Abstract
Intravenous (IV) push administration can provide clinical and practical advantages over longer IV infusions in multiple clinical scenarios, including in the emergency department, in fluid-restricted patients, and when supplies of diluents are limited. In these settings, conversion to IV push administration may provide a solution. This review compiles available data on IV push administration of antibiotics in adults, including preparation, stability, and administration instructions. Prescribing information, multiple tertiary drug resources, and primary literature were consulted to compile relevant data. Several antibiotics are Food and Drug Administration–approved for IV push administration, including many beta-lactams. In addition, cefepime, ceftriaxone, ertapenem, gentamicin, and tobramycin have primary literature data to support IV push administration. While amikacin, ciprofloxacin, imipenem/cilastatin, and metronidazole have limited primary literature data on IV push administration, available data do not support that route. In addition, a discussion on practical considerations, such as IV push best practices and pharmacodynamic considerations, is provided.
Keywords: anti-infectives, drug stability, intravenous therapy
Introduction
Antibiotics are commonly administered intravenous (IV) medications. Many of these drugs can be administered via IV push, intermittent IV infusion, and/or continuous IV infusion, depending on the medication. IV push allows for administration of an antibiotic in a minimal fluid volume. Small fluid volumes can be particularly useful in patients who are fluid-restricted, such as patients with acute volume overload or acute renal failure.1 In addition, the faster administration time may provide advantages in the emergency department (ED), so that time-to-first-dose can be shortened.2,3 There may also be interest in IV push administration in the setting of drug or fluid shortages, such as the current shortage of small volume parenteral (SVP) solutions (ie, 50 or 100 mL bags for intermittent IV infusion).4 In response, the American Society of Health-Systems Pharmacists recommends switching medication administration to IV push when possible to help conserve SVP supplies in the context of a shortage. Therefore, the purpose of this article is to summarize the available data that support IV push administration of antibiotics in adults.
Methods
A list of commercially available injectable antibiotics was generated from The Sanford Guide and the Food and Drug Administration (FDA) Orange Book.5,6 The prescribing information (PI) was used as the primary resource for FDA-approved routes of administration and stability data.7-59 The PIs for vials for reconstitution were selected if available because vial formulations are most readily prepared for IV push administration. Additional tertiary drug resources were used to confirm the information found in the PI and provide additional data, if available.60-66 Primary literature citations from tertiary sources were reviewed in their full-text form. A primary literature search was also performed of the MEDLINE and International Pharmaceutical Abstracts (IPA) databases. Each drug name was paired with the following terms to capture published data on IV push administration: intravenous, inject*, parenteral*, “administration and dosage”[MeSH Subheading], push, bolus, rapid, fast. All sources were consulted for each drug to ascertain consensus recommendations; in cases when information could only be located in one source, a note is included in the comment column of Table 1 or in the text summaries for the antibiotics.
Table 1.
| Antibiotic | FDA-approved administration | IV push/IV slow injection |
Notes | ||
|---|---|---|---|---|---|
| Preparation | Stabilityb | Administration | |||
| Aminoglycosides | |||||
| Gentamicin | Intermittent IV infusion IM Not approved for IV push administration |
Off-label preparation Loewenthal 201067: Dilute doses <800 mg to 20 mL with NS; larger doses administered as 40 mg/mL solution supplied in manufacturer’s vials Mendelson 197668: Dilute dose in 50-mL D5W or NS (most patients received 120-mg doses) Meunier 198769: 80 mg prediluted in 2-mL NS (40 mg/mL) Scott 198970: Dilute doses to 20 mL with NS (doses were 6 mg/kg/d in divided doses or 2 mg/kg/dose) |
Polypropylene syringe, 40 mg/mL63,71: 30 d at 4°C or
