Supplemental digital content is available in the text.
Key Words: Dysphagia, Lower Esophageal Sphincter, Manometry, Negative Pressure
Abstract
Herein, we present a case of a patient with Wallenberg syndrome with severe bulbar dysphagia who discovered a unique swallowing method: creating strong negative pressure in the esophagus to improve pharyngeal passage of a bolus. A 47-yr-old man presented with a subarachnoid hemorrhage secondary to a ruptured aneurysm in the right vertebral artery. After coil embolization, he experienced severe dysphagia due to Wallenberg syndrome and required tube feeding. Eighty-one days after the onset of the stroke, a videofluoroscopic swallowing evaluation revealed that the bolus was rapidly sucked into the esophagus. High-resolution manometry showed weak constriction of the pharynx simultaneous with forced, voluntary constriction of the diaphragm before swallowing; this created negative pressure in the esophagus. The authors named this unique swallowing method “vacuum swallowing.” Ultimately, the patient was able to eat an ordinary diet via the use of this technique. Vacuum swallowing is a unique method of improving pharyngeal passage of a bolus by creating strong negative pressure in the esophagus. Additional studies are necessary to determine whether vacuum swallowing can be successfully used for other forms of dysphagia.
Dysphagia is a common complication of stroke. Wallenberg syndrome is a type of brainstem stroke. The swallowing center, which is located in the medulla, controls and manipulates the oropharyngeal phase of the swallowing sequence. Therefore, patients with brainstem stroke may experience deficits in pharyngeal and upper esophageal sphincter (UES) function, such as UES and pharyngeal incoordination, abnormal UES relaxation and closure, and weak pharyngeal contraction.1 The incidence of dysphagia accompanying Wallenberg syndrome after lateral medullary infarction reportedly ranges from 50% to 100%.2–4
High-resolution manometry (HRM) is a relatively new method for assessing esophageal pressure characteristics,5 and it can be used to measure pressure from the pharynx to the stomach via closely spaced pressure transducers. Furthermore, the use of solid-state pressure sensors instead of conventional water-perfused pressure sensors enables faster response rates to pressure changes. The technique facilitates more detailed assessment of pharyngeal and esophageal pressure characteristics and makes it possible to study the relationships between pressures in the stomach, lower esophageal sphincter, UES, and esophageal body in detail.6
Herein, a case of a patient with Wallenberg syndrome with severe bulbar dysphagia who discovered a unique swallowing method in improving pharyngeal passage of a bolus by creating strong negative pressure in the esophagus using HRM is described.
CASE
A 47-yr-old man presented with disturbance of consciousness and was taken to the emergency department and intubated for airway protection. Initial computed tomography as well as computed tomography angiography of the head revealed subarachnoid hemorrhage secondary to an aneurysm rupture of the right vertebral artery. His medical history included dissection of a left vertebral artery when he was 40 yrs old, and he had no symptoms. After coil embolization of the aneurysm, diffusion weighted imaging showed a high signal (hyperintensity) representing a right medullary lateral infarction that included the nucleus ambiguus. He exhibited severe dysphagia classified as level 2 via the Food Intake Level Scale (FILS)7 (swallowing training not using food is performed),7 and he was fed by tube (Table 1). Forty-six days after onset, he was transferred to the rehabilitation department of the hospital for dysphagia rehabilitation. He had mild truncal ataxia, but no paralysis or dysmetria. He could walk well without a cane or walker. Sensory examination revealed reduced temperature and pinprick sensations on the left side of his face and body. He had severe dysphagia and was expectorating saliva into a tissue. On day 49, a videoendoscopic examination of swallowing revealed pooling of saliva in the valleculae. A videofluoroscopic examination (VF) of swallowing revealed that pharyngeal contraction was weakened and the UES did not open. A small amount of jelly and thickened liquid was used to evaluate swallowing function, but the bolus did not pass through the pharynx and remained in the pyriform sinus (Video 1, Supplemental Digital