1. Background
1.1. Caregiver burden
Approximately 42.1 million family caregivers provided care to an adult with limitations in daily activities at any given point in time in the US in 2009 (Feinberg et al., 2011). The economic value of caregivers' unpaid contributions was estimated to $450 billion (Feinberg et al., 2011). Younger care recipients most often suffer from mental illness (MI)1 while older care recipients' problems are commonly aging, chronic diseases, Alzheimer's, dementia/other mental confusion (National Alliance for Caregiving and AARP, 2004). There are approximately 1.3 million caregivers in Sweden who support someone regularly, of whom 900,000 are of working age and 140,000 have stopped or reduced their working hours due to the caregiving situation (Riksförbund, 2016). Many of the families with a person with MI experience such psychological distress that they require therapeutic intervention. Caregivers of people with other diseases, e.g. stroke (Rigby et al., 2009), dementia (Etters et al., 2008), cancer (Grunfeld et al., 2004), Parkinson's (Schrag et al., 2006), and brain tumors (Schubart et al., 2008) also experience caregiver burden. This entails both an objective and subjective burden, the latter referring to the psychological distress prompted by the illness (Lefley, 1989). It hence includes psychological, occupational and financial burdens, especially in times of illness deterioration (Grunfeld et al., 2004; Schubart et al., 2008). The experience of burden has been found to be enhanced in long-lasting relationships, when the caregiver and his/her relative live together and when the care is given daily and not appreciated (Östman and Hansson, 2004). Caregivers of older adults also report decreases in health due to caregiving (National Alliance for Caregiving and AARP, 2009). For example, role overload (Turcotte, 2013; Adelman et al., 2014) and caregiver burden can be the most important predictors of anxiety/depression (Rigby et al., 2009) and negative stress in caregivers (Turcotte, 2013; Adelman et al., 2014). Furthermore, caregivers report unmet needs such as finding own time, managing emotional and physical stress, and balancing work and family responsibilities (Longacre, 2013).
It has been proposed that health professionals should include the management of caregiver distress to improve families' quality of life (QoL) (Schrag et al., 2006) and guide them towards effective interventions (Rigby et al., 2009; Adelman et al., 2014). Care duties, carers' fears and worries, and the patient's behavior (Cormac and Tihanyi, 2006) can have negative effects on caregivers' mental health (Schulz and Sherwood, 2008; Phillips et al., 2009; Smith et al., 2014). Family interventions can improve the family's emotional climate (Pharoah et al., 2010), with lower relapse rates, and enhanced outcomes and problem-solving capacities. Transportation issues, fatigue, lack of resources and stigma can be barriers to accessing help, which can be addressed by online solutions. Tailored online interventions that incorporate behavior change techniques such as stress management can have positive effects on caregivers' psychological well-being (Guay et al., 2017). Web-based mindfulness interventions (MBI)2 show promising results with beneficial health effects for healthy and clinical samples (de Vibe et al., 2012). A feasibility study and randomized controlled trial of the current online MBI showed positive significant results for families living with MI with enhanced levels of mindfulness and self-compassion, and decreased levels of caregiver burden and perceived stress (Stjernswärd and Hansson, 2016a; Stjernswärd and Hansson, 2017), combined with good usability and subjective value when using the program (Stjernswärd and Hansson, 2016b). Usability refers to the extent to which a specific user can use a specific product to reach specific goals, with purposefulness, effectiveness, and satisfaction, in a given context (ISO, 1998). Ease of access and flexibility of use were strong motivators for use (Stjernswärd and Hansson, 2016b). More studies are called for to verify the intervention's effectiveness for extended groups of caregivers.
1.2. Mindfulness interventions
Kabat-Zinn's Mindfulness-Based Stress Reduction (MBSR) program is a contemporary version of mindfulness stripped of its buddhistic aspects. He defines mindfulness as “the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment” (Kabat-Zinn, 2003). Moreover, mindfulness has been successfully incorporated into evidence-based clinical interventions, i.e. Mindfulness-Based Cognitive Therapy (Segal et al., 2002), Acceptance and Commitment Therapy (Hayes et al., 2006), and Dialectical Behavior Therapy (Linehan, 1993), with subsequent decreases of clinical symptoms, and improved mental health and well-being (Keng et al., 2011; de Vibe et al., 2012; Khoury et al., 2013).
MBI show beneficial effects on mental health outcomes in persons with somatic and mild/moderate psychological problems and for non-clinical samples (de Vibe et al., 2012). MBSR interventions show positive effects on personal development (empathy, coping), mindfulness, QoL and somatic health outcomes (de Vibe et al., 2012). The literature also shows positive psychological effects, improved behavioral regulation (Keng et al., 2011) and effectiveness in reducing caregiver stress as measured by psychological and biological markers (Bloom et al., 2012). MBI have shown to be useful in addressing caregivers' burden, stress (Epstein-Lubow et al., 2011; Pagnini et al., 2015) and mental health (Hou et al., 2014; Paller et al., 2014). The standard 8-week MBI with an instructor requires time for weekly group meetings, daily exercises and one day's silent meditation. However, reduced exercise time does not necessarily affect outcomes negatively (Boettcher et al., 2013), and has been associated with positive results and high program satisfaction. Studies show the feasibility and benefits of MBI online in clinical (Boettcher et al., 2013) and non-clinical (Glück and Maercker, 2011) samples, including reduction in stress (Glück and Maercker, 2011; Krusche et al., 2012), anxiety and depression (Boyer et al., 2012), and increased QoL (Boettcher et al., 2013); this is valid for face-to-face (f2f) and online MBI (Boettcher et al., 2013) despite the lack of contact with an instructor and fellow participants in the latter (Krusche et al., 2012).
The cultivation of self-compassion is more or less explicitly interwoven in mindfulness practices (Hölzel et al., 2011), for example, by encouraging a gentle and accepting attitude towards the self during meditations. It can contribute to acceptance and a caring and non-judgmental attitude towards the self and others (Kabat-Zinn, 2009), and to positive effects on psychological functioning (Hofmann et al., 2011). Self-compassion entails three components: self-kindness vs self-judgment, common humanity vs isolation, and mindfulness vs over-identification (Neff, 2003). The practice of mindfulness practice helps break automatic behavior through increased awareness and facilitates responding and coping instead of reacting to stressors, deterring stress reactivity (Kabat-Zinn, 2009), which may enhance families' coping ability and prevent exhaustion. Caregivers' QoL is strongly affected by physical and emotional distress due to unfulfilled needs and caregiving (Caqueo-Urízar et al., 2009). Restoration of patient functioning in family/social roles are good targets for interventions (Caqueo-Urízar et al., 2009), as are coping strategies and the development of personal strength to improve QoL (Boyer et al., 2012). As caregivers can experience an added burden and inter-relational stress, the potential reduction of emotional reactivity, and the enhancement of emotional regulation and positive emotions through MBI (Hofmann et al., 2011; Keng et al., 2011) may be valuable to get a sense of perspective on the situation and enable responding rather than reacting automatically to stressful situations. The cultivation of compassion meditation can further contribute to a more compassionate and caring attitude towards the self and others (Kabat-Zinn, 2009), potentially benefiting both caregivers and patients. Healthy relatives are also better equipped to help the patient, which is why interventions to support burdened caregivers may be valuable to help them cope. The study's aim was to assess the effectiveness and usability of a web-based MBI for families living with mental or somatic illness.
2. Ethical considerations
The project was approved by the Regional Ethical Committee, Lund, Sweden (dnr 2016/925). Informed consent was obtained from all individual participants included in the study.
3. Methods
3.1. Procedure
The current effectiveness study was designed as a randomized controlled trial with an experimental group and a wait-list control group (WLC), with measurements at baseline (T1), post intervention (T2) and at a 3-month follow-up (T3) on primary and secondary outcomes, and usability, in order to explore the effectiveness of the web-based mindfulness program in supporting caregivers to cope with their situation. The hypothesis was that participation in the program would lead to increased levels of mindfulness and self-compassion, and to decreased levels of caregiver burden and perceived stress in the participants. The WLC was offered the same program after termination of the experiment group's test period, although with a 12-week delay due to semester break. The CONSORT (2010) checklist guided the reporting of the current randomized trial. As the participants could discontinue participation without needing to motivate this, however, reasons for drop-out were not actively registered unless the participants actively informed about the termination of their participation and volunteered this information (as this was done inconsistently, these are not reported here).
3.2. Intervention
The intervention consists of a web-based mindfulness program tailored for families living with mental (MI) or somatic illness (SI), in the sense that its contents are related to caregivers' situation and associated experiences of burden and stress. The audio files for instance take up the fact that being close to an ill person can arouse stressful feelings and thoughts and affect significant others' daily lives. The training is introduced as a potential tool for coping with e.g. stress. The program can be accessed through a computer/tablet/smartphone with Internet access. It contains audio/video files (960 min), including introductory information (initial video and weekly introductions for every new step) and a concluding video (video files) and weekly training advice half-way through the weekly steps (audio files) accompanied by written keywords on the screen, audio files for the daily formal mediations (2 × 10 min/day), descriptive text files and instructions for daily informal mindfulness practice (e.g. notice sounds, scents, etc.), a time log (the training time was registered automatically and displayed on the program website), and a private diary (not visible to the researchers). The recommended training time was set to 2 × 10 min/day, 6 days/week for 8 consecutive weeks. Participants were also encouraged, through a note on the screen once the daily formal meditations were completed, to do daily informal practices (e.g. notice the breath or bodily sensations at some point during the day). The formal training includes basic mindfulness practices such as breathing exercises, body scans, mindful yoga/conscious movements, attention to experiences through the senses, and (self) compassion meditations (Table 1). The exercises are comparable to those in MBSR programs, except that they are kept to a maximum of 10 min/exercise to make them more easily practicable for participants with busy schedules. The test period was set to 10 weeks to allow for individual flexibility. Weekly e-mail reminders, including contact information to the researchers/technical support, were sent to the participants as reminders and motivators for training.
