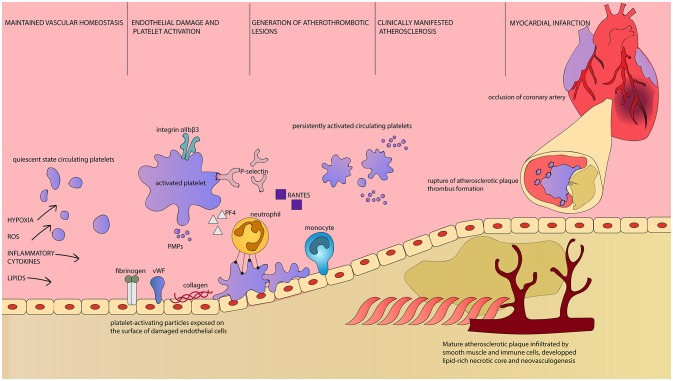
Figure 1.
Platelets as first and final effector cells in atherogenesis and its complications. Intermittent hypoxia, oxidative stress, elevated concentration of circulating inflammatory cytokines, and lipids are factors leading to disruption of vascular homeostasis in OSA patients. Parallel to endothelial damage and demonstration of otherwise unexposed molecules, platelet activation occurs. Activated platelets are characterized by increased surface area, upregulation of surface receptors and release of PMPs as well as plethora of bioactive substances (106). Reorganization of platelet integrin αIIbβ3 conformation enables fibrinogen binding and platelet aggregation (107). P-selectin is both exposed on the surface of platelets and released. It is essential for leukocyte recruitment and enables adhesion between platelets and neutrophils, as well as platelet aggregation. Platelet-derived RANTES is deposited on endothelial cells and allows monocyte arrest and infiltration. PF4 attracts neutrophils, but also interacts with endothelial LDL receptor and promotes lipid peroxidation. PMPs are highly coagulant carriers of platelet-derived molecules, including regulatory miRNA. Platelet-neutrophil interaction is dependent on the aforementioned P-selectin and PF4 as well as CD40L and GP1βα along with their ligands expressed on the surface of neutrophil, respectively PSGL-1, CD40, Mac1 and CCL5 (89). Platelets enhance neutrophil extracellular traps formation and neutrophil oxidative burst, which can lead to tissue damage. Persistent platelet activation results in constant presence of proinflammatory and proatherogenic substances, immune cells infiltration of the endothelium and consequently, to the development of atherosclerotic plaques. Clinical manifestation of atherosclerosis indicates the presence of mature plaques with rich in lipids necrotic core, neovascularization and fragile fibrous cap. At this time, circulating platelets display prothrombotic phenotype and are easily activated. Rupture of such atherosclerotic plaque results in rapid thrombus formation. It can lead to occlusion of critical arteries, including coronary vessels, and dramatical/major consequences. ROS, Reactive Oxygen Species; vWF, von Willebrandt Factor; PMPs, Platelet-derived Microparticles; PF4, Platelet Factor 4; Integrin αIIbβ3, glycoprotein IIb/IIIa; GP1βα, glycoprotein Ib alpha chain; RANTES, regulated on activation, normal T-cell expressed and secreted, CCL5; CD40L, CD40 Ligand, CD154; PSGL-1, P-selectin glycoprotein ligand-1; CD40, Cluster of differentiation 40; Mac1, Macrophage-1 antigen, integrin αMβ2.