Content 1, http://links.lww.com/PHM/A531). At that time, his ability to swallow was estimated to be level 3 (swallowing training using a small quantity of food is performed) using the FILS. He was fed via intermittent oro-esophageal tube feeding. He received 20–40 mins of dysphagia rehabilitation once a day, 5 days a week from a speech-language pathologist who employed balloon dilatation therapy,8 Shaker exercise,9 breathing training, and lingual resistance exercise.10 In addition to receiving dysphagia rehabilitation, the patient also self-administered balloon dilatation therapy. The speech-language pathologist assessed respiratory condition, voice, and cough reflex and monitored oxygen saturation during the rehabilitation sessions. He also received direct swallowing training using jelly and thickened liquid after balloon dilatation therapy, but even with very small amounts, some was still coughed up. The effectiveness of balloon dilatation therapy was confirmed via videoendoscopic examination of swallowing at the bedside, but improvement of the UES relaxation was insufficient. The jelly and thickened liquid did not pass completely through the pharynx and again pooled in the pyriform sinus. Ten weeks after the onset of the stroke, he reported that he could swallow more easily if he forcefully contracted his abdominal muscles while elevating his shoulders. On day 81, VF revealed that his swallowing function had improved (Video 1, Supplemental Digital Content 1, http://links.lww.com/PHM/A531). Jelly, thickened liquid, crushed agar, and natural liquid were used to evaluate the swallowing function. Although the pharyngeal contraction was weak, the relaxation of UES was improved when compared with that observed during the first examination. The pharyngeal passage of the bolus was improved, and the amounts of the valleculae and pyriform sinus residues were significantly reduced. At that time, his ability to swallow was estimated to be level 5 (easy-to-swallow food is orally ingested in one to two meals, but alternative nutrition is also given) via the FILS. Oral ingestion of a paste diet was started. On day 85, his dysphagia improved to FILS level 7 (easy-to-swallow food is orally ingested in three meals, no alternative nutrition is given). Intermittent oro-esophageal tube feeding was terminated, and oral ingestion of a dysphagia diet was implemented. On day 103, his swallowing function improved to FILS level 8 (the patient eats three meals by excluding food that is particularly difficult to swallow).
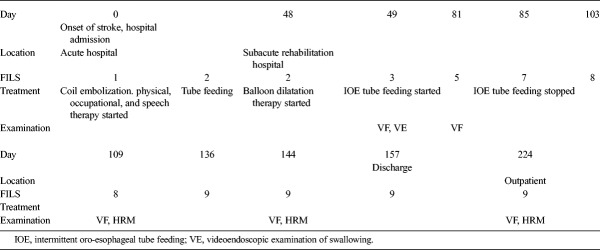
TABLE 1.
Clinical course and treatment timeline
On day 109, VF and HRM were performed. Videofluoroscopic examination showed that the pharyngeal passage speed of the bolus was high enough to be completely swallowed; the bolus was passed by being sucked into the esophagus despite the weak pharyngeal contraction (Video 1, Supplemental Digital Content 1, http://links.lww.com/PHM/A531). The bolus passed through the esophagus body to the bottom, without delay. The swallowing pressure along the velopharynx and upper esophagus was measured using HRM. There was weak constriction of the pharynx, and the patient created negative pressure in the upper esophagus. The maximum pressure in the pharynx was 53.4 mm Hg, which is consistent with oropharyngeal weakness. Negative pressure was observed in the esophagus, and the minimum pressure in the upper esophagus was −69.2 mm Hg. On day 136, his dysphagia improved to FILS level 9 (no dietary restriction, and the patient ingests three meals orally, but medical considerations are given).
Follow-up HRM and VF were performed 144 days after the onset of the stroke. High-resolution manometry during swallowing revealed forceful constriction of the lower esophageal sphincter muscle zone, which created the negative pressure in the esophagus (Fig. 1). The maximum pressure of the lower esophageal sphincter was 193.7 mm Hg, and the minimum pressure was −73.4 mm Hg. Swallowing function was evaluated with various types of boli including jelly, thickened liquid, crushed agar, normal liquid, and cookies. Jelly with low adhesion was inhaled into the lower esophagus extremely rapidly during swallowing (Video 1, Supplemental Digital Content 1, http://links.lww.com/PHM/A531). Videofluoroscopic examination of the esophageal stage in the sitting position revealed strong downward movement of the diaphragm during swallowing. The patient was discharged home 157 days after stroke.
FIGURE 1.