Table 1.
The program's 8 weekly steps.
| Week | Contents: every step (8 steps, 1 step/week) contains initial introductory audio-files and weekly advice (audio-files) half-way through the respective steps, besides general introductory and concluding video files (at start and finish), and written instructions for daily informal exercises for download. The daily meditation consist of 2 × 10 min audio files. |
|---|---|
| 1 | The breathing body |
| 2 | Being present in the body |
| 3 | Mindfulness in life and movement |
| 4 | Compassion with the self – acceptance |
| 5 | Wonderful pleasure |
| 6 | Being whole |
| 7 | Compassion with others |
| 8 | To live with the possibility of choosing |
3.3. Measures
Participants were sent a link by email for data collection online including a sociodemographic questionnaire (T1) and validated self-assessments scales online at baseline (T1), post intervention (T2), and at a 3-month follow-up (T3), and usability questionnaires (T2, T3).
Five Facet Mindfulness Questionnaire (FFMQ): it consists of 39 items, rated on a 5-points Likert scale (1 = never or very rarely true, 5 = very often or always true), assessing five facets of mindfulness: Non-reactivity to inner experience (7 items), Observing (8 items), Acting with Awareness (8 items), Describing (8 items), Non-judging of Experience (8 items). The scale has shown good internal consistency with alpha coefficients ranging from 0.75 to 0.91 (Baer et al., 2006; Baer et al., 2008). The Swedish version of the FFMQ has shown good psychometric properties, with results comparable to those obtained by Baer et al., 2006, Baer et al., 2008 (Lilja et al., 2011). Cronbach's alpha for FFMQ in the current study was 0.91.
Self-Compassion Scale-Short form (SCS-SF): this 12-item scale measures six components of self-compassion using six subscales with two items each: Self-Kindness, Self-Judgment, Common Humanity, Isolation, Mindfulness, and Over-Identification. Items are rated on a 5-point response scale (1 = almost never to 5 = almost always) (Raes et al., 2011). The scale has shown adequate internal consistency (Cronbach's alpha ≥0.86) and a near-perfect correlation with the long form SCS (r ≥ 0.97) (Raes et al., 2011). The Swedish version of the SCS was translated and back translated by Strömberg (unpublished manuscript) and approved by Neff, the scale's originator. It showed good reliability in a Swedish study (Wallmark et al., 2013). A short version was used, for which Cronbach's alpha in the current study was 0.84.
Perceived Stress Scale (PSS): it is a validated 14-item scale measuring the degree to which situations in life in the past month are appraised as unpredictable, uncontrollable and overwhelming, using a five-point response scale (0 = rarely to 4 = very often) (Cohen, 2013). The scale has shown good reliability and validity. The Swedish version has demonstrated good internal consistency (0.82) and split-half reliability (0.84), and adequate construct validity (Eskin and Parr, 1996). Cronbach's alpha for PSS in the current study was 0.78.
CarerQoL7-D: this self-rating instrument measures seven dimensions of caregiver burden using seven items with a 3-points response scale (1 = no problems to 3 = a lot of problems): fulfillment, relational dimension, mental health dimension, social dimension, financial dimension, perceived support, and physical dimension. It includes the CarerQoL-VAS, indicating the level of happiness with caregivers' experiences and encompassing both negative and positive aspects, ranging from 0 = “completely unhappy” to 10 = “completely happy” (Brouwer et al., 2006). The scale has shown good validity in measuring informal carer effects (Brouwer et al., 2006; Hoefman et al., 2011).
The Montgomery-Borgatta burden scale: this self-rating scale measures stress/subjective burden (affect component of burden), relationship burden (the extent to which caregivers perceive the care recipient's behavior as manipulative or overly demanding), objective burden (the extent to which care relationships impose on observable aspects of a caregiver's life, e.g. time for self/others), and uplifts. It includes 22 items with a response set ranging from 1 (a lot less) to 5 (a lot more) assessing to which level aspects of their life had changed because of caregiving (Montgomery et al., 2000). The four subscales' total scores are calculated, with higher scores indicating higher levels of burden or uplifts. The reliability of all forms of burden range from 0.83 to 0.89 (Savundranayagam and Montgomery, 2010). Cronbach's alpha in the current study was 0.82.
Usability, confounding factors and negative effects of training: A Swedish version of the System usability scale (SUS) (Brooke, 1996) was used to assess the program's usability. It is a 10-item 5-point Likert scale giving a global view of subjective assessments of usability. Possible scores range between 0 and 100 with higher scores indicating better usability. A system with a SUS value >70 can be estimated as good and > 85 as excellent, although it doesn't guarantee high acceptability in the field (Bangor et al., 2008). SUS has been used extensively, displaying good reliability and validity across a variety of assessed systems (Sauro, 2011). Additional questions with room for free-text answers about usability, confounding factors (other sources of support, negative life events, patient's health status) and negative effects of training were also included for separate analysis.
3.4. Participants
Participants were recruited (January–February 2017) through advertisement in papers, newsletters, online, social media, and clinics/organizations with interests in caregivers. On the question “where did you first hear about the project” respondents in the experiment and the WLC groups answered: newspaper advertisement (directly or through tips) (74%), Facebook-social media/advertisement on website (18%), tips from friend (5%), through care organization/family consultant (2%), and other/don't remember (1%). Information about the study and informed consent were available online. The inclusion criteria were: age (>18), being a relative/significant other to a person with MI or SI (mixed diagnoses/as reported by participants), having access to a computer/Internet, and understanding Swedish. The exclusion criteria were having prior experience of mindfulness meditation and an own severe MI that requires other professional treatment. A power calculation based on the primary outcome measure (mindfulness) from the previous feasibility study showed that 100 participants (50 per arm) would be an adequate sample size to identify a medium effect size using a 80% probability and p < 0.05 as a marker of significant differences. We intended to include 140 persons, accounting for a drop-out rate of around 30%.
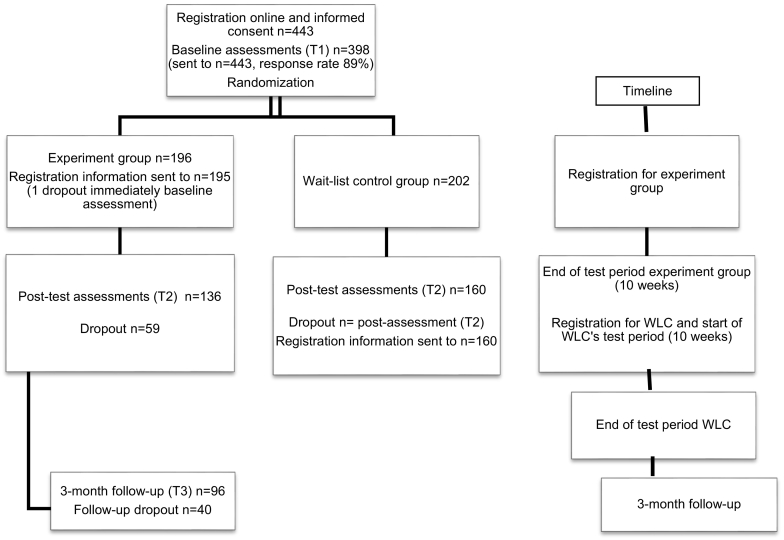
Of the 443 participants who fulfilled the inclusion criteria and were registered in the study using the online consent form, 398 completed the sociodemographic and baseline questionnaires (T1), after which all participants were randomized (allocation sequence generated by the first author through randomizer.org) into an experiment group (n = 196) and a WLC (n = 202) (Fig. 1). As registration to the study implied that the inclusion criteria were met, none of the registered participants were excluded. After randomization, participants in the experiment group were sent an e-mail with instructions for registration to the web-based mindfulness program. Participants in the WLC were sent similar instructions once the post-test questionnaires following the first test period (T2) were completed, which also represented their baseline assessments prior to their own test period with the same program as the experiment group.
Fig. 1.
Total sample and dropout.
There were no significant sociodemographic differences between the groups. The majority of participants were women, aged 50–69 (mean = 52.5), and a parent to the patient (47% and 51% in the respective groups), but also partners (21%/23%), adult children (17%/12%), siblings (9%/7%) and persons with another relationship to the patient (4%/3%) were represented (Table 2). A majority of participants reported that they provided between 1 and 15 h of caregiving per week, including different kinds of support, with emotional followed by practical support being the most common. A majority of the participants helped with contacts with health care/other organizations, and about 40% provided financial support. The most commonly reported time since diagnosis was 1–5 years (37%/32%), followed by >15 years (28%/27%) in the respective groups. The majority of participants reported good physical health, while a more or less equal number of participants reported good or bad own mental health in both groups.