25°C Plastic syringe, 40 mg/mL63,72: average loss of 16% after 30 d and brown precipitate formed at both 4°C and 25°C Glass syringe, 40 mg/mL63,72: average loss of 7% after 30 d, brown precipitate formed at 60 d at both 4°C and 25°C Possible instability with storage in plastic packaging due to potential oxygen exposure63,73 |
Off-label administration Loewenthal 201067: Inject over 3 to 5 min Mendelson 197668: Inject over 3 to 5 min using Soluset system Meunier 198769: Inject over <1 min Scott 198970: Inject over 5 min |
Loewenthal 201067: Described IV push administration of gentamicin and
tobramycin in OPAT setting, report of 5593 doses Mendelson 197668: Compared IV push with 2 h infusion in 63 patients with various infections Meunier 198769: PK study in 10 healthy volunteers that compared IV push with slow IV injection (same dose diluted in 100 mL given over 15 min); authors endorsed slow IV injection administration based on PK parameters (IV push resulted in high peak serum concentrations) Scott 19892: PK study in 19 patients and 2 healthy volunteers that compared IV push with IM administration Refer to text for additional data with IV push |
| Tobramycin | Intermittent IV infusion IM Not approved for IV push administration |
Off-label preparation Loewenthal 201067: Dilute doses <800 mg to 20 mL with NS; larger doses administered as 40 mg/mL solution supplied in manufacturer’s vials Aoyama 198774: 2 mg/kg dose diluted in 10-mL D5W |
Plastic syringe, 40 mg/mL solution from reconstituted 1.2-g vial63,75: after 2 mo, no significant change in concentration detected at 4°C and 25°C |
Off-label administration Loewenthal 201067: Inject over 3 to 5 min Aoyama 198774: IV push, administration time not reported; Injected within 2 to 3 min of preparation |
Loewenthal 201067: Described IV push administration of gentamicin and
tobramycin in OPAT setting, report of 5593 doses Aoyama 198774: Evaluated different routes of tobramycin administration in 21 burn patients, included IV push (5 patients) Refer to text for additional data with IV push |
| Carbapenems | |||||
| Ertapenem | Intermittent IV infusion IM Not approved for IV push administration |
Off-label preparation Wiskirchen 201376: Dilute 1 g dose in NS to a total volume of 10 mL (100 mg/mL) |
Wiskirchen 201376: Prepared doses used within 6 h of reconstitution; stored under refrigeration until administered Polypropylene syringes, 100 mg/mL in NS63,77: 30 min at RT, 24 h under refrigeration followed by 4 h at RT, 14 d frozen followed by 5 h at RT, or 28 d frozen followed by 3 h at RT |
Off-label administration Wiskirchen 201376: Inject over 5 min, at a rate of 2 mL/min through peripheral IV catheter |
Wiskirchen 201376: Evaluated IV push administration in a PK study of 12 healthy volunteers; did not specifically evaluate stability |
| Meropenem | IV push Intermittent IV infusion |
Vials of 500 mg or 1 g: reconstitute with 10-mL and 20-mL SWFI, respectively, to
a resulting concentration of 50 mg/mL No further dilution required |
Reconstituted vial: 3 h at 25°C and 13 h at 5°C Plastic luer-tip syringes with tubing attached and capped, 50 mg/mL in SWFI64: 8 h at RT and 44 h under refrigeration |
Inject over 3 to 5 min (adults and children ≥3 months) Children <3 months should receive IV infusion over 30 min |
|
| Cephalosporins | |||||
| Cefazolin | IV push Intermittent IV infusion IM |
Vials of 500 mg or 1 g: reconstitute with 2- and 2.5-mL SWFI to resulting
concentrations of 225 and 330 mg/mL, respectively Further dilute reconstituted solution with approximately 5 mL of SWFI for IV push administration Off-label preparation McLaughlin 2017, Poole 1999, Garrelts 19882,78,79: 1 or 2 g diluted with 10-mL SWFI |
Reconstituted vial: 24 h at RT and 10 d under refrigeration Extended stability data63: 500 mg diluted in 2 mL of SWFI80: 4 d at 25°C Plastic syringes, 100 and 200 mg/mL in SWFI81: 13 d at 24°C, 28 d at 4°C, 3 mo when frozen at −15°C (time to 10% loss) Polypropylene syringes, 100 and 200 mg/mL in SWFI82: 30 d at 5°C with light protection, followed by 72 h at 21 to 25°C with light exposure |
Inject over 3 to 5 min, directly into vein or through the tubing of a running
compatible IV infusion Off-label administration McLaughlin 20172: Inject over 2 min Poole 199979: Inject over 3 to 5 min Garrelts 198878: Inject over 1 to 2 min/g |
McLaughlin 20172: Evaluated use of IV push for first dose only in ED Poole 199979: Evaluated IV push for patient-administered doses at home (OPAT) Garrelts 198878: Evaluated rates of postinfusion phlebitis with IV push compared with IV infusion in a tertiary hospital |
