Abstract
This pilot study examined the efficacy and acceptability of a self-guided and culturally modified internet-delivered Cognitive Behaviour Therapy (iCBT) treatment for Arab people, aged 18 and over, with symptoms of depression and anxiety. Thirty-six participants from seven countries, with at least mild symptoms of depression (Patient Health Questionnaire 9-item; PHQ-9; total scores ≥ 5) or anxiety (Generalised Anxiety Disorder 7-item; GAD-7; total scores ≥ 5) accessed the online Arabic Wellbeing Course, which consisted of five online lessons delivered over eight weeks and presented in the English language. Standard measures of depression, anxiety, distress and disability were administered at pre-treatment, post-treatment and 3-month follow-up. Thirty-six percent of participants completed the five lessons over eight weeks, with 61% and 36% providing post-treatment and 3-month follow-up data respectively. Participants reported significant improvements (within-group Cohen's d; avg. reduction) in depression (ds ≥ 1.20; avg. reduction ≥ 46%), anxiety (ds ≥ 1.15; avg. reduction ≥ 45%), disability (ds ≥ 0.81; avg. reduction ≥ 35%) and psychological distress (ds ≥ 0.91; avg. reduction ≥ 24%) immediately post-treatment, which were sustained at or further improved to 3-month follow-up. Participants rated the Arabic Wellbeing Course as acceptable. Notwithstanding the absence of a control group, low follow-up questionnaire completion rates and the Course not being translated in Arabic, these results are encouraging and contribute to a growing body of literature indicating that, with minor modifications, internet-delivered interventions have the potential of increasing access to treatment for immigrant groups.
Keywords: Arabs, Anxiety, Depression, Internet-delivered treatment, Transdiagnostic
1. Introduction
Anxiety and major depressive disorders are among the most common mental conditions in the Western (Kessler et al., 2009, Slade et al., 2009) and Arab worlds, as reflected in epidemiological surveys conducted in Lebanon (Karam et al., 2006), Iraq (Alhasnawi et al., 2009), Morocco (Kadri et al., 2010) and Egypt (Ghanem et al., 2009). The Arab world refers to countries from the Middle East and North Africa where Arabic is the national language, has a current population of 377 million (The World Bank, 2014), and represents 5.4% of the world's population.
Unfortunately, recent studies indicate that only a small minority of Arab people with mental health problems seek treatment. For example, a recent survey of Arabs worldwide (n = 818) found that 46% of the sample had elevated levels of psychological distress, but only 8% of these people reported seeking treatment from a mental health professional (Kayrouz et al., unpublished). Barriers to treatment for Arab people appear to be similar to those experienced by people living in Western countries, and include low mental health literacy, lack of time and the shame associated with seeking mental health treatment (Gearing et al., 2012, Kayrouz et al., 2014, Kayrouz et al., 2015a).
One strategy that may improve access to mental health services for Arab people is to deliver psychological treatments, such as cognitive behavioural therapy (CBT), via the internet. Internet-delivered cognitive behavioural therapy (iCBT) interventions typically provide the same therapeutic content as provided in conventional face-to-face psychotherapy, but modified for online delivery (Andersson and Titov, 2014). Such treatments are typically highly structured, aim to impart practical skills, and can be delivered with or without therapist-guidance; but with some important exceptions (Berger et al., 2011a, Berger et al., 2011b, Dear et al., 2015a, Dear et al., 2015b, Dear et al., 2015c, Titov et al., 2013, Titov et al., 2015), results are typically stronger with therapist support (Titov, Dear & Andersson, 2014). While the use of such interventions has considerable meta-analytic support in predominantly Western samples (e.g., Andersson et al., 2014, Andrews et al., 2010, van Ballegooijen et al., 2014), there is emerging evidence to indicate their potential in Arab populations. For example, several small but promising trials have recently demonstrated that Arab people can benefit from iCBT interventions (Kayrouz et al., 2015, Knaevelsrud et al., 2015, Wagner et al., 2012). Among these, Knaevelsrud et al. (2015) provided therapist-guided online treatment for Iraqis (n = 47) with Post-Traumatic Stress Disorder (PTSD) and reported that 62% of those in a treatment group had recovered from post-traumatic stress symptoms at post-treatment, and that gains were maintained at three month follow up. More recently, Kayrouz et al. (2015) examined the feasibility of therapist-guided iCBT for Australian Arabs (n = 11) with anxiety and depression using a treatment course called the Arabic Wellbeing Course, which was presented in the English language. Significant reductions in symptoms of anxiety, depression and disability at post-treatment and three month follow up, with more than 90% reporting they would recommend the Course to a family member or friend.
The potential utility of iCBT for Arab populations is also consistent with clinical observations of therapists who have reported that Arabs prefer short-term and directive psychological treatments that have a focus on practical skills and the here-and-now, and that do not require them to divulge their story (Abudabbeh and Hays, 2006, Al-Krenawi and Graham, 2000, Chaleby, 1992). Consistent with this, the aforementioned international survey (n = 818) of Arabs (Kayrouz et al., unpublished) found that 82% of respondents reported they would be willing to try internet-delivered treatment if they experienced symptoms of anxiety and depression. Thus, internet-delivered treatment may be an acceptable option to address barriers and reduce psychological distress for Arabs worldwide.