Table 2.
Background characteristics of the baseline sample (n = 398).
| Baseline n=398 |
Experiment group n=196 |
WLC n=202 |
||
|---|---|---|---|---|
| n | % | n | % | |
| Men/Women | 29/168 | 15/85 | 27/175 | 13/87 |
| Age | ||||
| 20-29 | 12 | 6 | 14 | 7 |
| 30-39 | 20 | 10 | 24 | 12 |
| 40-49 | 34 | 18 | 30 | 15 |
| 50-59 | 79 | 40 | 62 | 30 |
| 60-69 | 39 | 20 | 56 | 28 |
| >70 | 12 | 6 | 16 | 8 |
| Married or in a relationship/Single | 163/33 | 83/17 | 167/35 | 83/17 |
| Relationship to the patient | ||||
| Father/mother | 7/85 | 47 | 6/96 | 51 |
| Son/daughter | 13/21 | 17 | 7/17 | 12 |
| Brother/sister | 2/15 | 9 | 1/13 | 7 |
| Partner (male/female) | 23/19 | 21 | 27/20 | 23 |
| Other relationship | 7 | 4 | 7 | 3 |
| Non valid answers | 4 | 2 | 8 | 4 |
| Shared household with the affected person | ||||
| Yes | 85 | 43 | 91 | 45 |
| No | 80 | 41 | 84 | 42 |
| Sometimes | 31 | 16 | 27 | 13 |
| Living situation | ||||
| In a city/town | 183 | 93 | 185 | 92 |
| On the country-side | 13 | 7 | 17 | 8 |
| Education | ||||
| Elementary school | 9 | 5 | 14 | 7 |
| Upper secondary school | 35 | 18 | 34 | 17 |
| University/higher education | 150 | 76 | 149 | 74 |
| Other | 2 | 1 | 5 | 2 |
| Work situation | ||||
| Employed | 153 | 78 | 147 | 73 |
| Not working | 43 | 22 | 55 | 27 |
| Main diagnosis as reported by participants | ||||
| Somatic diagnosis | 25 | 13 | 35 | 17 |
| Psychiatric diagnosis | 171 | 87 | 166 | 82 |
| Depression/anxiety disorders | 74 | 38 | 54 | 27 |
| Schizophrenia spectrum/psychotic disorders (incl. bipolar disorder) | 33 | 17 | 43 | 21 |
| Autism spectrum/neurodevelopmental disorders | 33 | 17 | 38 | 19 |
| Other (including personality disorders) | 28 | 14 | 30 | 15 |
| Missing | - | - | 1 | 1 |
| Time since diagnosis (in years) | ||||
| <1 | 9 | 4 | 15 | 8 |
| 1-5 | 72 | 37 | 65 | 32 |
| 6-10 | 37 | 19 | 41 | 20 |
| 11-15 | 23 | 12 | 27 | 13 |
| >15 | 55 | 28 | 54 | 27 |
| Type of support to patient (several answers possible) | ||||
| Emotional support | 185 | 94 | 186 | 92 |
| Help with daily care (e.g. hygiene, dressing) | 31 | 16 | 27 | 13 |
| Practical support (e.g. cleaning, transportation) | 125 | 64 | 134 | 66 |
| Economical support | 86 | 44 | 85 | 42 |
| Contact with health care/other organizations | 99 | 51 | 112 | 55 |
| Other help | 60 | 31 | 55 | 27 |
| Caregiving in hours/week | ||||
| <1 | 7 | 3 | 13 | 7 |
| 1-15 | 112 | 57 | 122 | 60 |
| 16-30 | 30 | 15 | 25 | 12 |
| 31-45 | 9 | 5 | 10 | 5 |
| >45 | 8 | 4 | 10 | 5 |
| “feels like 24/7” | 9 | 5 | 4 | 2 |
| “difficult to say/don’t know” | 21 | 11 | 18 | 9 |
| Self-rated own physical health | ||||
| Very good | 30 | 15 | 31 | 15 |
| Good | 127 | 65 | 131 | 65 |
| Bad | 34 | 17 | 38 | 19 |
| Very bad | 5 | 3 | 2 | 1 |
| Self-rated own mental health | ||||
| Very good | 15 | 8 | 13 | 6 |
| Good | 93 | 47 | 91 | 45 |
| Bad | 84 | 43 | 92 | 46 |
| Very bad | 4 | 2 | 6 | 3 |
A link to the post intervention assessments (T2) was sent to all participants in both groups who had not actively dropped out, regardless of training time (Fig. 1). This included registered participants with 0 min's training time who had not actively dropped out. The assessments also included questions about usability, confounding factors and negative effects of training. Of the 179 participants in the experiment group and the 201 in the WLC who received a link to the post intervention assessments (T2), 75% (n = 136) and 79% (n = 160) respectively completed the questionnaire. Follow-up assessments (T3) were sent to the participants 3 months after termination of the test period, at which point 96 participants in the experiment group completed these.
Daily formal practice time was registered online for all participants on the program website (120 min = 1 week's training). The number of missing cases regarding training time for the experiment group was 10. This is due to participants not registering, or registering to the program website but not initiating their training. These cases have been included in the 0–120 min interval below. If training was initiated, but did not proceed up to the fulfillment of the first 10 min' exercise, the training time was registered as 0 (experiment group n = 21) (=pre-treatment drop-out). In the experiment group at T2 (n = 136), 16% (n = 22) had a training time between 0 and 120 min (0 min: n = 6, included in the analyses), 27% (n = 37) between 121 and 480 min, and 57% (n = 77) between 481 and 960 min, whereas the figures in the respective training time intervals at the 3-month follow-up (n = 96) were 21% (n = 20), 22% (n = 21) and 57% (n = 55).
4. Data analyses
General linear models with repeated measures analyses of variance were performed on the responses of completers to evaluate between group comparisons of the intervention's impact on primary (FFMQ) and secondary (SCS-SF, PSS, CarerQoL-7D, Montgomery-Borgatta Caregiver Burden) outcomes as compared to the WLC. A GLM model was used to analyze whether drop-outs at T3 differed from remainders on changes in overall mindfulness scores between T1 and T2. Independent samples t-test was performed to investigate baseline differences between completers and dropouts at T2. In addition, an intention-to-treat analysis using GLM models was performed including the subscales and global scale of the primary outcome measure. In order to perform this, data for participants who completed the T1 measures but not the T2 assessments were imputed using the multiple imputation module in IBM SPSS.
Paired sample t-tests were carried out to compare means on primary and secondary outcomes between pre-intervention and follow-up for the experiment group. Between-group effect sizes for primary and secondary outcomes for the experiment group and the WLC post intervention were calculated, and within-group effect sizes for the experiment group at follow-up, using Cohen's d. Effect sizes below 0.5 were considered as small, between 0.5 and 0.8 as medium, and above 0.8 as large (Cohen, 2013). Spearman correlation analyses were used to investigate the association between amount of exercise reported and outcome of the intervention. IBM SPSS Statistics package version 24 was used in all statistical analyses.
A total score was calculated to obtain an overall value of system usability (SUS) (Brooke, 1996). Qualitative data from the usability questionnaires (T2, T3) was analyzed with content analysis (Graneheim and Lundman, 2004) and quantitative data is reported with descriptive statistics (Tables 4 and 5).
Table 4.
Aspects of usability and value as extracted from the free-text answers at T2/T3 (experiment group).
| Technical advantages and motivation to use |
Related to technology: Easy access and use, independence and flexibility of use (place, time, technical platform, independent use) Easy access as a safety, “a coach in my pocket” Related to contents: Speaker's voice, guiding voice - agreeable and easy to follow Type and variation of exercises (including mindful yoga), easy to grasp Effects as motivator: Positive effects of training (e.g. relaxation, calmness, better sleep, energy, conscious awareness, reflection, supportive tool, break automatic behavior/reactions, kinder with myself, better balance, feeling that I can influence my situation/well-being, reminder to self-care) |
| Disadvantages and barriers to use |
Related to technology: Technical difficulties (e.g. log-in procedure, insecurity regarding registration of training time online) Navigation difficulties Inability to browse among exercises and choose freely (note: can be done once the whole program has been completed) Dependence on Internet connection Related to contents: Lack of variation (exercises, instructions, speaker's voice) Too much talking (wish for more silent periods), wording, speaker's voice Certain contents provoking/difficult to relate to/not experienced as relevant for one's situation Difficulties with certain parts of the self-compassion exercises and conscious movements Commercial feel Related to own situation: Lack of time and/or peace and concentration to do the training Lack of motivation and/or support Life situation/events (e.g. move, stress at work, family conflicts, fatalities, health issues: own or/and patient's) Falling asleep during training |
| Other feedback and suggestions |
Related to technology: Internet-independent application Possibility to browse through the exercises (not possible before completion of full program) Easier navigation Clearer instructions Related to contents: More varied exercises and speaker voices Shorter daily training or longer test period |
| Negative effects of training | The training as another stressful demand, not keeping the pace induces negative feelings (failure, guilt, stress) Stirs up strong and sometimes negative feelings (can be experienced as negative, but also as positive and soothing) Periodically diminished well-being Too upsetting in connection with a crisis |
| Confounding factors |
Other sources of support: Own support from health professional (e.g. psychologist, counselor, physician) Emotional and/or practical support from friends/family/colleagues More support from other family members towards the patient (unburdening the participating caregiver) Professional support for the patient (e.g. medication, housing) Other sources of support (e.g. yoga, holiday) Negative life events: Ill health, conflicts or fatalities in family Deterioration in patient's and/or own health Work-related stress Economic deterioration due to own or/and patient's illness Other stressful life events (e.g. move, relationship break-up) |
Table 5.