| Cefepime | Intermittent IV infusion IM Not approved for IV push administration |
Off-label preparation Tran 20173: 1- and 2-g doses diluted in NS to a total volume of 10 mL McLaughlin 20172: 1- and 2-g doses diluted in 10 and 20 mL of SWFI, respectively |
Reconstituted solutions in compatible solutions: 24 h at 20 to 25°C and 7 d at 2
to 8°C (see PI for further details) Polypropylene syringes, 100 and 200 mg/mL in D5W, NS, or SWFI63,83,84: 14 d at 4°C, 1 d at RT, and up to 90 d at –20°C |
Off-label administration Tran 20173: Inject over 2 to 5 min McLaughlin 20172: Inject over 5 min |
Tran 2017 and McLaughlin 20172,3: Evaluated use of IV push for
first dose only in ED An additional study85 evaluated 2 g over 3, 5, 10, and 15 min in healthy volunteers; however, concentration was 40 mg/mL (total volume, 50 mL) |
| Cefotaxime | IV push Intermittent IV infusion IM |
Vials of 500 mg, 1 g, and 2 g: reconstitute with 10-mL SWFI to resulting
concentrations of 50, 95, and 180 mg/mL, respectively No further dilution required Maximum concentration for IV push is 200 mg/mL in SWFI65 |
Reconstituted vial: 24 h at RT, 7 d under refrigeration, and 13 wk frozen for
500-mg and 1-g vials; 12 h at RT, 7 d under refrigeration, and 13 wk frozen for
2-g vial Plastic syringe, reconstituted solutions for IV push: 5 d under refrigeration and 13 wk frozen |
Inject over 3 to 5 min Can be given directly into vein or through the tubing of a running compatible IV infusion60,63 |
Do not administer over <3 min; injection over <1 min through a central
venous catheter has resulted in life-threatening arrhythmias Maximum IV push concentration only reported in Pediatric Injectable Drugs text |
| Cefotetan | IV push Intermittent IV infusion IM |
Vials of 1 and 2 g: reconstitute with 10-mL and 10- to 20-mL SWFI to resulting
concentrations of 95 mg/mL and 95 or 182 mg/mL, respectively No further dilution required |
Reconstituted vial: 24 h at 25°C, 96 h at 5°C, and 1 wk at -20°C Plastic or glass syringes, reconstituted solutions for IV push: 24 h at 25°C and 96 h at 5°C |
Inject over 3 to 5 min | |
| Cefoxitin | IV push Intermittent IV infusion |
Vials of 1 and 2 g: reconstitute with 10-mL SWFI to resulting concentrations of
95 mg/mL and 180 mg/mL, respectively No further dilution required |
Reconstituted vials with 1 g/10 mL concentration: 6 h at RT and 1 wk under
refrigeration, for all compatible diluents Plastic syringes, 1 and 2 g diluted in 10 mL of SWFI63,81: 2 d at 24°C, 23 d at 4°C, 3 mo frozen at −15°C (time to 10% loss) |
Inject over 3 to 5 min, directly into vein or through the tubing of a running
compatible IV infusion Off-label administration McLaughlin 20172: Inject 1 g dose over 2 min and 2 g dose over 5 min Garrelts 198878: Inject over 1 to 2 min/g |
McLaughlin 20172: evaluated use of IV push for first dose only in ED; both 1 and
2 g doses were diluted in 10 mL SWFI Garrelts 198878: Evaluated rates of postinfusion phlebitis with IV push compared with IV infusion in a tertiary hospital; 1 g dose diluted in 10 mL SWFI |
| Ceftazidime | IV push Intermittent IV infusion IM |
Fortaz vials of 500 mg, 1 g or 2 g: reconstitute with 5.3-, 10-, and 10-mL SWFI
to resulting concentrations of 100, 100, and 170 mg/mL,
respectively Tazicef vials of 1 or 2 g: reconstitute with 10-mL SWFI to concentrations of 95 and 180 mg/mL, respectively No further dilution required Off-label preparation McLaughlin 20172: 1 or 2 g diluted with 10 or 20 mL SWFI, respectively |
Reconstituted vials for Fortaz (all sizes): 12 h at RT or 3 d under
refrigeration; reconstituted solution in original container may be frozen for 3 mo
at –20°C Reconstituted vials for Tazicef (all sizes): 24 h at RT or 7 d under refrigeration; reconstituted solution in original container may be frozen for 3 mo at –20°C Polypropylene syringes, 100 and 200 mg/mL in SWFI (Fortaz)63,86: 8 h at 22°C, 96 h at 4°C, and 91 d at –20°C |
Inject over 3 to 5 min, directly into vein or through the tubing of a running
compatible IV infusion Off-label administration McLaughlin 20172: Inject over 5 min Garrelts 198878: Inject over 1 to 2 min/g |
McLaughlin 20172: Evaluated use of IV push for first dose only in
ED Garrelts 198878: Evaluated rates of postinfusion phlebitis with IV push compared with IV infusion in a tertiary hospital; 1 g diluted in 10 mL SWFI Specific formulation of ceftazidime in Studies 1 and 2 not reported |