The present study aims to extend this small but promising literature by exploring the feasibility and efficacy of a self-guided version of the Arabic Wellbeing Course, to treat symptoms of anxiety and depression among Arabs worldwide. To date, the published trials of internet-delivered treatments with Arab people have reported results of therapist-guided treatments. Self-guided treatments, if effective, have considerably more potential as a public health intervention, by virtue of lower delivery cost and increased anonymity. Because of the absence of previous studies of self-guided treatments for Arab people, a single group design was used in order to examine the acceptability of the self-guided internet-delivered treatment and inform the power requirements of a large randomised controlled trial.
2. Method
2.1. Design and hypotheses
A single-group open trial design was utilised to examine the feasibility, acceptability and preliminary efficacy of the self-guided and culturally modified iCBT Arabic Wellbeing Course for Arab consumers worldwide. A sample size of 15 was determined as sufficient (one-tailed test, power at 80%, and alpha at .05) to detect within-group Cohen's d effect size of .70; the minimum likely effect based on previous studies employing the Wellbeing Course (Kayrouz et al., 2015, Titov et al., 2013, Titov et al., 2014b). This study was approved by the Human Research Ethics Committee of Macquarie University, Sydney, Australia, and registered as a clinical trial with the Australian New Zealand Clinical Trials Registry, ACTRN12614000124639.
Based on the results of the previous therapist-guided trial of the Arabic Wellbeing Course (Kayrouz et al., 2015) it was hypothesised that: (1) Arabs would show a statistically and clinically significant reduction in the symptoms of depression, anxiety, distress and disability; and (2) Arabs would rate the course as worthwhile and would recommend the course to a friend or family member.
2.2. Participants
Details about the study were promoted via various traditional and Facebook (FB) recruitment strategies. Traditional strategies included the following: (1) media release by the University media and communications department; (2) emails to relevant Arab organisations (medical, secular and religious), health professionals and interested individuals; (3) newspaper advertisements in English and in a Lebanese and Australian Arabic newspaper; and (4) advertisements in English in religious organisations' newsletters. As traditional strategies yielded very few participants, FB promotion strategies were used. These included (1) promoting posts; (2) promoting FB public page (i.e., ECC Arabic Wellbeing); (3) promoting website (www.ecentreclinic.org) and (4) promoting events (for more details see Kayrouz et al., submitted). Interested adults applied online through a clinical research website (www.ecentreclinic.org), which provides information about anxiety and depression, and conducts clinical research concerning internet-delivered treatment. Because of the slower than expected recruitment, participants were recruited over a 12-month period from 10 February 2014 to 2 March 2015.
Eighty-one people initially provided informed consent and volunteered to participate. Inclusion criteria were: (1) person who self-identified as being of Arabic ancestry; (2) between the ages of 18 and 70; (3) having reliable internet access; (4) a Patient Health Questionnaire 9-item (PHQ-9) score ≥ 5 or a Generalised Anxiety Disorder 7-item (GAD-7) score ≥ 5 indicating at least mild depressive or anxiety symptoms, but not currently experiencing very severe depression (defined as a total score ≥ 23 or a score > 2 on question 9 of the PHQ-9) (Kroenke et al., 2001); and (5) if taking medication for anxiety or depression, having been on a stable dose for at least one month.
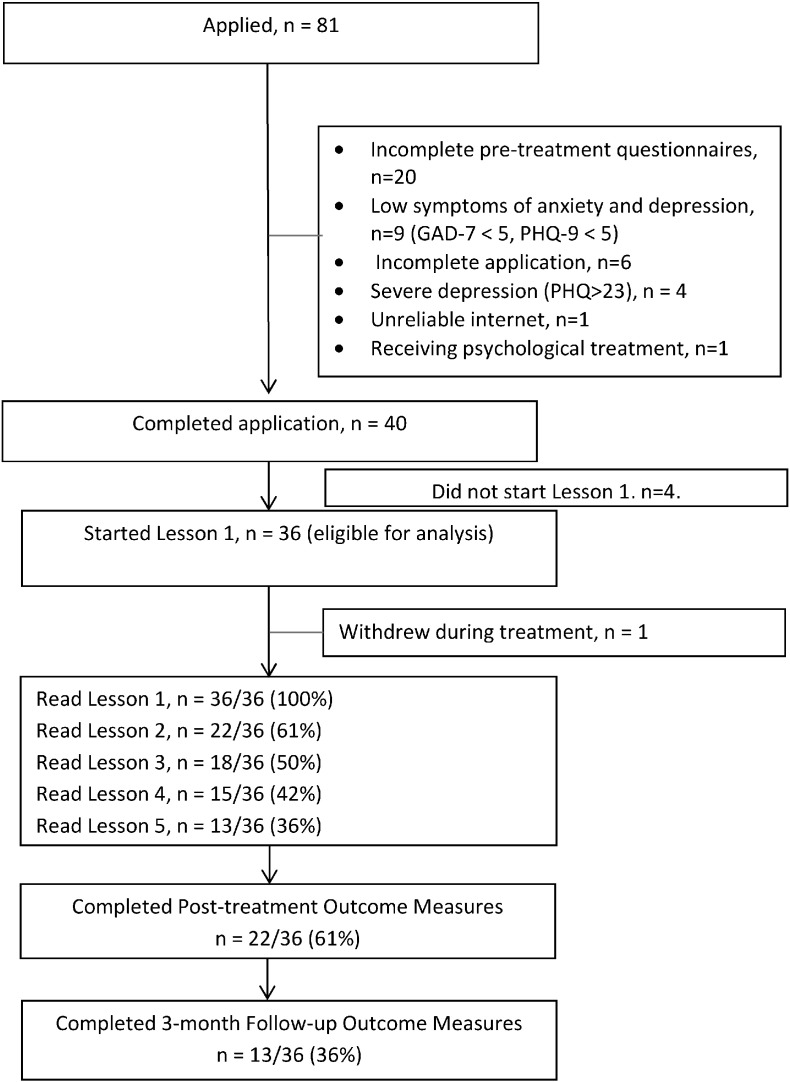
Of the 81 applicants, 45 were excluded (see Fig. 1) for the following reasons: (a) 6 for incomplete applications; (b) 9 for low symptoms of anxiety and depression (i.e., PHQ-9 and GAD-7 < 5); (c) 4 participants for very severe depression (i.e., defined as a total score ≥ 23 on the PHQ-9 or PHQ-9 Q9 > 2); (d) one for unreliable internet access; (e) one for seeing a psychologist face-to-face for CBT treatment; (f) 20 for non-completion of the pre-treatment questionnaires; and (g) 4 for not starting the course.