Usability aspects and potential confounding factors as experienced during the test period and by the 3-months follow-up (free-text answers and descriptive statistics, T2/T3).
| Assessments at T2 - after the experiment group's test period | Experiment group n = 136 | % | WLC n = 160 | % |
|---|---|---|---|---|
| Mental health fluctuations in the patient during the test period | ||||
| Improved | 16 | 12 | 30 | 19 |
| Unchanged | 58 | 43 | 43 | 27 |
| Deteriorated | 8 | 6 | 24 | 15 |
| Fluctuated (better and worse) | 26 | 19 | 44 | 28 |
| Don't know | 15 | 11 | 15 | 9 |
| Not relevant | 13 | 9 | 4 | 2 |
| Physical health fluctuations in the patient during the test period | ||||
| Improved | 9 | 7 | 19 | 12 |
| Unchanged | 76 | 56 | 65 | 41 |
| Deteriorated | 10 | 7 | 25 | 16 |
| Fluctuated (better and worse) | 13 | 9 | 32 | 20 |
| Don't know | 13 | 10 | 12 | 7 |
| Not relevant | 15 | 11 | 7 | 4 |
| Support from other sources during the test period with potential positive effects | ||||
| Yes | 44 | 32 | 34 | 21 |
| No | 90 | 66 | 116 | 73 |
| Don't know | 2 | 2 | 10 | 6 |
| Life events during the test period with potential negative effects | ||||
| Yes | 45 | 33 | 64 | 40 |
| No | 91 | 67 | 87 | 54 |
| Don't know | – | – | 9 | 6 |
| Assessments at T2 – after the experiment group's test periods | Experiment group n = 136 | % |
|---|---|---|
| Negative effects of training | ||
| Yes | 30 | 22 |
| No | 97 | 71 |
| Don't know | 9 | 7 |
| e-mail reminders positive for training | ||
| Yes | 73 | 54 |
| No | 7 | 5 |
| Neither nor | 52 | 38 |
| Don't know | 4 | 3 |
| Potentially pursue training with a similar program (T2) | ||
| Yes | 100 | 74 |
| Maybe | 26 | 19 |
| No | 8 | 6 |
| Don't know | 2 | 2 |
| Would/has recommend(ed) the program to others | ||
| Yes | 100 | 74 |
| Maybe | 26 | 19 |
| No | 5 | 4 |
| Don't know | 5 | 3 |
| Assessments at T3–3 months after termination of the test period | Experiment group n = 96 | % |
| Continued training after test period | ||
| Yes, 4–7 days/week | 6 | 6 |
| Yes, 2–3 days/week | 16 | 17 |
| Yes, 1–7 days/month | 35 | 36 |
| No, hardly ever | 39 | 41 |
| Experienced continued training after test period as valuable | ||
| Yes, very | 23 | 24 |
| Yes, partly | 35 | 36 |
| No, hardly or not at all | 5 | 5 |
| Don't know | 12 | 13 |
| Not relevant (did not pursue training) | 19 | 20 |
| Missing | 2 | 2 |
| Potentially pursue training | ||
| Yes | 66 | 69 |
| Maybe | 20 | 21 |
| No | 3 | 3 |
| Don't know | 7 | 7 |
| Would/has recommend(ed) the program to others | ||
| Yes | 68 | 71 |
| Maybe | 19 | 20 |
| No | 4 | 4 |
| Don't know | 5 | 5 |
5. Results
Mindfulness (FFMQ) significantly improved pre-post intervention in comparisons between the experiment and the WLC group. This was the case for both the overall score and all subscale scores (p = 0.001) with effect sizes mainly medium in size (range 0.51–0.74), except for the Acting with Awareness and the Describing subscales, which were small (0.33 and 0.30 respectively). An intention to treat analysis verified these results, showing no differences in results concerning outcome regarding the primary measure. There were significant and positive improvements in the experiment group between pre-intervention and follow-up in both the overall and the subscale scores with P-values 0.001 and within-group effect sizes were in the range 0.40–0.82 (Table 3). It is noticeable that most effect sizes except for the Observing subscale are larger at follow-up than post intervention, with a large size effect for the FFMQ global sum (0.82). With the means of a general linear model we examined whether there was a significant difference in outcome for the mindfulness global sum pre-post intervention between caregivers of a person with mental illness (85% of the T2 sample) compared to caregivers of a person with somatic illness (15%), which there wasn't.
Table 3.
Outcome of pre-post intervention comparisons between groups regarding Mindfulness, Self-Compassion, Perceived Stress, CarerQoL-7D and Montgomery-Borgatta Caregiver Burden Scale (repeated measures ANOVA) and pre-intervention follow-up in the experimental group (paired samples t-test).
| Outcome measure |
Baseline |
Post intervention |
Pre-post-intervention |
Follow-up |
Pre-intervention-follow-up |
||||
|---|---|---|---|---|---|---|---|---|---|
| Experiment group (n = 196) |
WLC (n = 202) |
Experiment group (n = 136) |
WLC (n = 160) |
Experiment group (n = 96) |
|||||
| M ± SD | M ± SD | M ± SD | M ± SD | p-value | Effect size | M ± SD | p-value | Effect size | |
| FFQM Global Sum | 119.7 ± 20.2 | 116.8 ± 19.7 | 133.4 ± 18.9 | 116.7 ± 21.2 | 0.001 | 0.69 | 134.7 ± 19.9 | 0.001 | 0.82 |
| Non-reactivity | 18.8 ± 4.7 | 18.5 ± 4.4 | 21.3 ± 4.1 | 18.45 ± 4.7 | 0.001 | 0.56 | 21.9 ± 4.1 | 0.001 | 0.71 |
| Observing | 24.5 ± 5.8 | 24.1 ± 5.9 | 28.4 ± 4.9 | 23.9 ± 5.5 | 0.001 | 0.74 | 27.7 ± 5.6 | 0.001 | 0.61 |
| Acting with Awareness | 23.8 ± 6.6 | 22.3 ± 6.1 | 26.0 ± 5.6 | 22.6 ± 6.2 | 0.001 | 0.33 | 26.8 ± 5.7 | 0.001 | 0.60 |
| Describing | 27.7 ± 6.5 | 27.6 ± 6.1 | 29.2 ± 5.6 | 27.3 ± 6.3 | 0.001 | 0.30 | 29.5 ± 5.9 | 0.001 | 0.40 |
| Non-judging | 24.9 ± 7.1 | 24.2 ± 7.2 | 28.5 ± 6.7 | 24.5 ± 7.5 | 0.001 | 0.51 | 28.8 ± 7.0 | 0.001 | 0.58 |
| SCS-SF Global Sum | 33.2 ± 8.2 | 32.7 ± 8.5 | 38.0 ± 8.7 | 33.2 ± 9.0 | 0.001 | 0.43 | 38.8 ± 9.9 | 0.001 | 0.65 |
| Self-Kindness | 5.5 ± 1.9 | 5.5 ± 1.8 | 6.1 ± 1.7 | 5.5 ± 1.7 | 0.001 | 0.38 | 6.2 ± 1.9 | 0.001 | 0.37 |
| Self-Judgment Common Humanity Isolation |
5.8 ± 2.2 5.9 ± 1.8 7.3 ± 1.9 |
6.2 ± 2.4 6.0 ± 1.9 7.4 ± 2.0 |
5.0 ± 2.3 6.8 ± 1.7 6.5 ± 2.1 |
6.1 ± 2.3 6.1 ± 1.9 7.2 ± 2.0 |
0.001 0.001 0.003 |
0.36 0.39 0.32 |
7.0 ± 2.3 7.0 ± 1.9 5.6 ± 2.1 |
0.001 0.001 0.001 |
0.45 0.58 0.43 |
| Mindfulness | 6.6 ± 1.8 | 6.6 ± 1.8 | 7.1 ± 1.6 | 6.5 ± 1.8 | 0.001 | 0.42 | 7.2 ± 1.9 | 0.001 | 0.35 |
| Over-identification | 7.6 ± 1.9 | 7.9 ± 1.9 | 6.6 ± 2.2 | 7.5 ± 2.1 | 0.007 | 0.30 | 5.8 ± 2.2 | 0.001 | 0.77 |
| PSS | 33.3 ± 7.2 | 34.9 ± 6.7 | 29.2 ± 7.5 | 34.1 ± 7.1 | 0.001 | 0.46 | 29.3 ± 8.3 | 0.001 | 0.53 |
| Montgomery-Borgatta Caregiver Burden | |||||||||
| Relationship burden | 13.8 ± 5.2 | 13.4 ± 4.8 | 13.6 ± 5.2 | 13.2 ± 4.7 | 0.709 | 0.03 | 12.9 ± 4.9 | 0.110 | 0.12 |
| Objective burden | 20.2 ± 5.6 | 19.5 ± 5.4 | 19.3 ± 5.6 | 19.4 ± 5.7 | 0.102 | 0.12 | 18.5 ± 5.7 | 0.001 | 0.26 |
| Stress/subjective burden | 19.1 ± 3.8 | 19.3 ± 3.8 | 17.7 ± 4.1 | 18.4 ± 4.2 | 0.141 | 0.12 | 17.0 ± 4.4 | 0.001 | 0.55 |
| Uplifts | 14.2 ± 4.8 | 14.5 ± 5.0 | 15.1 ± 5.2 | 14.7 ± 5.4 | 0.062 | 0.15 | 15.5 ± 5.3 | 0.002 | 0.25 |
| CarerQoL-7D | |||||||||
| Fulfillment | 1.93 ± 0.63 | 1.87 ± 0.58 | 1.97 ± 0.58 | 1.86 ± 0.59 | 0.419 | 0.08 | 1.98 ± 0.66 | 0.196 | 0.12 |
| Relational problems | 2.13 ± 0.76 | 2.11 ± 0.70 | 2.01 ± 0.74 | 2.06 ± 0.69 | 0.312 | 0.10 | 1.97 ± 0.70 | 0.004 | 0.12 |
| Mental health problems | 2.24 ± 0.63 | 2.29 ± 0.66 | 2.11 ± 0.60 | 2.26 ± 0.61 | 0.184 | 0.16 | 1.94 ± 0.66 | 0.001 | 0.50 |
| Problems with daily | |||||||||
| Activities | 1.94 ± 0.65 | 1.94 ± 0.69 | 1.84 ± 0.71 | 1.92 ± 0.71 | 0.312 | 0.11 | 1.64 ± 0.63 | 0.001 | 0.44 |
| Financial problems | 1.32 ± 0.54 | 1.28 ± 0.49 | 1.35 ± 0.61 | 1.34 ± 0.55 | 0.587 | 0.05 | 1.25 ± 0.52 | 0.580 | 0.06 |
| Support | 1.72 ± 0.68 | 1.84 ± 0.72 | 1.82 ± 0.71 | 1.84 ± 0.69 | 0.175 | 0.14 | 1.86 ± 0.73 | 0.021 | 0.21 |
| Physical problems | 1.79 ± 0.64 | 1.85 ± 0.64 | 1.78 ± 0.68 | 1.91 ± 0.70 | 0.291 | 0.10 | 1.65 ± 0.63 | 0.057 | −0.19 |
| CarerQoL-VAS | 4.27 ± 2.21 | 3.87 ± 2.23 | 5.19 ± 2.38 | 4.51 ± 2.24 | 0.229 | 0.20 | 5.07 ± 2.23 | 0.001 | 0.37 |
*p < 0.05.
