottish reference (RR = 100). CI, confidence interval; RR, rate ratio.
Fig. 2.
Unadjusted and age-adjusted ratios for all-cause hospitalisations of females by sex and ethnic group. The bars show the 95% CIs; the dotted line is the White Scottish reference (RR = 100). CI, confidence interval; RR, rate ratio.
Fig. 1, Fig. 2 also show the age-adjusted RRs, representing the rates of admission if the age structure of the other groups were identical to that of the White Scottish. Among males, most adjusted RRs were closer to but still lower than that of the White Scottish, e.g. Chinese 62 (95% CI 57–66), African 79 (95% CI 69–90) and Bangladeshi 92 (95% CI 81–104). The exceptions were Pakistani 119 (95% CI 112–126) and Black Scottish/other Black 118 (95% CI 95–146) groups. Among females, the general effect of age adjustment was similar, with the adjusted RRs of Africans 106 (95% CI 92–123), Pakistanis 113 (95% CI 109–119) and Caribbeans 115 (95% CI 95–141) now higher than the White Scottish.
Influence of socio-economic status and place of birth
Table 1 shows that adjustment for socio-economic status had little effect, resulting in less than 10% change in the age-adjusted RRs for either males or females in all ethnic groups compared with the White Scottish majority. Table 2 categorises individuals in each ethnic group according to whether they were born in the UK/RoI or elsewhere. It shows that among males in 12 ethnic groups and females in nine, those born outside the UK/RoI had lower age-adjusted admission rates than those born in the UK/RoI. In 11 of the 21 groups, the difference was more than 10%. In contrast, females in four ethnic groups born outside the UK/RoI (i.e. Black Scottish, Chinese, Indian and Pakistani) had higher RRs than their counterparts born in the UK.
Table 2.
Rate ratios (RRs) for hospitalisation after adjustment for age, for persons born in the United Kingdom/Republic of Ireland (UK/RoI) or outside the UK/RoI. White Scottish born in UK/RoI are the reference RR = 100 (95% confidence intervals).
| Male |