Fig. 1.
Participant flow.
The final sample of 36 participants had a mean age of 36.23 years (SD = 12.14; range = 19–67) and 58% (21/36) were females. The majority of participants were married (53%, n = 19), with the remainder single (30%, n = 11) or separated/divorced/other (17%, n = 6). Sixty-four per-cent of the sample (n = 23) had attained at least a bachelor's degree, 22% (n = 8) attained a trade certificate/apprentice or completed at least up to Yr10, and 14% (n = 5) attained a diploma. Sixty-one percent of the participants (22/36) reported they were in full-time or part-time employment, 17% (6/36) were full-time or part-time students, 17% (6/36) unemployed, 2.5% (1/36) reported not being able to work because of disability and 2.5% (1/36) was retired. Fifty-three percent participants (19/36) reported residing in Australia, 17% (6/36) residing in Lebanon, 8% (3/36) residing in Egypt, 8% (3/36) residing in Saudi Arabia, 5.5% (2/36) in the UK, 5.5% (2/36) in the USA and 3% (1/36) in Algeria. Forty-four per cent of the sample (16/36) reported having had previous mental health treatment and 25% (9/36) reported taking medication related to their symptoms.
2.3. Questionnaire measures
2.3.1. Primary measures
2.3.1.1. Patient Health Questionnaire – 9-item (PHQ-9; Kroenke et al., 2001)
The PHQ-9 is a nine-item measure of the symptoms and severity of depression. It has a clinical cut-off score of 10 that is predictive of a DSM-IV diagnosis of depression, with higher PHQ-9 scores indicating greater symptom severity. Internal consistency of the questionnaire is high (α = .74–.89) (Kroenke et al., 2001), and the questionnaire has good clinical sensitivity to change (Titov et al., 2011). Cronbach's alpha in the present study was acceptable (α = .73).
2.3.1.2. Generalised Anxiety Disorder — 7-item scale (GAD-7; Spitzer et al., 2006)
The GAD-7 is a brief seven-item screening questionnaire that has been found to be sensitive to generalised anxiety disorder, social phobia and panic disorder, with higher scores indicating greater symptom severity (Lowe et al., 2008). The GAD-7 scale has good internal consistency (α = .79–.91) and has good convergent and divergent validity with other anxiety and disability scales (Dear et al., 2011, Kroenke et al., 2010). A clinical cut-off score of 8 is indicative of a diagnosis of a DSM-IV anxiety disorder (Dear et al., 2011, Lowe et al., 2008, Richards and Suckling, 2009). In the present study, Cronbach's α = .71.
2.3.2. Secondary measures
2.3.2.1. Kessler 10-item scale (K-10; Kessler et al., 2002)
The K-10 is a ten-item measure of general psychological distress with total scores ≥ 22 associated with a diagnosis of anxiety and depressive disorders (Andrews and Slade, 2001). In the present sample, Cronbach's alpha was high (α = .83).
2.3.2.2. Sheehan Disability Scales (SDS; Sheehan, 1983)
The SDS is a three-item scale measuring functional impairment in the following domains: (1) work and studies, (2) social life, and (3) family life and home responsibilities. The SDS has been found to have high internal consistency of .89 (Leon et al., 1997). In the present study, Cronbach's α = .67.
Participants were administered all primary and secondary questionnaires at pre-treatment, post-treatment and at 3 month follow-up. The PHQ-9 and GAD-7 were also administered weekly to monitor safety and progress of each participant.
2.3.3. Additional measures
At post-treatment acceptability of the course was assessed by asking two questions. Questions required a ‘Yes’ or ‘No’ response. The questions were: (1) Would you recommend this Course to a friend or family member also experiencing stress or low mood?; and (2) Was it worth your time doing this Course?
2.4. Intervention
The Wellbeing Course is a five-lesson iCBT intervention targeting symptoms of both anxiety and depression, that is, a transdiagnostic intervention (Titov et al., 2013, Titov et al., 2014b). The Wellbeing Course is based on the Macquarie University Model (MUM) of internet-delivered psychological treatment (Titov et al., 2015). The Wellbeing Course is a structured skills-based course that focuses on teaching practical evidence-based psychological skills (e.g., realistic thinking, assertiveness, behavioural activation and graded exposure) that assist in the management of symptoms of anxiety and depression, consistent with the aforementioned Arab preferences for psychological treatment (Abudabbeh and Hays, 2006, Al-Krenawi and Graham, 2000, Chaleby, 1992). This course has been evaluated in several clinical trials (Kirkpatrick et al., 2013, Titov et al., 2013) with individuals of many different cultural backgrounds, including Arab Australians, and has been used in a national online public mental health service to treat more than 1000 Australian adults (Titov et al., 2015).