| Ceftriaxone | Intermittent IV infusion IM Not approved for IV push administration |
PI reconstitution Vials of 250 mg, 500 mg, 1 g, and 2 g: reconstitute with 2.4-, 4.8-, 9.6-, and 19.2-mL SWFI, NS, or D5W, respectively, to a resulting concentration of 100 mg/mL (PI recommends further dilution for administration via IV infusion) Off-label preparation McLaughlin 20172: 1 and 2 g diluted in 10 mL SWFI Poole 199979: 1 g diluted in 10 mL SWFI Garrelts 198878: 1 g diluted in 10 mL SWFI |
Reconstituted vials (100 mg/mL): 2 d at 25°C and 10 d at
4°C Polypropylene syringes, 100 mg/mL in SWFI63,87: 72 h at 20°C; 40 d at 4°C, and 180 d frozen at –20°C |
Off-label administration McLaughlin 20172: Inject over 2 min (adults only) Poole 199979: Inject over 2 to 4 min in those aged >11 years Garrelts 198878: Inject over 1 to 2 min/g (adults only) |
McLaughlin 20172: Evaluated use of IV push for first dose only in ED Poole 199979: Evaluated IV push for patient-administered doses at home (OPAT) Garrelts 198878: Evaluated rates of postinfusion phlebitis with IV push compared with IV infusion in a tertiary hospital |
| Cefuroxime | IV push Intermittent IV infusion Continuous IV infusion IM |
Vials 750 mg and 1.5 g: reconstitute with 8.3- and 16-mL SWFI, respectively, to
a resulting concentration of 90 mg/mL No further dilution required Off-label preparation Poole 1999 and Garrelts 198878,79: 750 mg diluted with 10 mL SWFI |
Reconstituted vials: 24 h at RT and 48 h under refrigeration | Inject over 3 to 5 min, directly into vein or through the tubing of a running
compatible IV infusion Off-label administration Garrelts 198878: Inject over 1 to 2 min/g |
Poole 199979: Evaluated IV push for patient-administered doses at home
(OPAT); over 3 to 5 min Garrelts 198878: Evaluated rates of postinfusion phlebitis with IV push compared with IV infusion in a tertiary hospital No relevant syringe stability was located |
| Glycopeptides/lipoglycopeptides/lipopeptides | |||||
| Daptomycin | IV push (adults only) Intermittent IV infusion (adults and pediatric patients aged 1 to 17 years) |
Cubicin Cubicin vials: reconstitute with 10 mL of NS to concentration of 50 mg/mL No further dilution required Cubicin RF Cubicin RF vials: reconstitute with 10 mL of SWFI or BWFI to concentration of 50 mg/mL No further dilution required |
Cubicin Reconstituted Cubicin vials: 12 h at RT and 48 h under refrigeration Cubicin RF Reconstituted Cubicin RF vials: 24 and 48 h at RT in SWFI and BWFI, respectively; 3 d under refrigeration in both SWFI and BWFI Polypropylene syringes (with elastomeric rubber stopper), 50 mg/mL (Cubicin RF): 24 h and 3 d at RT and under refrigeration, respectively, when diluted with SWFI; 48 h and 5 d at RT and under refrigeration, respectively, when diluted with BWFI |
Cubicin and Cubicin RF Inject over 2 min |
Cubicin and Cubicin RF Do not administer by IV push in pediatric and adolescent patients aged ≤17 years. 2 formulations are available (Cubicin and Cubicin RF), which have differences in reconstitution and storage Cubicin No relevant syringe stability for Cubicin formulation was located Cubicin RF Do not use saline-based diluents to reconstitute Cubicin RF; this results in hyperosmotic solution that may cause infusion-site reactions when given as IV push |
| Monobactam | |||||
| Aztreonam | IV push Intermittent IV infusion IM |
Vials of 1 and 2 g: reconstitute with 6- to 10-mL SWFI No further dilution required |
Reconstituted solutions >20 mg/mL in SWFI: 48 h at RT and 7 d under refrigeration | Inject over 3 to 5 min, directly into vein or through the tubing of a running compatible IV infusion | No relevant syringe stability was located |
| Others | |||||
| Chloramphenicol | IV push | Vials of 1 g: reconstitute with 10 mL of SWFI or D5W to resulting concentration
of 100 mg/mL No further dilution required |
Reconstituted vial62,63: 30 d at RT | Inject over at least 1 min | No relevant syringe stability was located |
| Penicillins | |||||
| Ampicillin | IV push Slow IV injection IM |
Vials of 125, 250, and 500 mg: reconstitute with 5-mL SWFI or BWFI Vials of 1 and 2 g: reconstitute with 7.4 or 14.8 mL, respectively, SWFI or BWFI No further dilution required |
IM and IV push injections should be administered within 1 h after reconstitution
as potency may decrease Additional stability information in text summary |
Inject over 3 to 5 min for 125-, 250-, and 500-mg doses Inject over 10 to 15 min for 1- and 2-g doses |