Female |
|||
|---|---|---|---|---|
| Born in UK/RoI | Born outside UK/RoI | Born in UK/RoI | Born outside UK/RoI | |
| White Scottish | 100 | 88 (85, 91) | 100 | 98 (95, 101) |
| Other White British | 81 (80, 82) | 84 (79, 89) | 94 (92, 95) | 92 (88, 97) |
| White Irish | 100 (97, 103) | 76 (63, 92) | 96 (93, 99) | 93 (75, 116) |
| Other White | 86 (82, 91) | 79 (75, 82) | 93 (88, 97) | 81 (78, 84) |
| Any mixed background | 100 (92, 108) | 67 (59, 75) | 92 (86, 99) | 76 (67, 87) |
| Indian | 101 (90, 113) | 92 (87, 98) | 91 (80, 103) | 106 (98, 114) |
| Pakistani | 123 (108, 140) | 116 (110, 122) | 105 (99, 111) | 125 (118, 132) |
| Bangladeshi | 99 (85, 115) | 88 (74, 105) | 86 (67, 110) | 80 (65, 99) |
| Other South Asian | 116 (98, 137) | 82, (71, 93) | 100 (88, 114) | 86 (77, 97) |
| Caribbean | 113 (82, 154) | 69 (57, 82) | 135 (110, 165) | 106 (71, 158) |
| African | 104 (81, 133) | 71 (60, 84) | 143 (105, 194) | 92 (80, 107) |
| Black Scottish or other Black | 122 (93, 159) | 107 (76, 151) | 80 (66, 96) | 89 (67, 119) |
| Chinese | 59 (52, 66) | 62 (57, 68) | 60 (54, 66) | 73 (68, 80) |
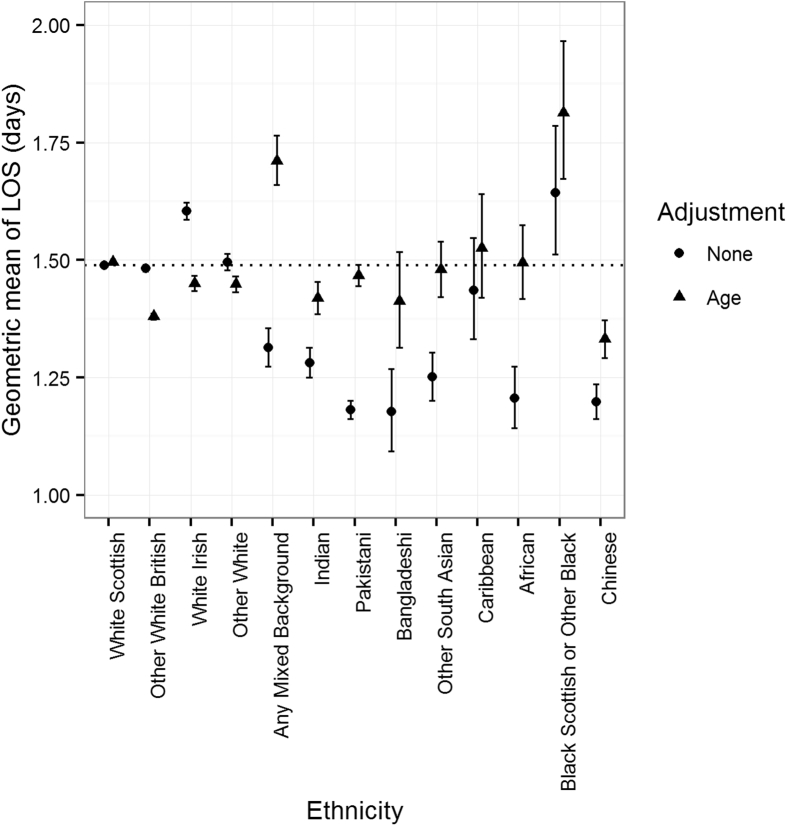
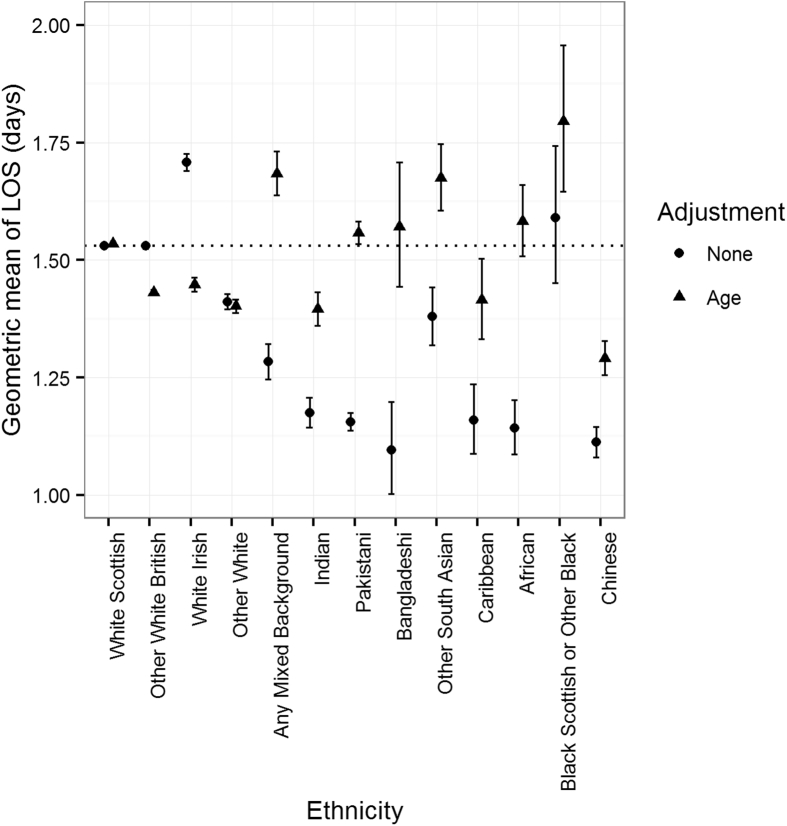
Length of stay
Fig. 3 shows that among males, almost all the non-White ethnic groups had shorter unadjusted mean lengths of stay than the White Scottish. Only the White Irish and Black Scottish had longer lengths of stay. A similar picture is seen for females in Fig. 4: most ethnic minorities had substantially shorter mean lengths of stay, with the White Irish being the only clear exception. Fig. 3, Fig. 4 also show that age adjustment had a large effect. It brought the average lengths of stay for most groups much closer to the White Scottish reference, with those of mixed background and Black Scottish males and females and other South Asian females becoming clearly longer than for the White Scottish. In contrast, those of both male and female other White British and White Irish became shorter than the White Scottish after age adjustment.
Fig. 3.