In addition to the five lessons, the Wellbeing Course comprises: (a) a summary of each lesson with homework to apply the skills taught in that lesson, (b) automated emails that encourage adherence and reinforce progress, (c) additional online resources about skills not described in the lessons, including communication, assertiveness, and sleep-hygiene skills and (d) stories about people who have recovered from anxiety and depression.
The Arabic Wellbeing Course was written in English and retained the core therapeutic components of the Wellbeing Course, maintaining the use of key concepts and descriptions of skills. However, modifications were made to make the course more culturally appropriate. Some of the key modifications included the following: (a) key words were transliterated into Arabic from English (e.g., not shameful (la khajela, mukhjil) and symptoms (3arada)); (b) case examples and educational stories were made more relevant to the target population by changing images, names and demographic characteristics of case examples, and edited to reflect common experiences for Arabs; and (c) the development of a religion and wellbeing resource that included information about cognitive restructuring of unhelpful religious thoughts, and religious practises (e.g., prayer, acts of service and charity) to reduce psychological symptoms (for detailed consideration of the structure, content and modifications refer to Kayrouz et al. (2015)).
Participants completed the course without direct contact or clinical support. However, all participants across the seven phases received automated weekly emails. These emails aimed to reinforce progress, summarise key skills of the course, normalise commonly experienced difficulties during treatment and encourage continued engagement.
2.5. Statistical methods
All analyses were performed in SPSS version 22.0 (SPSS, Inc., Chicago, IL). A generalised estimation equation (GEE) modelling technique was employed to examine changes in the symptom measures over time. GEE emphasises the modelling of change in an average group effect over time while accounting for within-subject variance with the specification of a working correlation structure (Hubbard et al., 2010). An unstructured working correlation structure was selected, coupled with a robust error estimation, for all GEE analyses. GEE analyses therefore provide model coefficients that represent multiplicative change in the dependent variable and these coefficients form a change factor (i.e., exp.(β)), which can be used to calculate the average percentage change from baseline to any time point. All GEE models also specified a gamma distribution with a log link response scale to address positive skewness, identified in each of the dependent variable distributions. Separate GEE models, utilising time effects and pre-treatment severity, were employed to impute missing data in the dependant variables consistent with intention-to-treat principles. In order to present the results transparently, these means from these GEE analyses (i.e., Estimated Marginal Means) are presented alongside data based on completers-only (i.e., Observed Means) and last-observation-carried-forward (i.e., LOCF Means) approaches to missing data.
The preliminary efficacy of the intervention was analysed for each dependent variable, one at a time. In each GEE analysis, change was calculated from pre-treatment to post-treatment and 3-month follow-up. SPSS pairwise comparisons were used to contrast the marginal means for the different time points (e.g. post to three month follow-up).
Several different statistics were calculated for comparison and benchmarking purposes. First, the average percentage change across time was calculated from the GEE analyses for each of the outcome variables with 95% confidence intervals. Second, Cohen's d effect sizes and 95% confidence intervals were also calculated for the within-groups effects based on the estimated marginal means derived from the GEE models. Third, based on dissemination studies (Richards and Suckling, 2009), an index of clinical significant remission and deterioration was calculated. The remission index was defined as the proportion of participants who at pre-treatment scored at or above the clinical cut-offs on the PHQ-9 (≥ 10) and GAD-7 (≥ 8), and subsequently decreased to a score that was below these clinical cut-offs at post-treatment and/or three-month follow-up (Richards and Suckling, 2009). Deterioration was defined as an increase by five or more points on the PHQ-9 or GAD-7 at post-treatment or follow-up, compared to pre-treatment (Richards and Suckling, 2009). Importantly, in these analyses, the last available data (i.e., last observation-carried-forward; LOCF) was carried forward for participants who did not complete post-treatment or three-month follow-up questionnaires to provide a conservative estimate of effect sizes and remission.
3. Results
3.1. Adherence and attrition
Thirty-six percent (13/36) of the participants completed the Course, which was defined as reading all five lessons within the eight-week period, however, 42% (15/36) read the first four lessons, which provides a proxy of minimum therapeutic dose. Sixty-one percent (22/36) and 36% (13/36) of the participants provided post-treatment and three-month follow-up data, respectively. Fig. 1 shows participant flow including adherence and attrition rates.
3.2. Outcomes and effect sizes
The outcomes and effect sizes of the trial are displayed in Table 1. The GEE analyses revealed significant main effects for Time on all measures: PHQ-9 (Wald's χ2(2, N = 36) = 82.71, p < .001), GAD-7 (Wald's χ2(2, N = 36) = 58.46, p < .001); SDS (Wald's χ2(2, N = 36) = 53.77, p < .001); and K-10 (Wald's χ2(2, N = 36) = 55.11, p < .001). Pairwise comparisons revealed that PHQ-9, GAD-7, SDS and K-10 scores were significantly lower at post-treatment and 3-month follow-up than at pre-treatment (all p < .001). There were significant differences on PHQ-9 (p = .004), SDS (p < .001), and K10 (p = .006) between post-treatment and 3-month follow-up.
Table 1.