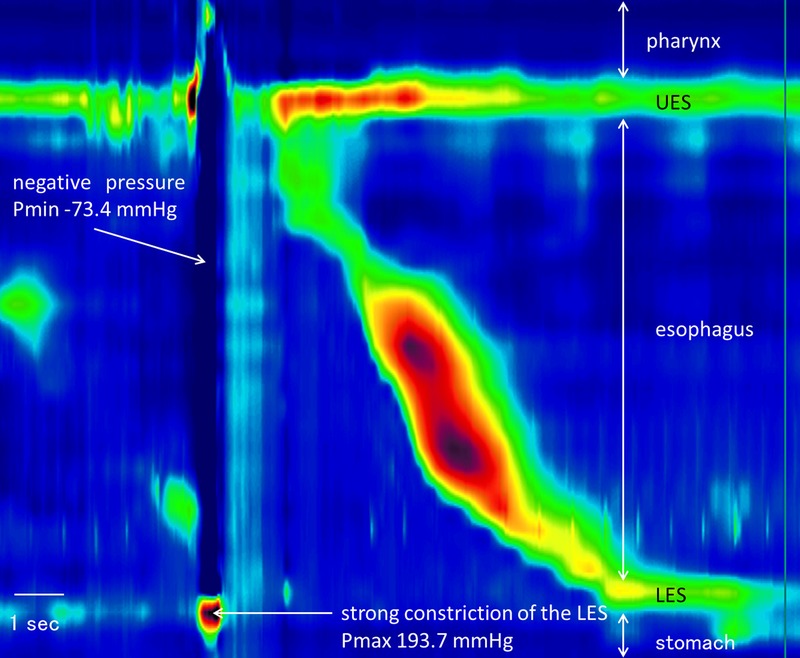
Vacuum swallowing characterized by creating negative pressure in the esophageal body.
After discharge, the patient was able to eat a regular diet without any restrictions. On day 224, the findings of follow-up VF and HRM were similar to those of the previous examinations; since that follow-up, he has not shown events associated with a swallowing disorder and his oral intake has remained stable.
The patient provided informed consent to publication of his case. The investigations and case study were performed in accordance with the ethical standards established in the 1964 Declaration of Helsinki and later amendments, as well as ethical guidelines for medical and health research involving human subjects in Japan. This study conforms to all case reports guidelines and reports the required information accordingly (see Checklist, Supplemental Digital Content 2, http://links.lww.com/PHM/A532).
DISCUSSION
To our knowledge, this is the first report describing a unique swallowing method to improve pharyngeal passage of a bolus by creating negative pressure in the esophageal lumen via forced voluntary constriction of the diaphragm before swallowing. The authors named this swallowing method “vacuum swallowing,” because the bolus is sucked into the esophagus from the weakly constricted pharynx during swallowing.
In a previous study, during swallowing the respective mean maximum values of pressures at the velopharynx and tongue base in a group of healthy subjects were 191.76 (77.99) and 149.61 (34.06) mm Hg.11 In the present case, the pharyngeal maximum pressure was 53.4 mm Hg. The patient had significantly reduced maximum pressure in the pharynx during swallowing compared with that of normal subjects. Conversely, he exhibited strong negative pressure in the esophagus during swallowing, and the minimum esophageal pressure was −73.4 mm Hg. In a previous study, the esophageal minimum pressure was −10.7 (6.0) mm Hg (n = 10) in healthy subjects. The subjects in that study did not create more negative pressure during swallowing. Pharyngeal contraction was very weak in the patient in the current study, and he created strong negative pressure in the esophageal body via contraction of the diaphragm. This pressure gradient between the pharynx and the esophageal body during swallowing was a very unique finding.
In the present case, a specific pattern of esophageal pressure characteristics was observed during the act of vacuum swallowing in HRM and VF. The mechanism of vacuum swallowing was characterized by a pressure increase at the part of the esophagogastric junction and simultaneous movement of the diaphragm in a downward direction. Via VF, the authors observed downward movement of the diaphragm consistent with the contraction of the diaphragm. The movement pattern of the diaphragm created a sudden reduction in pressure in the esophageal body.
Vacuum swallowing is characterized by the creation of negative pressure in the thoracic cavity via movement of the diaphragm in a downward direction similar to a strong deep inspiration. The patient elevated his shoulders while swallowing, which is also similar to what occurs during strong deep inspiration. He may be employing contraction of accessory muscles of respiration. In this mechanism, the driving force behind the sudden influx of the bolus into the esophageal body is the pressure gradient between the weak pharyngeal pressure and negative intraesophageal pressure.
