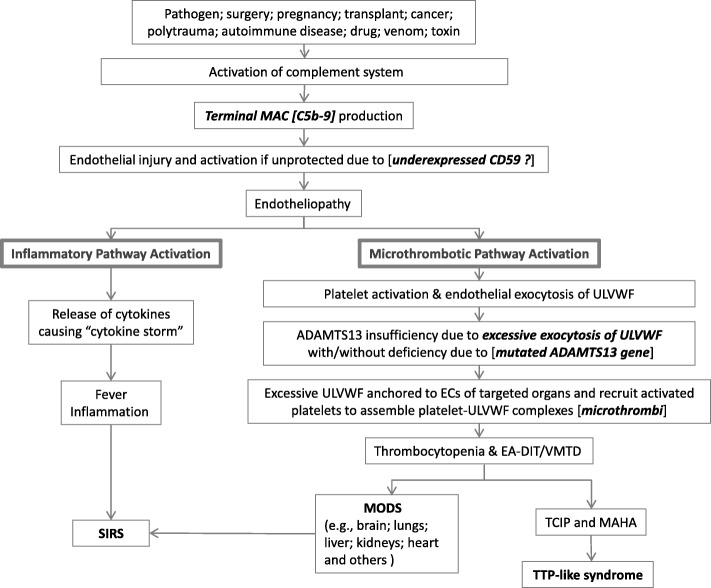
Fig. 1.
Molecular pathogenesis of TTP-like syndrome Fig. 1 elaborates “two activation theory of the endothelium”, which shows complement-induced endothelial molecular events, leading to endotheliopathy-associated DIT (i.e., TTP-like syndrome) and MODS. The organ phenotype syndrome in MODS includes encephalopathy, ARDS, AFHF, ARF/HUS, MI, AI, pancreatitis, rhabdomyolysis, "DIC", HELLPs, SS, and others. For example, in sepsis complement activation is the initial critical event. Complement activation can occur through one of three different pathways (i.e., classical, alternate and lectin). In addition to lysis of pathogen by terminal product C5b-9, it could induce endotheliopathy to the innocent bystander ECs of the host. C5b-9-induced endotheliopathy is suspected to occur if the endothelium is “unprotected” by CD59. Activated inflammatory pathway provokes inflammation in sepsis, but inflammation could be modest if the number of organ involvement is limited. Activated microthrombotic pathway results in endotheliopathy-associated DIT if the excess of ULVWF develops following endothelial exocytosis as a result of relative insufficiency of ADAMTS13 with/without mild to moderate ADAMTS13 deficiency, which is associated with heterozygous gene mutation or polymorphism of the gene. This theory explains all the manifestations of VMTD as illustrated in the Fig. 1. Abbreviations: AFHF, acute fulminant hepatic failure; AI, adrenal insufficiency; ARDS, acute respiratory distress syndrome; ARF, acute renal failure; “DIC”, false disseminated intravascular coagulation; DIT, disseminated intravascular microthrombosis; ECs, endothelial cells; EA-DIT, endotheliopathy-associated DIT; HELLPs, hemolysis, elevated liver enzymes, and low platelet syndrome; HUS, hemolytic uremic syndrome; MI, myocardial infarction; MODS, multi-organ dysfunction syndrome; MAHA, microangiopathic hemolytic anemia; SIRS, systemic inflammatory response syndrome; SS, stroke syndrome; TCIP, thrombocytopenia in critically ill patient; TTP, thrombotic thrombocytopenic purpura; ULVWF, unusually large von Willebrand factor; VMTD, vascular microthrombotic disease