There were significant improvements pre-post intervention regarding self-compassion in comparisons between the groups. The experiment group showed significant changes in the global SCS-SF score and in several of the SCS-SF's subscales at the p = 0.001 level, except for the Isolation (p = 0.003) and Over-Identification (p = 0.007) subscales. Effect sizes for the global sum score and all subscales were small (range 0.30–0.43). Comparisons pre-intervention and follow-up showed significant within-group improvements in the experiment group in all subscales, with effect sizes in the range 0.35–0.77.
Significant decreases in favor of the experimental group were observed in the perceived stress scale (PSS) in pre-post intervention comparisons between the groups (p = 0.001 and ES = 0.46). Within-group comparisons in the experimental group showed a significant improvement between pre-intervention and follow-up (p = 0.001 and ES = 0.53).
Comparisons between the groups pre-post intervention on caregiver burden (CarerQoL-7D) showed no significant improvements in favor of the experimental group in any of the 7 dimensions nor the VAS scale. The latter indicates levels of happiness with caregiving experiences. However, within-group comparisons pre-intervention and follow-up in the experiment group showed significant improvements in Mental Health Problems (p = 0.001, ES 0.12), Problems with Daily Activities (p = 0.001, ES 0.44) and the CarerQol-VAS (p = 0.001, ES 0.37).
Regarding the Montgomery-Borgatta Caregiver Burden Scale, comparisons between the groups pre-post intervention showed no significant improvements for the experimental group on any of the subscales. Within-group comparisons pre-intervention and follow-up, however, showed significant improvements in objective (p = 0.001, ES 0.26) and stress/subjective burden (p = 0.001, ES.55), and uplifts (p = 0.002, ES.25), but no improvements in relationship burden.
Of the 136 participants in the experiment group completing the usability questionnaire at T2, 133 (n = 3 missing) reported rather low overall SUS scores (range 5–40, mean = 21). Additional questions on usability, also including free-text answers, illuminated motivators and barriers to use, which related to technical aspects (e.g. flexibility of use vs technical hitches), program contents (e.g. type of exercises and delivery format) and the participants' life situation (e.g. life events) (Table 4, Table 5). Effects of training were described as motivating and perceiving the training as another daily demand was stressful. Over half of the participants experienced the weekly e-mail reminders as positive for their training. While 71% answered “no” to whether their training had any negative effects, 22% answered “yes”. As to potential confounders, mental and/or physical health fluctuations in the patient during the test period were reported in both groups. A majority reported not having additional sources of support during the test period, while 32% and 21% in the respective groups did. As to life events occurring and affecting the participants negatively during the test period, 33% and 40% respectively answered “yes”. A majority of participants who completed the T3 assessments reported that they had maintained their training after the test period, although with varying intensity and 60% experienced their training as (partly or very) valuable. Most participants in the experimental group at both T2 and T3 reported that they were open to pursuing their training and that they would/had recommend(ed) the program to others (see Table 5).
Amount of exercise: We examined whether there was a relationship between the amount of exercises performed during the intervention and changes in mindfulness through a correlational analysis. It showed a significant small association of 0.29 pre-post intervention and 0.33 between pre-intervention and follow-up, indicating that amount of exercise accounted for around 8% and 11% respectively of the variation in mindfulness changes.
No significant differences between completers and drop-outs at T2 were found on sociodemographic variables such as gender, age, employment status, or relationship to the patient. There were however significantly more participants with a higher education level (university/higher education) (p = 0.24) among completers at T2. Considering the sizeable number of participants dropping out from the investigation between assessments at T2 and T3, we analyzed whether dropouts differed from remainders with regard to outcome pre-post intervention in the primary outcome measure mindfulness (global sum). The analysis showed no differences between the groups regarding changes in mindfulness, which indicates that those participating in the follow-up assessments were representative for the sample participating in the intervention.
6. Discussion
In accordance with the literature, significant improvements were found in the primary outcome mindfulness, currently with mainly medium effect sizes in both the global sum scale and all subscales both post intervention and at follow-up. The effect size increase for all the FFMQ subscales except one (Observing) and the large effect size of the global sum scale at follow-up is, however, noticeable. Similar improvements were found in previous studies with the same intervention (Stjernswärd and Hansson, 2016a; Stjernswärd and Hansson, 2017), although effect sizes were slightly weaker in the current study compared to the earlier effectiveness study (Stjernswärd and Hansson, 2017). Significant improvements in benefit for the experimental group were also found for perceived stress, with a small effect size post intervention and medium effect size at follow-up. Previous studies showed medium effect sizes already post intervention (Stjernswärd and Hansson, 2016a; Stjernswärd and Hansson, 2017). MBI such as MBSR have been associated with lowered levels of perceived stress and negative affect, with linear decreases as a function of both time and cumulative number of days of mindfulness training, suggesting a dose-effect relationship (Snippe et al., 2017). Nevertheless, even shorter interventions show beneficial health outcomes (Carmody and Baer, 2009; Zeidan et al., 2010; Krusche et al., 2012; Boettcher et al., 2013; Stjernswärd and Hansson, 2017), which is also the case in the current study. Current associations between training time and effect were smaller compared to previous studies (Stjernswärd and Hansson, 2016a; Stjernswärd and Hansson, 2017). Nevertheless, the enhanced effect sizes at follow-up may speak for the value of maintained training, although there is an insecurity as to how much more the remaining participants had practiced by the time of the 3-month assessment. Training time was registered until T3, however training time > 960 min (complete program) could not be registered online and the amount of self-reported maintained training was not specific enough to draw any further dose-effect related conclusions.
The current intervention was targeted at a wider audience of caregivers, speaking for generalizability of the results. Half of the participants reported low levels of mental health speaking for the relevance of targeting this population with supportive interventions such as MBI, which can help decrease stress reactivity (Kabat-Zinn, 2009) and enhance the ability to communicate and respond constructively to stress, including relationship stress (Barnes et al., 2007). Increased self-compassion can also improve interpersonal relationships (Hofmann et al., 2011; Jazaieri et al., 2014; Yadavaia et al., 2014). It can help reduce shame, negative affect and emotional exhaustion, while increasing positive affect (Leary et al., 2007; Neff et al., 2007; Neff and Vonk, 2009). In accordance with previous findings (Stjernswärd and Hansson, 2016a; Stjernswärd and Hansson, 2017), significant improvements were found for self-compassion including most of its subscales. A number of participants, however, commented on difficulties with the self-compassion exercises, such as difficulties with including “all humanity” or “others” in their training, or feeling provoked because they already cared a lot for others. Additional (virtual) support may be valuable in addressing such resistance, which may activate a threat response (Rockliff et al., 2008) and increase the vulnerability to mental health problems (Gilbert et al., 2011) instead of opening up for the beneficial effects of compassion.