Observed and estimated means, standard deviations, confidence intervals effect sizes (Cohen's d) and percentage change for the overall sample.
| Observed means |
Estimated marginal means |
LOCF means |
Cohen's d effect sizes a |
Percentage change from baseline b |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Follow-up | Pre | Post | Follow-up | Pre | Post | Follow-up | Pre to post | Post to follow-up | Pre to post | Pre to follow-up | |
| Primary measures | |||||||||||||
| Depression (PHQ-9) | 12.08 (4.87) | 6.54 (5.91) | 4.08 (4.54) | 12.08 (4.80) | 6.49 (4.51) | 4.37 (2.62) | 12.08 (4.87) | 8.39 (5.91) | 7.72 (5.64) | 1.20 (.69–1.69) | .57 (.10–1.04) | 46.3 (32.6–57.2) | 63.8 (56.0–70.3) |
| Anxiety (GAD-7) | 10.44 (4.01) | 5.77 (5.59) | 3.77 (5.02) | 10.44 (3.96) | 5.72 (4.27) | 4.58 (2.96) | 10.44 (4.01) | 7.61 (5.54) | 7.31 (5.54) | 1.15 (.64–1.63) | .31 (−.16–0.77) | 45.3 (30.2–57.1) | 56.2 (45.9–64.5) |
| Secondary measures | |||||||||||||
| Disability (SDS) | 22.50 (9.89) | 14.77 (13.10) | 9.08 (13.51) | 22.50 (9.75) | 14.54 (10.01) | 8.99 (7.80) | 22.50 (9.89) | – | – | 0.81 (.32–1.28) | .62 (.14–1.08) | 35.4 (19.1–48.4) | 60.0 (46.9–69.9) |
| Distress (K10) | 28.06 (6.96) | 21.13 (10.85) | 17.23 (9.09) | 28.06 (6.86) | 21.11 (8.29) | 17.88 (5.27) | 28.06 (6.96) | – | – | 0.91 (.42–1.39) | .47 (−.01–.93) | 24.8 (14.5–33.8) | 36.3 (29.8–42.1) |
Note. Standard deviations and 95% confidence intervals are shown in parentheses. Pre: Pre-treatment, Post: Post-treatment; Follow-up: 3 month follow-up; PHQ-9: Patient Health Questionnaire 9-Item; GAD-7: Generalised Anxiety Disorder 7-Item.; SDS: Sheehan Disability Scale; K10: Kessler 10-item; LOCF: Last Observation Carried Forward. No LOCF for secondary measures as no mid-treatment data was collected.
The effect sizes from baseline statistics are based on estimated marginal means derived from the GEE models.
The percentage change from baseline statistics are estimates of relative change derived from the GEE models conducted separately for each outcome.
Moderate-to-large pre-treatment to post-treatment effect size improvements were observed on the primary outcomes of anxiety and depression (Cohen's ds: Observed means ≥ 0.96; LOCF means ≥ 0.59; Estimated marginal means ≥ 1.15), which were maintained at 3-month follow-up. The effect sizes based on the estimated marginal means corresponded to average reductions in symptoms ≥ 45.3% at post-treatment and 3-month follow-up. Moderate-to-large pre-treatment to post-treatment effect size improvements were observed on the secondary outcomes of disability and general psychological distress (Cohen's ds: Observed means ≥.53; Estimated marginal means ≥ 0.81). LOCF means were not available for secondary outcomes as no mid-treatment data were collected. The effect sizes based on the estimated marginal means corresponded to reductions ≥ 24.8% at post-treatment and 3-month follow-up.
3.3. Clinical significance
Table 2 displays the clinically significant remission and recovery rates on the PHQ-9 and GAD-7. For the PHQ-9, of the 24/36 (66.67%) participants who scored above the cutoff at pre-treatment, eleven (11/24; 45.83%) were below this cutoff at post-treatment and 3-month follow-up. Fifteen of 36 (41.67%) participants made a 50% or greater improvement on the PHQ-9 at 3-month follow-up. For the GAD-7, of the 23/36 (63.90%) participants who scored above the cutoff at pre-treatment, 10/23 (43.48%) were below this cutoff at post-treatment and 3-month follow-up. Thirty-six percent of participants (13/36) made a 50% or greater improvement on the GAD-7 at post-treatment and 3-month follow-up.
Table 2.
Proportion of participants below cut-off scores of clinical significance (remission) and proportion demonstrating at least 50% reduction in pre-treatment scores (recovery) and the average improvement of the group.
| Pre-treatment |
Post-treatment |
3-month follow-up |
|||||
|---|---|---|---|---|---|---|---|
| ≥ Clinical cut-off | ≤ Clinical cut-off | ≥ 50% improvement | Average improvement | ≤ Clinical cut-off | ≥ 50% improvement | Average improvement | |
| PHQ-9 | 24/36 (66.67%) | 11/24 (45.83%) | 11/36 (30.55%) | 27.05% | 11/24 (45.83%) | 15/36 (41.67%) | 34.09% |
| GAD-7 | 23/36 (63.90%) | 10/23 (43.48%) | 13/36 (36.11%) | 27.24% | 10/23 (43.48%) | 13/36 (36.11%) | 31.42% |
Note. Intention-to-treat model was employed with last-observation being carried forward if follow-up data was not available. The clinical cut-off utilised for the PHQ-9 and GAD-7 was 10 and 8 respectively.
3.4. Deterioration
At post-treatment and 3-month follow-up, one (2.8%) and two (5.6%) of the 36 participants obtained PHQ-9 and GAD-7 scores five or more points higher compared to pre-treatment, respectively, indicating deterioration.