Unadjusted and age-adjusted geometric mean lengths of stay of males by sex and ethnic group. The bars show the 95% CI; the dotted line is the White Scottish mean as reference. CI, confidence interval; LOS, length of stay.
Fig. 4.
Unadjusted and age-adjusted geometric mean lengths of stay of females by sex and ethnic group. The bars show the 95% CI; the dotted line is the White Scottish mean as reference. CI, confidence interval LOS, length of stay
Discussion
Analysing almost 10 million general hospital admissions over 12 years, we found that the unadjusted admission rates of both males and females in most ethnic groups were substantially lower than those of the White Scottish majority. Adjusting for age generally reduced the differences and in some groups made them a little higher than the White Scottish, most notably Pakistani males and females. Adjusting for a combination of educational attainment and housing tenure had little effect. In a large majority of ethnic groups, people born outside the UK/RoI had lower age-adjusted admission rates. Unadjusted mean lengths of stay were generally shorter among the ethnic minorities. Thus, overall use of hospital beds by most ethnic minorities was lower than the overall use of hospital beds by the White Scottish majority, particularly by those born outside the UK/RoI.
The main strength of this study is that it is based on an unusually complete linked data set, covering the use of a national health service by a whole population over a long period of time. However, it would have excluded recent immigrants including refugees and asylum seekers whose residency in the UK was uncertain at the time of the census. It also focuses only on episodes of hospitalisation, providing no information on the use of primary care, emergency or out-patient services. Nevertheless, the findings are an important piece in the largely incomplete jigsaw of understanding how migrants and ethnic minorities use health services relative to the majority population and to each other.
A major impediment to carrying out analyses of hospital utilisation by ethnic group is the unreliable recording of patients' ethnic group in hospital record systems. A 1991 study using self-reported data from the General Household Survey of Great Britain found relatively small differences in hospitalisation rates between Whites, Indians, Pakistanis and Caribbeans. However, as the sample was restricted to persons aged 0–64 years and only included 1818 people from non-White groups, this may not have represented the true picture across the UK at that time.12 Since 1995, the UK legislation and policies have required ethnic monitoring of hospital utilisation in the UK with the aim of providing ‘equitable access to NHS services for all ethnic groups’.13 The value of doing this has been questioned, not least because of the relatively crude classification of ethnic groups.14 In practice, achieving a level of completeness of ethnic group recording sufficient to permit valid analyses has proved difficult. Until recently, only about 10% of routine hospital records in Scotland recorded the patient's ethnic group. With considerable effort, this has now been increased to around 80%,15 but completeness and accuracy are still not sufficient to provide reliable estimates of differences between ethnic groups.16 Linking Scotland's Census 2001 to hospitalisation records, with self-reported ethnic group recorded to a high level of completeness, largely overcomes this problem. It enables us to provide the first robust estimates of overall use of hospital beds by ethnic group for a large population in the UK.
An important question is whether lower use of services among immigrants or ethnic minorities is because they are healthier than the majority population or because their access to healthcare services is impeded. Reflecting the younger average age of minority groups in Scotland, we found that age-adjustment resulted in a rise of the admission rates and lengths of stays of most groups towards and in some cases above that of the majority. Another study of the same cohort found that most of the ethnic minorities in Scotland have higher life expectancies, suggesting better overall health.17 The relatively low rates of hospital admission for most ethnic minorities are thus in keeping with their younger age and relatively better health and unlikely to reflect inequitable service provision. Interestingly, the higher admission rates of members of ethnic groups born in the UK/RoI compared with those who migrated here, suggest some convergence by the former with the White Scottish majority in health status and/or health service usage.
How do our findings compare with those from elsewhere? A comprehensive analysis of health service use by around 1.25 million people in the Aragon Region of Spain, 11.9% of whom were immigrants,5 found that age-adjusted hospital admission rates were around 25% lower among adult immigrants from most world regions compared with the Spanish nationals. The difference narrowed somewhat after further adjustment for disease burden. Use of primary care was somewhat lower among immigrants, but emergency care was higher. There was greater variation among children. A smaller study in another region of Spain found foreign-born male patients had lower age-adjusted hospital admissions rates than those born in Spain, but rates among foreign-born females were higher.18 In a study of over 3.7 million people in Norway of whom 10.4% were immigrants, a lower proportion of immigrants than natives used primary-care and emergency-care services.6 However, immigrants using the services did so more frequently than natives. A systematic review of 21 European studies examining access to health care by immigrants in a range of primary-care, hospital out-patient and hospital in-patient settings reported a varied picture.4 Three out of the four small studies of hospitalisation found higher rates among immigrants. A systematic review of 37 studies in five European countries, the United States and Canada compared the use of primary-care services by immigrants and non-immigrants.19 It also found mixed results, with differences in service use being greatest in the United States. Together, these studies show there is no consistent picture: results vary according to the country, the service setting, the migrant or ethnic groups and the outcomes observed.