Administration of ampicillin more rapidly than recommended may result in
convulsive seizuresc No relevant syringe stability was located |
| Ampicillin/sulbactam | Slow IV injection Intermittent IV infusion IM |
Vials of 1.5 and 3.0 g: Reconstitute with 3.2 or 6.4 mL of SWFI, respectively,
to a concentration of 250 mg ampicillin/mL Further dilute with suitable diluent to a final concentration of 30 mg ampicillin/mL (maximum concentration for IV administration) |
Reconstituted solution (30 mg ampicillin/mL), in SWFI or NS: 8 h at 25ºC and 48 h at 4ºC | Inject over at least 10 to 15 min | See PI for detailed information on stability for various diluents and storage
conditions No relevant syringe stability was located |
| Nafcillin | Slow IV injection Intermittent IV infusion IM |
Vials of 1 or 2 g: reconstitute, respectively, with 3.4 or 6.6 mL SWFI, NS, or
BWFI (with benzyl alcohol or parabens) to final concentration of 250
mg/mL Further dilute reconstituted solution with at least 15 to 30 mL SWFI, NS, or ½ NS Off-label preparation Poole 199979: 1 g diluted with 25 mL NS (for central line administration only) |
Initial reconstituted solution (250 mg/mL): 3 d at RT, 7 d under refrigeration,
and 90 d frozen Stability of further diluted solutions: 10 to 200 mg/mL: 24 h at RT and 7 d under refrigeration, in SWFI and NS |
Inject over 5 to 10 min, recommended to be given through the tubing of a running compatible IV infusion | Poole 199979: Evaluated IV push for patient-administered dose at home
(OPAT); given over 5 to 10 min No relevant syringe stability was located |
| Oxacillin | Slow IV injection Intermittent IV infusion IM |
Vials of 1 and 2 g: Reconstitute with 10 or 20 mL, respectively, of SWFI, ½ NS,
or NS to 100 mg/mL No further dilution required |
Reconstituted solution (10-100 mg/mL): 4 d at RT and 7 d under refrigeration, in
SWFI and NS Reconstituted solution (100 mg/mL): 30 d frozen in SWFI and NS (for SWFI, includes 50-100 mg/mL) Plastic luer-tip syringes with tubing attached and capped, 100 mg/mL in NS64: 92 h at RT and 2 wk under refrigeration |
Inject over 10 min | |
| Polymyxins | |||||
| Colistimethate sodium | IV push IV continuous infusion IM injection |
150 mg vial: reconstitute with 2 mL SWFI to resulting concentration of 75
mg/mL No further dilution required |
Reconstituted vial: 7 d at refrigerated (2°-8°C) or RT (20°-25°C) | Inject over 3 to 5 min | See text summary for additional stability information No relevant syringe stability was located |
Note. FDA = Food and Drug Administration; ½ NS = half-normal saline (0.45% sodium chloride); D5W = dextrose 5% in water; OPAT = outpatient parenteral antibiotic therapy; ED = emergency department; IM = intramuscular; IV = intravenous; NS = normal saline (0.9% sodium chloride); PI = prescribing information; PK = pharmacokinetic; RT = room temperature; SWFI = sterile water for injection; BWFI = bacteriostatic water for injection; USP = United States Pharmacopeia.
Information sourced from PI unless otherwise noted.
For assigning beyond use dates, in addition to stability data, USP <797> recommendations for sterility still apply. The shorter of the times should be used.
Clinical Pharmacology reported 100 mg/min as maximum rate; however, this information could not be confirmed in additional resources. In addition, this rate is slower than what would be administered if following PI-recommended dilution and administration.
Table 1 provides a summary of antibiotics that can be administered IV push. Stability data are limited to solutions (eg, concentrations, diluents) that can be used for IV push administration. Because there is no exact definition of IV push and a wide range of administration durations were considered IV push in the original sources, Table 1 separates administration recommendations into 2 categories. Administration over 5 minutes or less are listed as IV push, while administration over longer durations of time (eg, over 5-10 minutes) are listed as slow IV injection; however, specific administration times are provided. Figure 1 lists antibiotics that had no data or limited data suggesting IV push as a viable administration method; therefore, these antibiotics are excluded from Table 1.
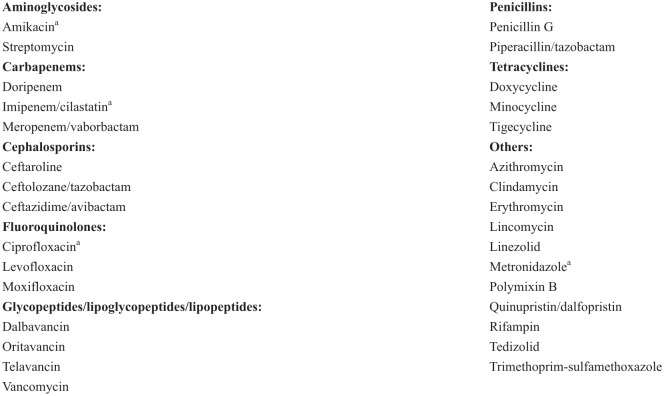
Figure 1.
Antibiotics with limited or no data for IV push administration. See the text summaries for each drug class for further information.
aLimited data available, not recommended for IV push administration.