3.5. Acceptability
Twenty-one of 36 respondents (58.33%) provided data to assess the acceptability of the course. Ninety-one percent (19/21) of the responding participants reported it was ‘worth their time doing the course’, and 91% (19/21) reported that they would ‘recommend this course to a friend or family member with anxiety or depression’.
3.6. Contact
During treatment email contact was provided to six participants to assist with technical difficulties during the course. Additional email contact was provided to six participants to assess and manage mental health crises.
4. Discussion
The primary aims of the present study were to examine the preliminary efficacy and acceptability of the self-guided format of the Arabic Wellbeing Course, a culturally modified transdiagnostic iCBT programme, for symptoms of anxiety and depression in Arabs worldwide. It was hypothesised that participants would show statistically and clinically significant reduction in symptoms of depression, anxiety, distress and disability, and that they would rate the course as worthwhile and recommend the programme to a friend or family member. These hypotheses were supported.
Overall, the results from this small, preliminary trial are encouraging. Large within-group effect sizes were found on the primary and secondary outcome measures including a measure of disability, indicating that improvements generalised to other domains. The available data indicated that these improvements were maintained at follow-up and were reflected in moderate levels of remission and recovery. These results are consistent with the results of a previous small open trial of the Arabic Wellbeing Course with Arab Australians (Kayrouz et al., 2015), and with results observed in an evaluation of the Wellbeing Course used in a self-guided format with a general Australian population (Titov et al., 2013, Titov et al., 2014b). In addition, high rates of participant satisfaction were observed in the present trial, highlighting the potential time and cost-effectiveness of self-guided iCBT to Arab people.
These results are also consistent with the positive results from a small but encouraging body of work that has evaluated modified versions of iCBT interventions developed for Western populations with other cultural groups (Choi et al., 2012, Kayrouz et al., 2015, Knaevelsrud et al., 2015, Wagner et al., 2012). This literature provides further support for the position that people of different cultures share similar experiences of anxiety and depression, and may therefore benefit from similar treatment strategies. Notwithstanding the limitations of an open trial design, the present study extends these results by demonstrating that relatively minor modifications can be sufficient to make interventions acceptable to a targeted culturally and linguistically diverse (CALD) group. Importantly, since modified interventions have shown preliminary effectiveness in self-guided formats (Titov et al., 2013, Titov et al., 2014b, Titov et al., 2012), the potential for improving access to psychological treatments for CALD communities is considerable.
Notwithstanding this potential, the language barrier of the Arabic Wellbeing course being available in English only, may explain the low level of interest and difficulties in recruiting Arabs to the current study. Language has been found to be a barrier to accessing western psychological treatments among Arab populations (Gearing et al., 2012). Thus, providing an intervention in a language that is congruent and sensitive to the values and meanings of the participant culture (Bernal et al., 1995, Bernal et al., 2009) is critical in reducing barriers and possibly increasing interest in and recruitment for future trials. Recently, the research team has completed a rigorous Arabic translation of the Arabic Wellbeing Course and is currently conducting a trial to examine the preliminary efficacy and acceptability of the Arabic translation.
Limitations of this study include the following: first, the absence of a control group means it is not possible to determine effect of the treatment beyond that of spontaneous remission. Second, the small sample size limits the extent to which the results can be generalised and means that significant caution is needed in interpreting the results of the trial beyond conclusions about the general feasibility of iCBT for Arabs. Third, the relatively high educational level of the sample limits the extent to which the results can be generalised to those with lower levels of educational attainment. Fourth, the level of acculturation was not measured, raising questions about the extent to which acculturation may moderate treatment outcomes. However, a large randomised controlled trial is planned, which will address several of these issues. A fifth limitation is the low questionnaire completion rates at post-treatment and follow-up, which reflect the low completion rates of the entire five lessons of the course. In order to present the results transparently, completer, last-observation-carried-forward, and results based on estimates using GEE modelling were reported. However, these limited completion rates provide further indications that caution should be taken in generalising the results of this study.
In summary, the self-guided format of the Arabic Wellbeing Course resulted in large improvements on measures of anxiety, depression, stress and disability at post-treatment, which were sustained at three-month follow up. Moreover, the treatment was rated as acceptable to participants. Notwithstanding the low treatment completion and questionnaire completion rates, these results provide further evidence that this intervention has potential as a treatment tool for Arabs worldwide with symptoms of anxiety and depression.
Funding
The funding for the study was provided by Macquarie University as part of the lead author's PhD candidature. BFD is supported by a National Health and Medical Research Council Australian Public Health Fellowship. MG is supported by a Macquarie University Research Fellowship. The development of the Wellbeing Course was enabled by funding from the Australian National Health and Medical Research Council Project Grant No. 630,560.
Declaration of conflicting interests
The Authors declare that there is no conflict of interest.
Acknowledgements
The Authors wish to acknowledge all participants, service providers, Arabic speaking organisations and other agencies that supported this study.