Regarding caregiver burden, the study showed no significant improvements post intervention in the CarerQoL-7D, although some dimensions showed significant improvements at follow-up. Previous findings were mixed, with significant but small improvements on some dimensions of caregiver burden (Stjernswärd and Hansson, 2016a; Stjernswärd and Hansson, 2017). As previously discussed (Stjernswärd and Hansson, 2017), the CarerQoL-7D does not appear to capture central effects of the intervention, although the latter may have indirect positive effects on the caregivers' situation and experiences of burden. The Montgomery-Borgatta Caregiver Burden Scale was added to investigate the appropriateness of a different instrument to measure potential changes in burden. Although no significant changes in any of the subscales were found post intervention, significant but mostly small improvements were found at follow-up for uplifts, objective and subjective burden, but not for relationship burden. Coping is viewed as a central mediator that can affect the outcomes of stress (Pearlin et al., 1990). In the process of decreasing stress reactivity (Kabat-Zinn, 2009), MBI can help caregivers cope more constructively with stress. Such strategies may help reduce the negative effects of stress on caregivers' health and relationships, which in turn may indirectly contribute to alleviate the caregivers' situation. Potential direct effects on caregiver burden is, however, an issue for further research. As reported in the free-text answers, the training was a reminder and opportunity for respite and to make own time without feeling guilty. The positive effects of training can contribute to increase caregivers' well-being and QoL, which also goes in line with previous findings (Banerjee et al., 2017).
The majority of participants reported spending 1–15 h weekly caring for the affected person, which is not uncommon (National Alliance for Caregiving and AARP, 2004; Turcotte, 2013). Caregivers also report spending care time equaling a full-time job (Turcotte, 2013), representing a source of worry and stress. MBI can help increase psychological flexibility (Hayes et al., 1999), and the ability to accept and connect with the present moment, including negative thoughts, feelings and bodily sensations (Hayes, 2002), potentially addressing caregiver distress (Jansen et al., 2015; Jansen et al., 2017). Mindfulness can contribute to an increased and non-judgmental acceptance of what is, and an enhanced ability to be in the present moment rather than to ruminate about the past or worry about the future (Kabat-Zinn, 2009). MBI may help caregivers come to an acceptance of the situation, while also making space for grief and other negative emotions related to their kin's illness (Jansen et al., 2017). Although many of the problems associated with being a caregiver cannot be solved with MBI, such intervention may be an additional coping tool.
There is a need for identifying central key components and mechanisms of change in web-based caregiver-targeted interventions (Guay et al., 2017). Theoretically grounded interventions (Webb et al., 2010) and interventions including behavior change techniques (BCT) (Guay et al., 2017) appear to be more efficacious in improving caregiver outcomes. Moreover, interventions providing stress management techniques – which caregivers covet (National Alliance for Caregiving and AARP 2015) - appear to have the greatest effect on behavior (Webb et al., 2010). The current intervention has its theoretical underpinnings in the beneficial effects of MBI, for which the underlying effective mechanisms still need to be illuminated, especially when adapted to new populations and contexts (Crane et al., 2017). In MBI, however, a relationship change towards one's experiences, whether pleasant or unpleasant, is associated with decreased levels of distress (Kabat-Zinn, 2009; Crane et al., 2017). There is evidence for the association of MBSR/MBCT with reduced cognitive and emotional reactivity, and reduced rumination and worry (Gu et al., 2015). In this respect, stress management through MBI may represent a potential mediator of burden for caregivers.
A fifth of the participants reported negative effects of their training, which is important to bear in mind. Anxiety about not succeeding in maintaining the training pace was a source of stress that can decrease motivation and adherence. Other reported negative effects were the surfacing of strong emotions, anxiety from a participant in crisis, and at times reduced well-being. Awareness about unpleasant thoughts, feelings and experiences, idealizing practice or setting impossible standards, and sleepiness (Kabat-Zinn, 2017a) can be obstacles to (but also opportunities for) training, similarly as self-criticism for disengaging from practice (Banerjee et al., 2017). Discipline and motivation to engage in mindfulness practice are key and obstacles can be turned into opportunities if embraced in awareness (Kabat-Zinn, 2017b). Although severe mental illness was an exclusion criterion and the participants were informed that the training can give rise to strong emotions, crises can occur at any time during the test period, which requires vigilance.
Lack of motivation is a barrier in e-health interventions (Kampmeijer et al., 2016), as also seen in the current study, which is why ways of upholding motivation may improve adherence and the potential beneficial effects of training. Human support is commonly used in caregiver interventions online (Guay et al., 2017) and can enhance adherence (Kelders et al., 2012; Kampmeijer et al., 2016) and intervention efficacy (Webb et al., 2010). Moreover, reminders (Fry and Neff, 2009; Webb et al., 2010) and the RCT format appear (for different potential reasons) to increase adherence (Kelders et al., 2012), which was also mentioned by participants in a previous study (Stjernswärd and Hansson, 2016b). Lack of support and feedback can be further barriers, while ease of use, prompts and personal support may facilitate the use of such interventions (Kampmeijer et al., 2016), as partly illuminated in the current study. A possibility for the participants to discuss their practice may be a valuable complement to the web-based program.
The SUS scores were surprisingly low, especially in comparison with earlier high usability scores (Stjernswärd and Hansson, 2017), although many participants commented upon the program's ease and flexibility of use. The supplementary usability questions may help shed light onto factors affecting these ratings negatively and areas for enhancements. Weaving in an even clearer rationale in the program, among others, may help clarify the mindfulness principles and uphold motivation, as seen in previous studies (Banerjee et al., 2017).
6.1. Limitations
Although the current design was a RCT, the intervention was not compared against an alternative control intervention. The use of self-report measures is a potential limitation, as is the potential selection bias, limiting generalizability of the results. The participants consisted of a majority of middle-aged women and mothers to an ill person, which also goes in line with previous studies (Guay et al., 2017; Stjernswärd and Hansson, 2016a; Stjernswärd and Hansson, 2017), the literature on caregiving (e.g. Fox and Brenner, 2012) and engagement in online interventions. There was also a significant overrepresentation of participants with a higher education among the completers at T2, limiting representativity and generalizability of the current findings. The presence of potential confounders was explored, such as the occurrence of support or negative life events during the test period, or health fluctuations in the patient – which were present in both groups. Slightly more participants in the experiment group reported additional sources of support compared to the WLC and fewer also reported negative life events, possibly affecting the interpretation of the current results.
Dropout rates for the experiment group were 30% (n = 59) and 20% (n = 40) at T2 and T3, respectively. Dropout rates in earlier MBI online range between 7.7 and 52.3% (Fish et al., 2016) (Fish et al., 2016) and the average dropout rates for internet-based treatments for psychological disorders is 35% (Melville et al., 2010). Kelders et al. (2012) found an average adherence of 50% to web-based health interventions (range <10%–>90%), further illuminating challenges with adherence and motivation in online interventions. Due to the high drop-out rate, an ITT analysis was performed on the primary outcome mindfulness, resulting in equivalent findings, which indicates the validity of the results. A majority of the participants in the present study completed between 50 and 100% of the suggested training dose, and several participants reported that they worried about not being able to complete the full program within the study's test period, creating additional stress. Training undeniably requires motivation, time and discipline (Stjernswärd and Hansson, 2016b; Kabat-Zinn, 2017b). The potential value of including further psychoeducation (clearer rationale) and virtual support to address difficult experiences that emerge during practice (Banerjee et al., 2017) and self-criticism (e.g. related to non-adherence to suggested training dose) (Langdon et al., 2011) should be explored. Feedback on usability of the program also highlights areas for improvement in future MBI online.
6.2. Conclusions
Web-based mindfulness programs can be a potentially cost-effective tool to support caregivers coping with stress and burden, preventing further ill health and costs to society. Further research is needed to corroborate and explore the effectiveness and usability of such interventions, possibly adding instructor support (e.g. online or by phone) to enhance the program's beneficial effects. Caregiver interventions can be tailored to better suit their users and enhance their beneficial outcomes through an understanding of potential barriers and facilitators of use. Attention to ways of supporting motivation and adherence to the programs may contribute to enhanced benefits of mindfulness practice, such as increased levels of mindfulness and self-compassion, and decreased levels of perceived stress, and indirectly of caregiver burden.
Declarations of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Mental illness (abbreviated MI).
Mindfulness-based interventions (abbreviated MBI).
Contributor Information
Sigrid Stjernswärd, Email: sigrid.stjernsward@med.lu.se.
Lars Hansson, Email: lars.hansson@med.lu.se.