Aminoglycosides
None of the aminoglycosides are indicated for IV push administration.7-9,46 Aminoglycosides are generally not recommended for IV push administration due to the concern that elevated peak levels after rapid administration may cause toxicity, such as ototoxicity.9,65,88 Specifically, the PI for tobramycin notes that peak serum levels may exceed 12 μg/mL when administered over periods <20 minutes.9
However, IV push administration of gentamicin and tobramycin has been reported frequently in primary literature.89-100 Table 1 includes a summary of studies with sufficient detail to replicate administration, including a descriptive report demonstrating that gentamicin and tobramycin can be safely administered IV push based on experience with 5593 doses in the setting of outpatient parenteral antibiotic therapy (OPAT).67 In addition to the studies cited in Table 1, gentamicin has reportedly been administered over time periods ranging from <10 seconds to 5 minutes,89-91,93-96 while tobramycin has been administered over time periods ranging from 15 seconds to 5 minutes.89,90,96-101 Most administration times for gentamicin and tobramycin ranged from approximately 3 to 5 minutes. These studies were of varying quality and instructions for preparation were not described. There are limited reports of IV push administration with amikacin; one healthy volunteer study (n = 5) evaluated administration of 7.5 mg/kg directly from the manufacturer vial (250 mg/mL) over 2 minutes, but this resulted in potentially toxic peak serum concentrations (68-122 μg/mL).102 Amikacin has been administered over 3 minutes and 5 minutes, respectively, in 2 additional pharmacokinetic studies; however, dilution and preparation instructions were not reported.103,104 Reports of streptomycin administered via IV push were not identified.
Carbapenems
Of the carbapenems, only meropenem is FDA- approved to be administered IV push.11 Doripenem and meropenem/vaborbactam should only be given via intermittent IV infusion; no data are available to support IV push administration.35,37 One pharmacokinetic study was identified describing administration of imipenem/cilastatin 500 mg over 10 minutes in 6 patients undergoing continuous ambulatory peritoneal dialysis; the volume/concentration of the administered solution was not provided.105 However, IV push administration of imipenem/cilastatin is not recommended due to adverse events associated with rapid administration, such as nausea and vomiting.61,66 Administration of ertapenem 1 gram IV push over 5 minutes was bioequivalent to the 30-minute infusion for maximum serum concentration (Cmax) and area under the curve (AUC) in a study in 12 healthy volunteers, and no serious adverse events, such as vomiting or seizures, occurred (Table 1).76
Cephalosporins
Cefazolin, cefotaxime, cefotetan, cefoxitin, ceftazidime, and cefuroxime are FDA-approved for IV push administration.12,14-18,20 Studies comparing IV push and short-term infusion administration of cephalosporins have generally found similar rates of phlebitis and other complications.78,79,106 Although not FDA-approved, cefepime and ceftriaxone may also be administered IV push.2,3,78,79,85 Data for cefepime are limited to use as the first-dose in the ED, with limited outcome and adverse event data provided in reports.2,3 One additional study evaluated cefepime administered IV push, but the required volume for preparation was 50 mL, losing volume minimization advantages of IV push.85 Ceftriaxone IV push administration has been evaluated in several settings, including in the ED, with OPAT, and in hospitalized patients, with no noted concerns.2,78,79 Additional data on ceftriaxone IV push administration exist, but the majority of studies did not robustly report both preparation and administration details or focused solely on pediatric populations.107-109 Only 3 cephalosporins lack information for IV push administration: ceftazidime/avibactam, ceftolozane/tazobactam, and ceftaroline.
Specific adverse events related to IV push administration of cefotaxime and ceftriaxone are noted in the literature. A potentially life-threatening arrhythmia occurred in 6 patients who received rapid (<1 minute) administration of cefotaxime through a central venous catheter.14 Rapid ceftriaxone administration (2 grams over 5 minutes) was associated with a case of palpitation, tachycardia, restlessness, shivering, and diaphoresis in an adult.110 Ceftriaxone has also been reported to be associated with increased biliary pseudolithiasis in children given ceftriaxone over 3 to 5 minutes, and with the formation of calcium-ceftriaxone precipitate in neonates receiving concurrent calcium-containing solutions who received ceftriaxone over 2 to 4 minutes, which led to adverse cardiopulmonary events.111,112
Glycopeptides/Lipoglycopeptides/Lipopeptides
Daptomycin (both Cubicin and Cubicin RF) may be administered IV push in adults when reconstituted to a concentration of 50 mg/mL.21,22 While this practice has been reported to be safe in adults,113-115 a case report exists documenting an IV push-related reaction to daptomycin (Cubicin) administered over 2 minutes involving redness and a warm sensation on the face, neck, and upper chest that resolved with diphenhydramine and did not recur with rechallenge of a 30- to 40-minute infusion.116 The newer agents of these classes are not amenable to IV push administration; dalbavancin, oritavancin, and telavancin are administered via extended infusions ranging from 1 to 3 hours, and no recent literature reports their administration over shorter periods.38-40 Vancomycin, because of the risk for infusion reaction (ie, “red-man syndrome”), should be administered no more rapidly than 10 mg/minute or over a period of ≥60 minutes, whichever is longer.60,61,65,66 Infusion reactions can be mediated by both the concentration and rate of administration of vancomycin. For patients in need of fluid restriction, vancomycin may be administered at concentrations up to 10 mg/mL, though this may increase the risk for infusion reaction.