In Wallenberg syndrome patients with bulbar dysphagia, balloon dilatation,8 Shaker exercise,9 botulinum toxin type A injection,12 and cricopharyngeal myotomy13 have been shown to be beneficial in those with failed UES relaxation. In the present case, however, the patient discovered a unique swallowing technique to improve the pharyngeal passage of a bolus by himself. This swallowing method is very likely a compensatory method and independent of the neural mechanism underlying bulbar palsy. It is unclear whether this method would be effective in other patients with similar etiologies of dysphagia or in other types of dysphagia.
Although this patient did not experience adverse events using this swallowing method, others may need to be attentive to such possibilities, including the risk of aspiration caused by uncoordinated breathing and swallowing. It is also unclear what effect this swallowing method has on the esophagus over time; however, the patient in this study did not have symptoms related to the esophagus (e.g., reflux esophagitis).
In conclusion, vacuum swallowing is a unique method of improving pharyngeal passage of a bolus in which strong negative pressure in the esophagus is created to suck the bolus past the pharynx. It was successful for this patient, but it is unclear whether it can be effective for other patients or for other forms of dysphagia; it is also unclear whether it can be taught therapeutically. Additional studies are necessary to determine whether vacuum swallowing can be successfully used for other forms of dysphagia.
Supplementary Material
Footnotes
KK, SK, and IF contributed in the following: conception and design of the study, analyzing and interpreting data, drafting, revising the article, and approval of the final version of the article.
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.ajpmr.com).
REFERENCES
- 1.Martino R, Foley N, Bhogal S, et al. : Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 2015;36:2756–63 [DOI] [PubMed] [Google Scholar]
- 2.Sacco RL, Freddo L, Bello JA, et al. : Wallenberg's lateral medullary syndrome. Clinical-magnetic resonance imaging correlations. Arch Neurol 1993;50:609–14 [DOI] [PubMed] [Google Scholar]
- 3.Currier RD, Giles CL, Dejong RN: Some comments on Wallenberg's syndrome. An analysis and clinico-anatomic correlation of certain symptoms associated with the “posterior inferior cerebellar artery syndrome”. Trans Am Neurol Assoc 1960;85:36–41 [PubMed] [Google Scholar]
- 4.Kameda W, Kawanami T, Kurita K, et al. : Lateral and medial medullary infarction: a comparative analysis of 214 patients. Stroke 2004;35:694–9 [DOI] [PubMed] [Google Scholar]
- 5.Kessing BF, Smout AJ, Bredenoord AJ: Clinical applications of esophageal impedance monitoring and high-resolution manometry. Curr Gastroenterol Rep 2012;14:197–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessing BF, Bredenoord AJ, Smout AJ: Mechanisms of gastric and supragastric belching: a study using concurrent high-resolution manometry and impedance monitoring. Neurogastroenterol Motil 2012;24:573–9 [DOI] [PubMed] [Google Scholar]
- 7.Kunieda K, Ohno T, Fujishima I, et al. : Reliability and validity of a tool to measure the severity of dysphagia: the Food Intake LEVEL Scale. J Pain Symptom Manage 2013;46:201–6 [DOI] [PubMed] [Google Scholar]
- 8.Rees CJ, Fordham T, Belafsky PC: Transnasal balloon dilation of the esophagus. Arch Otolaryngol Head Neck Surg 2009;135:781–3 [DOI] [PubMed] [Google Scholar]
- 9.Logemann JA, Rademaker A, Pauloski BR, et al. : A randomized study comparing the Shaker exercise with traditional therapy: a preliminary study. Dysphagia 2009;24:403–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robbins J, Kays SA, Gangnon RE, et al. : The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil 2007;88:150–8 [DOI] [PubMed] [Google Scholar]
- 11.Park D, Shin CM, Ryu JS: Effect of different viscosities on pharyngeal pressure during swallowing: a study using high-resolution manometry. Arch Phys Med Rehabil 2017;98:487–94 [DOI] [PubMed] [Google Scholar]
- 12.Lee SY, Seo HG, Paik NJ: Botulinum toxin injection for dysphagia: a blinded retrospective videofluoroscopic swallowing study analysis. Am J Phys Med Rehabil 2009;88:491–4 [DOI] [PubMed] [Google Scholar]
- 13.Muñoz AA, Shapiro J, Cuddy LD, et al. : Videofluoroscopic findings in dysphagic patients with cricopharyngeal dysfunction: before and after open cricopharyngeal myotomy. Ann Otol Rhinol Laryngol 2007;116:49–56 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.