By using the Scottish 2001 Census population, our analysis excluded recent migrants including refugees and asylum seekers. Such individuals may not have the same entitlement to health care as other citizens in many countries. A 2016 report by the Migrant Integration Policy Index (MIPEX) on health services in 34, mainly, European countries used a consistent scoring system across four issues: migrants' entitlements to health services; accessibility of health services for migrants; responsiveness to migrants' needs; and measures to achieve change.3 The authors found considerable variation between countries, broadly related to gross domestic product, health expenditure and the proportion of the population who were migrants. While initiatives like the MIPEX report are important, they reflect laws and policies rather than actual experience. They should be backed up by studies that use robust data from whole populations or adequate samples to help us better understand the real healthcare experience of migrants and ethnic minorities and provide the evidence to help policymakers and service planners to respond appropriately.
In conclusion, our study found that than by ethnic minorities in Scotland was lower than the overall use of hospital beds by the White Scottish majority population. There was no evidence that this was either inequitable or would have caused disproportionate pressure on the hospital services. The ethnic make-up of the Scottish population is unique to Scotland. How its health service functions may differ considerably from those in other jurisdictions. Other countries should use similar methods to evaluate their performance.
Author statements
Ethical approval
Ethical approval for the data linkage, security and analyses was granted by the Scottish Multicentre Ethics Committee and the Privacy Advisory Committee of NHS National Services Scotland.
Funding
The authors thank the Chief Scientist Office for a grant (CZH/4/648), NHS Health Scotland for a supplementary grant (no number). SVK acknowledges funding from a NRS Senior Clinical Fellowship (SCAF/15/02), the Medical Research Council (MC_UU_12017/13 & MC_UU_12017/15) and Scottish Government Chief Scientist Office (SPHSU13 & SPHSU15). AS is supported by the Farr Institute.
Competing interests
None declared.
Author contributions
All authors contributed to the design of the study. Raj Bhopal was the principal investigator; Laurence Gruer chaired the study group including all the authors. Anne Douglas managed the study. Linda Williams, Geneviève Cézard and Markus Steiner carried out the statistical analysis. Laurence Gruer and Andrew Millard drafted the paper. All authors commented on all the drafts and approved the final version.
Other contributions
The Equality and Diversity Information Programme of the Information Services Division (ISD) of NHS National Services Scotland provided valuable support. ISD and National Records of Scotland made ‘in-house’ technical and advisory contributions to the work. Anne Houghton and Theresa Kirkpatrick gave administrative help. Colin Fischbacher as co-applicant helped to set the study up; Chris Povey was a co-investigator and had the idea of linking the census data to the data held by ISD and performed most of the linkage of census to CHI; Alex Stannard advised on use of census data; David Clark advised on and assisted with linkage to ISD databases; Jamie Pearce advised on data analysis particularly social and economic variables.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.puhe.2018.04.010.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.Scholz N. January 2016. The public health dimension of the European migrant crisis. European Parliamentary Research Service.http://www.europarl.europa.eu/RegData/etudes/BRIE/2016/573908/EPRS_BRI(2016)573908_EN.pdf Brussels. [Google Scholar]
- 2.Dyan M. Nuffield Trust; June 2016. The facts: EU migration and pressure on the NHS.https://www.nuffieldtrust.org.uk/resource/the-facts-eu-immigration-and-pressure-on-the-nhs [Google Scholar]
- 3.Summary report on the MIPEX Health Strand and Country Reports. International Organisation for Migration; Brussels: 2016. https://publications.iom.int/system/files/mrs_52.pdf [Google Scholar]