Fluoroquinolones
Fluoroquinolones (ciprofloxacin, levofloxacin, and moxifloxacin) are not recommended for IV push administration due to adverse events associated with rapid administration.57-59,61,66 These adverse events include venous irritation with ciprofloxacin, hypotension with levofloxacin, and an increase in the incidence and magnitude of QT prolongation with moxifloxacin. In addition, moxifloxacin is only available in premix formulations intended for intermittent IV infusion.6,58 In order to reduce venous irritation, slow IV infusion of ciprofloxacin into a large vein is recommended.59 Although reports of ciprofloxacin administration over a period ranging from 3 to 15 minutes were identified, these studies did not specifically aim to evaluate the safety and efficacy of the IV push administration.117-119 In 2 pharmacokinetic studies in healthy volunteers, ciprofloxacin was administered via rapid injection over 3 or 5 minutes, but the volume and concentration of the administered solutions were not specified.117,118 In one of these studies, observed adverse events with administration of ciprofloxacin 250 mg over 5 minutes in 8 healthy volunteers included localized numbness (n = 1), local thrombophlebitis (n = 1), and nausea (n = 1).117 In another study in 12 healthy volunteers, ciprofloxacin 50 mg and 100 mg was prepared in 50 mL normal saline and administered over 15 minutes with a constant pump, with no observed adverse events.119 However, these doses are lower than those commonly used in clinical practice.60
Penicillins and Monobactam
Among the penicillins, ampicillin may be administered IV push or as a slow IV injection after reconstitution, depending on the dose.26 Administration faster than recommended by the PI may increase the risk of seizures.26,60,65 In addition, ampicillin has limited stability, which decreases with increasing concentrations.63 Nafcillin and oxacillin require administration via slow IV injection (eg, over 5-10 minutes).28,29 Phlebitis may occur if these agents are injected too rapidly.60 Of note, profound hypotension has been reported among patients receiving IV push administration of nafcillin during coronary artery bypass graft surgery, presumed to be due to histamine-mediated vasodilation.120 Penicillin G and piperacillin/tazobactam are not recommended for IV push administration. Ampicillin/sulbactam is recommended to be diluted in volumes that may preclude practical administration via slow IV injection (eg, 1.5 g vials in 50 mL to obtain maximum 30 mg/mL concentration).27 Although a study in 16 patients undergoing colorectal surgery reported IV push administration of 2 g/1 g ampicillin/sulbactam over 3 minutes, the concentration of the solution was not reported.121 Similarly to ampicillin, seizures may occur with rapid administration of ampicillin/sulbactam.66 Finally, the monobactam aztreonam is indicated for IV push administration after reconstitution of vials.23
Polymyxins
Colistimethate sodium can be administered IV push.25 After reconstitution, the manufacturer recommends use within 7 days. However, colistimethate sodium can hydrolyze to colistin in aqueous solution. Although this conversion was minimally observed in one stability study (<1% after storage of reconstituted solution at 4° or 25°C for 7 d in the dark), the authors cautioned that reconstitution should still be done as close to administration as possible, and if it is necessary to store the solution, they recommend storage at 4°C to minimize bacterial contamination.122 With regard to the safety of IV push administration, 1 patient out of 12 in a trial assessing the safety and tolerability of IV push colistimethate reported dizziness/lack of coordination after receiving 160 mg in 10 mL over 5 minutes.123 This resolved when the patient was switched to an intermittent IV infusion over 30 minutes. Polymyxin B is FDA-approved to be given as an IV infusion, intramuscularly, or intrathecally.45 Administration of polymyxin B over a period <30 minutes is not recommended, and rapid IV injections should be avoided due to the potential for nephro- or neurotoxicity.62,124
Tetracyclines
Doxycycline, minocycline, and tigecycline are recommended to be administered as an intermittent IV infusion and are not suitable for IV push administration.42-44 The PIs for doxycycline and minocycline specifically state that rapid administration is not recommended, and oral administration is preferred over parenteral administration.42,43 Phlebitis and burning have been observed with more concentrated solutions of doxycycline.65,125
Others
Of the antibiotics that are not included in the classes already discussed, only chloramphenicol can be administered IV push.24 All of the other agents have specific statements against IV push administration in at least one tertiary resource.60-63,65,66 Of note, Seifert and colleagues documented a report of severe nausea, cramping, and hypotension after administration of erythromycin 1 g in 100 mL of normal saline over 10 minutes.126 In addition, Aucoin and colleagues reported a case of complete heart block following administration of clindamycin 600 mg over several minutes; the same patient tolerated subsequent clindamycin infusions over 30 minutes without incident.127 Rapid lincomycin administration has also been associated with severe cardiac events including cardiopulmonary arrest.128
Linezolid and metronidazole are not available in a vial formulation so these drugs are not practical to administer IV push.6,51,52 One observational pharmacokinetic study documented rapid IV push of metronidazole 500 mg over 5 minutes, but the volume/concentration of the administered solution was not specified so these data are not readily applicable to current clinical practice.129
Practical Considerations for IV Push Antibiotics