References
- Adelman R.D., Tmanova L.L., Delgado D., Dion S., Lachs M.S. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052–1060. doi: 10.1001/jama.2014.304. [DOI] [PubMed] [Google Scholar]
- Baer R.A., Smith G.T., Hopkins J., Krietemeyer J., Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer R.A., Smith G.T., Lykins E., Button D., Krietemeyer J., Sauer S., Walsh E., Duggan D., Williams J.M. Construct validity of the five facet mindfulness questionnaire in meditating and non-meditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Banerjee M., Cavanagh K., Strauss C. A qualitative study with healthcare staff exploring the facilitators and barriers to engaging in a self-help mindfulness-based intervention. Mindfulness. 2017;8(6):1653–1664. doi: 10.1007/s12671-017-0740-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangor A., Kortum P., Miller J. An empirical evaluation of the system usability scale. Int. J. Hum. Comput. Interact. 2008;24(6):574–594. [Google Scholar]
- Barnes S., Brown K.W., Krusemark E., Campbell W.K., Rogge R.D. The role of mindfulness in romantic relationship satisfaction and responses to relationship stress. J. Marital. Fam. Ther. 2007;33(4):482–500. doi: 10.1111/j.1752-0606.2007.00033.x. [DOI] [PubMed] [Google Scholar]
- Bloom P., Ho L., Vega J.G., Pasinetti G. P02. 37. Mindfulness for caregivers. BMC Complement. Altern. Med. 2012;12(Suppl. 1):P93. [Google Scholar]
- Boettcher J., Åström V., Påhlsson D., Schenström O., Andersson G., Carlbring P. Internet-based mindfulness treatment for anxiety disorders: a randomised controlled trial. Behav. Ther. 2013;45(2):241–253. doi: 10.1016/j.beth.2013.11.003. [DOI] [PubMed] [Google Scholar]
- Boyer L., Caqueo-Urízar A., Richieri R., Lancon C., Gutiérrez-Maldonado J., Auquier P. Quality of life among caregivers of patients with schizophrenia: a cross-cultural comparison of Chilean and French families. BMC Fam. Pract. 2012;13(1):42. doi: 10.1186/1471-2296-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooke J. SUS - a quick and dirty usability scale. In: Jordan P.W., Thomas B., Weerdmeester B.A., McClelland A.L., editors. Usability Evaluation in Industry. Taylor and Francis; London: 1996. [Google Scholar]
- Brouwer W.B.F., Exel N.J.A., Gorp B., Redekop W.K. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual. Life Res. 2006;15(6):1005–1021. doi: 10.1007/s11136-005-5994-6. [DOI] [PubMed] [Google Scholar]
- Caqueo-Urízar A., Gutiérrez-Maldonado J., Miranda-Castillo C. Quality of life in caregivers of patients with schizophrenia: A. Health Qual. Life Outcomes. 2009;7:84. doi: 10.1186/1477-7525-7-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmody J., Baer R.A. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. J. Clin. Psychol. 2009;65(6):627–638. doi: 10.1002/jclp.20555. [DOI] [PubMed] [Google Scholar]
- Cohen J. Academic Press; 2013. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- CONSORT Checklist. Transparent Reporting of Trials. 2010. http://www.consort-statement.org/
- Cormac I., Tihanyi P. Meeting the mental and physical healthcare needs of carers. Adv. Psychiatr. Treat. 2006;12(3):162–172. [Google Scholar]
- Crane R.S., Brewer J., Feldman C., Kabat-Zinn J., Santorelli S., Williams J.M.G., Kuyken W. What defines mindfulness-based programs? The warp and the weft. Psychol. Med. 2017;47(6):990–999. doi: 10.1017/S0033291716003317. [DOI] [PubMed] [Google Scholar]
- de Vibe M., Bjørndal A., Tipton E., Hammerstrøm K.T., Kowalski K., Bjørndal A. Mindfulness based stress reduction (MBSR) for improving health, quality of life, and social functioning in adults. Campbell Syst. Rev. 2012;8(3) [Google Scholar]
- Epstein-Lubow G., McBee L., Darling E., Armey M., Miller I.W. A pilot investigation of mindfulness-based stress reduction for caregivers of frail elderly. Mindfulness. 2011;2(2):95–102. [Google Scholar]
- Eskin M., Parr D. Department of Psychology University of Stockholm; 1996. Introducing a Swedish Version of an Instrument Measuring Mental Stress. [Google Scholar]
- Etters L., Goodall D., Harrison B.E. Caregiver burden among dementia patient caregivers: a review of the literature. J. Am. Acad. Nurse Pract. 2008;20(8):423–428. doi: 10.1111/j.1745-7599.2008.00342.x. [DOI] [PubMed] [Google Scholar]
- Feinberg L., Reinhard S.C., Houser A., Choula R. Insight on the Issue. vol. 51. 2011. Valuing the invaluable: 2011 update, the growing contributions and costs of family caregiving; pp. 1–28. [Google Scholar]
- Fish J., Brimson J., Lynch S. Mindfulness interventions delivered by technology without facilitator involvement: what research exists and what are the clinical outcomes? Mindfulness. 2016;7(5):1011–1023. doi: 10.1007/s12671-016-0548-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox S., Brenner J. Pew Internet & American Life Project; Washington, DC: 2012. Family Caregivers Online. [Google Scholar]
- Fry J.P., Neff R.A. Periodic prompts and reminders in health promotion and health behavior interventions: systematic review. J. Med. Internet Res. 2009;11(2) doi: 10.2196/jmir.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert P., McEwan K., Matos M., Rivis A. Fears of compassion: development of three self-report measures. Psychol. Psychother. Theory Res. Pract. 2011;84(3):239–255. doi: 10.1348/147608310X526511. [DOI] [PubMed] [Google Scholar]
- Glück T.M., Maercker A. A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry. 2011;11(1):175. doi: 10.1186/1471-244X-11-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graneheim U.H., Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Grunfeld E., Coyle D., Whelan T., Clinch J., Reyno L., Earle C.C.…Glossop R. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. Can. Med. Assoc. J. 2004;170(12):1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu J., Strauss C., Bond R., Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol. Rev. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006. [DOI] [PubMed] [Google Scholar]
- Guay C., Auger C., Demers L., Mortenson W.B., Miller W.C., Gelinas-Bronsard D., Ahmed S. Components and outcomes of internet-based interventions for caregivers of older adults: systematic review. J. Med. Internet Res. 2017;19(9) doi: 10.2196/jmir.7896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes S.C. Buddhism and acceptance and commitment therapy. Cogn. Behav. Pract. 2002;9(1):58–66. [Google Scholar]
- Hayes S.C., Luoma J.B., Bond F.W., Masuda A., Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav. Res. Ther. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes S.C., Strosahl K.D., Wilson K.G. Guilford Press; New York: 1999. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. [Google Scholar]
- Hoefman R.J., Exel van, N Job A., Foets M., Brouwer W.B. Sustained informal care: the feasibility, construct validity and test–retest reliability of the CarerQol-instrument to measure the impact of informal care in long-term care. Aging Ment. Health. 2011;15(8):1018–1027. doi: 10.1080/13607863.2011.575351. [DOI] [PubMed] [Google Scholar]
- Hofmann S.G., Grossman P., Hinton D.E. Loving-kindness and compassion meditation: potential for psychological interventions. Clin. Psychol. Rev. 2011;31(7):1126–1132. doi: 10.1016/j.cpr.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel B.K., Lazar S.W., Gard T., Schuman-Olivier Z., Vago D.R., Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect. Psychol. Sci. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Hou R.J., Wong S.Y., Yip B.H., Hung A.T., Lo H.H., Chan P.H., Lo C.S., Kwok T.C., Tang W.K., Mak W.W., Mercer S.W., Ma S.H. The effects of mindfulness-based stress reduction program on the mental health of family caregivers: a randomized controlled trial. Psychother. Psychosom. 2014;83(1):45–53. doi: 10.1159/000353278. [DOI] [PubMed] [Google Scholar]
- ISO . 1998. ISO 9241–11 Ergonomic Requirements for Office Work With Visual Display Terminals (VDTs) - Part 11: Guidance on Usability. [Google Scholar]
- Jansen J.E., Haahr U.H., Lyse H., Pedersen M.B., Trauelsen A.M., Simonsen E. Psychological flexibility as a buffer against caregiver distress in families with psychosis. Front. Psychol. 2017;8:1625. doi: 10.3389/fpsyg.2017.01625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen J.E., Harder S., Haahr U.H., Lyse H., Pedersen M.B., Trauelsen A.M., Simonsen E. The role of metacognitions in expressed emotion and distress: a study on caregivers of persons with first-episode psychosis. Clin. Psychol. Psychother. 2015;22(6):525–532. doi: 10.1002/cpp.1907. [DOI] [PubMed] [Google Scholar]
- Jazaieri H., McGonigal K., Jinpa T., Doty J.R., Gross J.J., Goldin P.R. A randomized controlled trial of compassion cultivation training: effects on mindfulness, affect, and emotion regulation. Motiv. Emot. 2014;38(1):23–35. [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin. Psychol. Sci. Pract. 2003;10(2):144–156. [Google Scholar]
- Kabat-Zinn J. 2009. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness Delta. [Google Scholar]
- Kabat-Zinn J. Common obstacles to practice. Mindfulness. 2017;8(6):1713–1715. [Google Scholar]
- Kabat-Zinn J. Supports for your practice. Mindfulness. 2017;8(6):1716–1719. [Google Scholar]
- Kampmeijer R., Pavlova M., Tambor M., Golinowska S., Groot W. The use of e-health and m-health tools in health promotion and primary prevention among older adults: a systematic literature review. BMC Health Serv. Res. 2016;16(5):290. doi: 10.1186/s12913-016-1522-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelders S.M., Kok R.N., Ossebaard H.C., Van Gemert-Pijnen J.E. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J. Med. Internet Res. 2012;14(6) doi: 10.2196/jmir.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keng S., Smoski M.J., Robins C.J. Effects of mindfulness on psychological health: a review of empirical studies. Clin. Psychol. Rev. 2011;31(6):1041–1056. doi: 10.1016/j.cpr.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury B., Lecomte T., Fortin G., Masse M., Therien P., Bouchard V., Chapleau M., Paquin K., Hofmann S.G. Mindfulness-based therapy: a comprehensive meta-analysis. Clin. Psychol. Rev. 2013;33(6):763–771. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- Krusche A., Cyhlarova E., King S., Williams J.M.G. Mindfulness online: a preliminary evaluation of the feasibility of a web-based mindfulness course and the impact on stress. BMJ Open. 2012;2(3) doi: 10.1136/bmjopen-2011-000803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langdon S., Jones F.W., Hutton J., Holttum S. A grounded-theory study of mindfulness practice following mindfulness-based cognitive therapy. Mindfulness. 2011;2(4):270–281. [Google Scholar]
- Leary M.R., Tate E.B., Adams C.E., Batts Allen A., Hancock J. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J. Pers. Soc. Psychol. 2007;92(5):887. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- Lefley H.P. Family burden and family stigma in major mental illness. Am. Psychol. 1989;44(3):556. doi: 10.1037//0003-066x.44.3.556. [DOI] [PubMed] [Google Scholar]
- Lilja J.L., Frodi-Lundgren A., Hanse J.J., Josefsson T., Lundh L., Sköld C., Hansen E., Broberg A.G. Five facets mindfulness questionnaire—reliability and factor structure: a Swedish version. Cogn. Behav. Ther. 2011;40(4):291–303. doi: 10.1080/16506073.2011.580367. [DOI] [PubMed] [Google Scholar]
- Linehan M.M. Guilford Press; New York, NY: 1993. Cognitive Behavioral Treatment of Borderline Personality Disorder. [Google Scholar]
- Longacre M.L. Cancer caregivers information needs and resource preferences. J. Cancer Educ. 2013;28(2):297–305. doi: 10.1007/s13187-013-0472-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melville K.M., Casey L.M., Kavanagh D.J. Dropout from internet-based treatment for psychological disorders. Br. J. Clin. Psychol. 2010;49(4):455–471. doi: 10.1348/014466509X472138. [DOI] [PubMed] [Google Scholar]
- Montgomery R.J., Borgatta E.F., Borgatta M.L. Who should Care for the Elderly. 2000. Societal and family change in the burden of care; pp. 27–54. [Google Scholar]
- National Alliance for Caregiving and AARP Caregiving in the U.S. 2004. http://www.caregiving.org/data/04finalreport.pdf Available.