- 4.Norredam M., Nielsen S.S., Krasnik A. Migrants' utilization of somatic healthcare services in Europe–a systematic review. Eur J Public Health. 2010;20:555–563. doi: 10.1093/eurpub/ckp195. [DOI] [PubMed] [Google Scholar]
- 5.Gimeno-Feliu L., Calderon-Larranaga A., Diaz E., Poblador-Plou B., Macipe-Costa R., Prados-Torres A. Global health-care use by immigrants in Spain according to morbidity burden, area of origin and length of stay. BMC Public Health. 2016;16:450. doi: 10.1186/s12889-016-3127-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diaz E., Calderon-Larranaga A., Prado-Torres A., Poblador-Plou B., Gimenu-Feliu L. How do immigrants use primary health care services? A register-based study in Norway. Eur J Public Health. 2014;25(1):72–78. doi: 10.1093/eurpub/cku123. [DOI] [PubMed] [Google Scholar]
- 7.Bhopal R., Fischbacher C.M., Povey C., Chalmers J., Mueller G., Steiner M. Cohort profile: Scottish Health and Ethnicity Linkage Study of 4.65 million people exploring ethnic variations in disease in Scotland. Int J Epidemiol. 2011;40:1168–1175. doi: 10.1093/ije/dyq118. [DOI] [PubMed] [Google Scholar]
- 8.Bansal N., Fischbacher C.M., Bhopal R.S., Brown H., Steiner M., Capewell S. Myocardial infarction incidence and survival by ethnic group: Scottish Health and Ethnicity Linkage retrospective cohort study. BMJ Open. 2013;3:e003415. doi: 10.1136/bmjopen-2013-003415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simpson C., Steiner M., Cezard G., Bansal N., Fischbacher C., Douglas A. Ethnic variations in morbidity and mortality from lower respiratory tract infections: a retrospective cohort study. J Roy Soc Med. 2015;10–108:406–417. doi: 10.1177/0141076815588321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhopal R.S., Cezard G., Bansal N., Ward H.J.T., Bhala N. Ethnic variations in five lower gastrointestinal diseases: Scottish Health and Ethnicity Linkage Study. BMJ Open. 2014;4:e006120. doi: 10.1136/bmjopen-2014-006120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fischbacher C.M., Cezard G., Bhopal R.S., Pearce J., Bansal N. Measures of socioeconomic position are not consistently associated with ethnic differences in cardiovascular disease in Scotland: methods from the Scottish Health and Ethnicity Linkage Study (SHELS) Int J Epidemiol. 2014;43:129–139. doi: 10.1093/ije/dyt237. [DOI] [PubMed] [Google Scholar]
- 12.Balarajan R., Raleigh V., Yuen P. Hospital care among ethnic minorities in Britain. Health Trends. 1991;23:90–93. [PubMed] [Google Scholar]
- 13.NHS Executive Information Management Group . 2nd ed. Department of Health; London: 1994. Collecting ethnic group, data for admitted patient care: implementation guidance and training material. [Google Scholar]
- 14.Hilton C. Collecting ethnic group data for in-patients: is it useful? BMJ. 1996;313:923–925. doi: 10.1136/bmj.313.7062.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scotland I.S.D. January–March 2016. Improving ethnic data collection for equality and diversity monitoring.https://www.isdscotland.org/Health-Topics/Equality-and-Diversity/Publications/2016-08-30/2016-08-30-EDIP-Report.pdf [Google Scholar]
- 16.Knox S., Bhopal R., Buchanan D., Thomson C., Millard A., Fraser A., Gruer L. Scottish Public Health Observatory; June 2016. Using routinely collected data to compare hospital admission rates by ethnic group in Scotland.http://www.scotpho.org.uk/downloads/scotphoreports/scotpho160621-hospital-admissions-by-ethnic-group-v1.pdf [DOI] [PubMed] [Google Scholar]
- 17.Gruer L., Cezard G., Clark E., Douglas A., Steiner M., Millard A. Life expectancy of different ethnic groups using death records linked to population census data for 4.62 million people in Scotland. J Epidemiol Community Health. 2016;70:1251–1254. doi: 10.1136/jech-2016-207426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rue M., Cabre X., Soler-Gonzalez J., Bosch A., Almirall M., Xavier C. Emergency hospital services utilization in Lleida (Spain): a cross-sectional study of immigrant and Spanish-born populations. BMC Health Serv Res. 2008;8:81. doi: 10.1186/1472-6963-8-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uiters E., Deville W., Foets M., Spreeuwenberg P., Groenewegen P. Differences between immigrant and non-immigrant groups in the use of primary medical care; a systematic review. BMC Health Serv Res. 2009;9:76. doi: 10.1186/1472-6963-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.