References
- Abudabbeh N., Hays P.A. Cognitive behavioral therapy with people of Arab heritage. In: Hays P.A., Iwamasa G.Y., editors. Culturally Responsive Cognitive-Behavioral Therapy: Assessment, Practice, And Supervision. American Psychological Assocaition; Washington, DC: 2006. pp. 141–159. [Google Scholar]
- Alhasnawi S., Sadik S., Rasheed M., Baban A., Al-Alak M.M., Othman A.Y.…Kessler R.C. The prevalence and correlates of DSM-IV disorders in the Iraq Mental Health Survey (IMHS) World Psychiatry. 2009;8(2):97–109. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2694515/ Retrieved from. [PMC free article] [PubMed] [Google Scholar]
- Al-Krenawi A., Graham J.R. Culturally sensitive social work practice with Arab clients in mental health settings. Health Soc. Work. 2000;25(1):9–22. doi: 10.1093/hsw/25.1.9. [DOI] [PubMed] [Google Scholar]
- Andersson G., Titov N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry. 2014;13(1):4–11. doi: 10.1002/wps.20083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G., Cuijpers P., Carlbring P., Riper H., Hedman E. Guided Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry. 2014;13(3):288–295. doi: 10.1002/wps.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G., Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10) Australian and New Zealand Journal of Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842x.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- Andrews G., Cuijpers P., Craske M.G., McEvoy P., Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One. 2010;5(10) doi: 10.1371/journal.pone.0013196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger T., Caspar F., Richardson R., Kneubuhler B., Sutter D., Andersson G. Internet-based treatment of social phobia: a randomized controlled trial comparing unguided with two types of guided self-help. Behav. Res. Ther. 2011;49(3):158–169. doi: 10.1016/j.brat.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Berger T., Hämmerli K., Gubser N., Andersson G., Caspar F. Internet-based treatment of depression: a randomized controlled trial comparing guided with unguided Self-Help. Cogn. Behav. Ther. 2011;40(4):251–266. doi: 10.1080/16506073.2011.616531. [DOI] [PubMed] [Google Scholar]
- Bernal G., Bonilla J., Bellido C. Ecological validity and cultural sensitivity for outcome research: issues for the cultural adaptation and development of psychosocial treatments with Hispanics. J. Abnorm. Child Psychol. 1995;23(1):67–82. doi: 10.1007/BF01447045. [DOI] [PubMed] [Google Scholar]
- Bernal G., Jimenez-Chafey M.I., Domenech Rodriguez M.M. Cultural adaptation of treatments: a resource for considering culture in evidence-based practice. Professional Psychology - Research & Practice. 2009;40(4):361–368. [Google Scholar]
- Chaleby K. Psychotherapy with Arab patients, toward a culturally oriented technique. Arab Journal of Psychiatry. 1992;3(1):16–27. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=psyc3&AN=2001-16515-003 Retrieved from. [Google Scholar]
- Choi I., Zou J., Titov N., Dear B.F., Li S., Johnston L.…Hunt C. Culturally attuned Internet treatment for depression amongst Chinese Australians: a randomised controlled trial. J. Affect. Disord. 2012;136(3):459–468. doi: 10.1016/j.jad.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Titov N., Sunderland M., McMillan D., Anderson T., Lorian C., Robinson E. Psychometric comparison of the Generalized Anxiety Disorder Scale-7 and the Penn State Worry Questionnaire for measuring response during treatment of Generalised Anxiety Disorder. Cogn. Behav. Ther. 2011;40(3):216–227. doi: 10.1080/16506073.2011.582138. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Gandy M., Karin E., Staples L.G., Johnston L., Fogliati V.J.…Titov N. The Pain Course: a randomised controlled trial examining an internet-delivered pain management program when provided with different levels of clinician support. Pain. 2015;156(10):1920–1935. doi: 10.1097/j.pain.0000000000000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dear B.F., Staples L.G., Terides M.D., Karin E., Zou J., Johnston L.…Titov N. Transdiagnostic versus disorder-specific and clinician-guided versus self-guided treatment for Generalised Anxiety Disorder: a randomised controlled trial. J. Anxiety Disord. 2015 doi: 10.1016/j.janxdis.2015.09.003. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Zou J.B., Ali S., Lorian C.N., Johnston L., Terides M.D.…Titov N. Examining self-guided internet-delivered cognitive behavior therapy for older adults with symptoms of anxiety and depression: two feasibility open trials. Internet Interventions. 2015;2(1):17–23. [Google Scholar]
- Gearing R.E., Schwalbe C.S., MacKenzie M.J., Brewer K.B., Ibrahim R.W., Olimat H.S.…Al-Krenawi A. Adaptation and translation of mental health interventions in Middle Eastern Arab countries: a systematic review of barriers to and strategies for effective treatment implementation. Int. J. Soc. Psychiatry. 2012;59(7):671–681. doi: 10.1177/0020764012452349. [DOI] [PubMed] [Google Scholar]
- Ghanem M., Gadallah M., Meky F.A., Mourad S., El-Kholy G. National survey of prevalence of mental disorders in Egypt: preliminary survey. East Mediterr. Health J. 2009;15(1):65–75. http://simsrad.net.ocs.mq.edu.au/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=2010300342&site=ehost-live Retrieved from. [PubMed] [Google Scholar]
- Hubbard A.E., Ahern J., Fleischer N.L., Laan M.V.d., Lippman S.A., Jewell N.…Satariano W.A. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467–474. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- Kadri N., Agoub M., Assouab F., Tazi M.A., Didouh A., Stewart R., Moussaoui D. Moroccan national study on prevalence of mental disorders: a community-based epidemiological study. Acta Psychiatr. Scand. 2010;121(1):71–74. doi: 10.1111/j.1600-0447.2009.01431.x. [DOI] [PubMed] [Google Scholar]
- Karam E.G., Mneimneh Z.N., Karam A.N., Fayyad J.A., Nasser S.C., Chatterji S., Kessler R.C. Prevalence and treatment of mental disorders in Lebanon: a national epidemiological survey. Lancet. 2006;367(9515):1000–1006. doi: 10.1016/S0140-6736(06)68427-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayrouz R., Dear B.F., Johnston L., Keyrouz L., Nehme E., Laube R., Titov N. Intergenerational and cross-cultural differences in emotional wellbeing, mental health service utilisation, treatment seeking preferences and acceptability of psychological treatments for Arab Australians. Int. J. Soc. Psychiatry. 2014 doi: 10.1177/0020764014553004. [DOI] [PubMed] [Google Scholar]
- Kayrouz, R., Dear, B. F., Karin, E., Terides, M., Gandy, M., Fogliati, V., & Titov, N. (unpublished). Acceptability of mental health services for anxiety and depression amongst Arabs. International Journal of Social Psychiatry.