- National Alliance for Caregiving and AARP Caregiving in the US: a focused look at those caring for someone age 50 or older. Full report. 2009. https://assets.aarp.org/rgcenter/il/caregiving_09.pdf Available.
- Neff K. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity. 2003;2(2):85–101. [Google Scholar]
- Neff K.D., Rude S.S., Kirkpatrick K.L. An examination of self-compassion in relation to positive psychological functioning and personality traits. J. Res. Pers. 2007;41(4):908–916. [Google Scholar]
- Neff K.D., Vonk R. Self-compassion versus global self-esteem: two different ways of relating to oneself. J. Pers. 2009;77(1):23–50. doi: 10.1111/j.1467-6494.2008.00537.x. [DOI] [PubMed] [Google Scholar]
- Östman M., Hansson L. Appraisal of caregiving, burden and psychological distress in relatives of psychiatric inpatients. Eur. Psychiatry. 2004;19(7):402–407. doi: 10.1016/j.eurpsy.2004.06.030. [DOI] [PubMed] [Google Scholar]
- Pagnini F., Phillips D., Bosma C.M., Reece A., Langer E. Mindfulness as a protective factor for the burden of caregivers of amyotrophic lateral sclerosis patients. J. Clin. Psychol. 2015;72(1):101–111. doi: 10.1002/jclp.22235. [DOI] [PubMed] [Google Scholar]
- Paller K.A., Creery J.D., Florczak S.M., Weintraub S., Mesulam M.M., Reber P.J., Kiragu J., Rooks J., Safron A., Morhardt D., O'Hara M., Gigler K.L., Molony J.M., Maslar M. Benefits of mindfulness training for patients with progressive cognitive decline and their caregivers. Am. J. Alzheimer's Dis. Other Dement. 2014;30(3):257–267. doi: 10.1177/1533317514545377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L.I., Mullan J.T., Semple S.J., Skaff M.M. Caregiving and the stress process: an overview of concepts and their measures. The Gerontologist. 1990;30(5):583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pharoah F., Mari J., Rathbone J., Wong W. Cochrane Database of Systematic Reviews Issue. vol. 12. 2010. Family intervention for schizophrenia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips A.C., Gallagher S., Hunt K., Der G., Carroll D. Symptoms of depression in non-routine caregivers: the role of caregiver strain and burden. British Journal of Clinical form of the self-compassion scale. Clin. Psychol. Psychother. 2009;18(3):250–255. doi: 10.1348/014466508X397142. [DOI] [PubMed] [Google Scholar]
- Raes F., Pommier E., Neff K.D., Van Gucht D. Construction and factorial validation of a short form of the self‐compassion scale. Clin. Psychol. Psychother. 2011;18(3):250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- Rigby H., Gubitz G., Phillips S. A systematic review of caregiver burden following stroke. Int. J. Stroke. 2009;4(4):285–292. doi: 10.1111/j.1747-4949.2009.00289.x. [DOI] [PubMed] [Google Scholar]
- Riksförbund Anhörigas. Information till dig som anhörig/anhörigvårdgivare. 2016. http://media.anhorigasriksforbund.se/2016/04/Blad-andra-språk-svenska.pdf Available:
- Rockliff H., Gilbert P., McEwan K., Lightman S., Glover D. A pilot exploration of heart rate variability and salivary cortisol responses to compassion-focused imagery. J. Clin. Neuropsychiatry. 2008;5(3):132–139. [Google Scholar]
- Sauro J. 2011. A Practical Guide to the System Usability Scale: Background, Benchmarks & Best Practices. Measuring Usability LLC. [Google Scholar]
- Savundranayagam M.Y., Montgomery R.J. Impact of role discrepancies on caregiver burden among spouses. Res. Aging. 2010;32(2):175–199. [Google Scholar]
- Schrag A., Hovris A., Morley D., Quinn N., Jahanshahi M. Caregiver-burden in Parkinson's disease is closely associated with psychiatric symptoms, falls, and disability. Parkinsonism Relat. Disord. 2006;12(1):35–41. doi: 10.1016/j.parkreldis.2005.06.011. [DOI] [PubMed] [Google Scholar]
- Schubart J.R., Kinzie M.B., Farace E. Caring for the brain tumor patient: family caregiver burden and unmet needs. Neuro-Oncology. 2008;10(1):61–72. doi: 10.1215/15228517-2007-040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R., Sherwood P.R. Physical and mental health effects of family caregiving. J. Soc. Work. Educ. 2008;44(Suppl. 3):105–113. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal Z.V., Williams J.M.G., Teasdale J.D. Guilford; New York, NY: 2002. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. [Google Scholar]
- Smith L., Onwumere J., Craig T., McManus S., Bebbington P., Kuipers E. Mental and physical illness in caregivers: results from an English national survey sample. Br. J. Psychiatry. 2014;205(3):197–203. doi: 10.1192/bjp.bp.112.125369. [DOI] [PubMed] [Google Scholar]
- Snippe E., Dziak J.J., Lanza S.T., Nyklícek I., Wichers M. The shape of change in perceived stress, negative affect, and stress sensitivity during mindfulness-based stress reduction. Mindfulness. 2017;8(3):728–736. doi: 10.1007/s12671-016-0650-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stjernswärd S., Hansson L. Outcome of a web-based mindfulness intervention for families living with mental illness - a feasibility study. Inform. Health Soc. Care. 2016;42(1):97–108. doi: 10.1080/17538157.2016.1177533. [DOI] [PubMed] [Google Scholar]
- Stjernswärd S., Hansson L. User value and usability of a web-based mindfulness intervention for families living with mental health problems. Health Soc. Care Commun. 2016;25(2):700–709. doi: 10.1111/hsc.12360. [DOI] [PubMed] [Google Scholar]
- Stjernswärd S., Hansson L. Effectiveness and usability of a web-based mindfulness intervention for families living with mental illness. Mindfulness. 2017;8(3):751–764. doi: 10.1007/s12671-016-0653-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turcotte M. 2013. Family Caregiving: What are the Consequences? Statistics Canada/Statistique Canada. Catalogue no. 75-006-X. (ISSN 2291-0840) [Google Scholar]
- Wallmark E., Safarzadeh K., Daukantaitė D., Maddux R.E. Promoting altruism through meditation: an 8-week randomized controlled pilot study. Mindfulness. 2013;4(3):223–234. [Google Scholar]
- Webb T., Joseph J., Yardley L., Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J. Med. Internet Res. 2010;12(1) doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadavaia J.E., Hayes S.C., Vilardaga R. Using acceptance and commitment therapy to increase self-compassion: a randomized controlled trial. J. Context. Behav. Sci. 2014;3(4):248–257. doi: 10.1016/j.jcbs.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan F., Johnson S.K., Diamond B.J., David Z., Goolkasian P. Mindfulness meditation improves cognition: evidence of brief mental training. Conscious. Cogn. 2010;19(2):597–605. doi: 10.1016/j.concog.2010.03.014. [DOI] [PubMed] [Google Scholar]