- Kayrouz R., Dear B.F., Titov N. 2016. Facebook as an effective recruitment strategy for mental health research of hard to reach populations Internet Interventions. (submitted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayrouz R., Dear B.F., Johnston L., Gandy M., Fogliati V.J., Sheehan J., Titov N. A feasibility open trial of guided Internet-delivered cognitive behavioural therapy for anxiety and depression amongst Arab Australians. Internet Interventions. 2015;2(1):32–38. [Google Scholar]
- Kessler R.C., Aguilar-Gaxiola S., Alonso J., Chatterji S., Lee S., Ormel J.…Wang P.S. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) Surveys. Epidemiology and Psychiatric Sciences. 2009;18(01):23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.-L.T.…Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32(06):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick T., Dear B.F., Johnston L., Titov N. A feasibility open trial of an internet-delivered cognitive-behavioural therapy (iCBT) among consumers of a Non-Governmental Mental Health Organisation with anxiety. PeerJ. 2013;1 doi: 10.7717/peerj.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knaevelsrud C., Brand J., Lange A., Ruwaard J., Wagner B. Web-based psychotherapy for posttraumatic stress disorder in war-traumatized Arab patients: randomized controlled trial. J. Med. Internet Res. 2015;17(3) doi: 10.2196/jmir.3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Löwe B. The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen. Hosp. Psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Leon A.C., Olfson M., Portera L., Farber L., Sheehan D.V. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int. J. Psychiatry Med. 1997;27:93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- Lowe B., Decker O., Muller S., Brahler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the Generalized Anxiety Disorder screener (GAD-7) in the general population. Med. Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Richards D.A., Suckling R. Improving access to psychological therapies: phase IV prospective cohort study. Br. J. Clin. Psychol. 2009;48(4):377–396. doi: 10.1348/014466509X405178. [DOI] [PubMed] [Google Scholar]
- Sheehan D.V. Charles Scribner and Sons; New York: 1983. The Anxiety Disease. [Google Scholar]
- Slade T., Johnston A., Oakley Browne M.A., Andrews G., Whiteford H. 2007 National Survey of Mental Health and Wellbeing: methods and key findings. Aust. N. Z. J. Psychiatry. 2009;43(7):594–605. doi: 10.1080/00048670902970882. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Lowe B. A brief measure for assessing Generalized Anxiety Disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- The World Bank . 2014. Arab world.http://data.worldbank.org/region/ARB Retrieved from. [Google Scholar]
- Titov N., Dear B.F., Andersson G. Internet-delivered psychotherapy for anxiety disorders and depression. Focus. 2014;12(3):299–308. [Google Scholar]
- Titov N., Dear B.F., Johnston L., Lorian C., Zou J., Wootton B.…Rapee R.M. Improving adherence and clinical outcomes in self-guided internet treatment for anxiety and depression: randomised controlled trial. PLoS One. 2013;8(7) doi: 10.1371/journal.pone.0062873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Johnston L., McEvoy P., Wootton B., Terides M.…Rapee R. Improving adherence and clinical outcomes in self-guided internet treatment for anxiety and depression: a 12-month follow-up of a randomised controlled trial. PLoS One. 2014;9(2) doi: 10.1371/journal.pone.0089591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Johnston L., Terides M. Transdiagnostic internet treatment for anxiety and depression. Spanish Journal of Clinical Psychology. 2012;17(3):237–260. [Google Scholar]
- Titov N., Dear B.F., McMillan D., Anderson T., Zou J., Sunderland M. Psychometric comparison of the PHQ-9 and BDI-II for measuring response during treatment of depression. Cogn. Behav. Ther. 2011;40(2):126–136. doi: 10.1080/16506073.2010.550059. [DOI] [PubMed] [Google Scholar]
- Titov N., Dear B.F., Staples L.G., Bennett-Levy J., Klein B., Rapee R.M.…Nielssen O.B. MindSpot Clinic: an accessible, efficient, and effective online treatment service for anxiety and depression. Psychiatr. Serv. 2015;66(10):1043–1050. doi: 10.1176/appi.ps.201400477. [DOI] [PubMed] [Google Scholar]
- van Ballegooijen W., Cuijpers P., van Straten A., Karyotaki E., Andersson G., Smit J.H., Riper H. Adherence to internet-based and face-to-face cognitive behavioural therapy for depression: a Meta-analysis. PLoS One. 2014;9(7) doi: 10.1371/journal.pone.0100674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner B., Schulz W., Knaevelsrud C. Efficacy of an internet-based intervention for posttraumatic stress disorder in Iraq: a pilot study. Psychiatry Res. 2012;195(1–2):85–88. doi: 10.1016/j.psychres.2011.07.026. [DOI] [PubMed] [Google Scholar]