Several organizations have issued guidance or recommendations for safe IV administration practices.130 The Institute for Safe Medication Practices (ISMP) provides guidance on adult IV push medication safety.131 Briefly, this guidance supports preparation of IV push medications in the pharmacy so that a ready-to-administer form can be provided to patient care areas. In cases where immediate administration is required for medication stability, preparation and dilution of the medication can occur in patient care areas. In those instances, dilution should take place in a clean, uncluttered area with clear instructions on the type and volume of diluent that is needed. Syringes should be promptly labeled; supplying blank, ready-to-apply labels may help with adherence to that step. Considerations for safe administration of IV push medications can be found in the ISMP guidance document. The 2016 Infusion Nurses Society (INS) Infusion Therapy Standards of Practice largely mirror the ISMP recommendations for safe preparation of medications for IV push administration.132
Osmolality is a concern when administering concentrated solutions. The 2016 INS Infusion Therapy Standards of Practice state that solutions with osmolality >900 mOsm/kg should be administered through a central line and solutions with osmolalities below this limit can be administered via peripheral or midline catheters.132 The Standards of Practice do not have any statements that connect osmolality and administration rate; therefore, there does not seem to be any added concern with IV push administration of solutions with higher osmolalities compared with slower administration rates. Osmolality data is not readily available in product labeling or other tertiary resources and most published osmolality values are based on historical literature that is not readily applicable to current practice.1,78,133-135 With the limitation that not all agents have relevant data, our review of all available published and unpublished (manufacturer-supplied) osmolality information for the antibiotics that can be administered IV push suggests that the recommended solutions for IV push administration all have osmolalities well below 900 mOsm/kg.
Additional steps that help ensure safe use of IV push medications include providing a specific administration duration on the label or in the electronic medication administration record (eg, “administer over 10 minutes” rather than “slow IV injection”).131 Nurse education on proper dilution of IV push medications may also facilitate proper preparation. A 2014 ISMP survey found that 83% of nurse respondents further dilute certain IV push medications prior to administration.136 Unnecessary dilution of medications can lead to contamination of sterile products, dosing errors, or administration errors. Multidose vials should not be kept in patient care areas per the Centers for Disease Control and Prevention One & Only Campaign, which prevents both inadvertent use in multiple patients and errors related to IV push administration of these solutions.137
Pharmacodynamic Considerations for IV Push Antibiotics
The pharmacodynamic effect of antibiotics can be generalized into either concentration-dependent or time-dependent bactericidal activity.138 For agents that are concentration-dependent, maximizing the AUC per unit of time in relation to the bacterial minimum inhibitory concentration (MIC) generally increases the rapidity of bacterial killing and thus increases the likelihood of a good clinical outcome. For example, daptomycin has concentration-dependent bactericidal activity and a change in the rate of infusion (eg, a 30-minute infusion versus a 5-minute injection) does not significantly affect the resulting AUC. For beta-lactams, increasing the infusion duration can substantially increase the duration of time that the drug concentration remains above the MIC (T > MIC); therefore, changing from an infusion to IV push administration may negatively affect the pharmacodynamics of these agents. One Monte Carlo simulation study and one healthy volunteer pharmacokinetic study have investigated the impact of IV push administration.76,139 Based on these results, 3- to 5-minute IV push injections and 30-minute infusions of aztreonam, cefepime, ertapenem, and meropenem are expected to achieve similar T > MIC profiles.
In contrast, the difference in T > MIC between a 3- to 5-minute IV push injection (or 30-minute infusion) and an extended (eg, over 3 or 4 hours) or continuous infusion can be clinically significant.140 Several studies have found that extended and continuous infusion strategies are associated with improved clinical cure and survival, particularly in severely ill patients, compared with shorter infusion durations.141-143 Therefore, current data do not support the substitution of IV push administration for extended or continuous infusion schemes in patients who are critically ill, immunocompromised, or infected with organisms with MICs at or above the clinical breakpoint for susceptibility (eg, Pseudomonas with a piperacillin/tazobactam MIC of 16 μg/mL).
Conclusion
Several antibiotics, particularly in the cephalosporin class, are FDA-approved for IV push or slow IV injection administration. In addition, there are primary literature data that support IV push administration of cefepime, ceftriaxone, ertapenem, gentamicin, and tobramycin. Syringe stability data are not available for all antibiotics, which may preclude IV push administration if preparation in patient care areas for immediate use is not possible. Precautions should be taken to ensure safe IV push administration, including clear labeling and staff education. Pharmacodynamic changes due to IV push administration should be considered, including effects on time above MIC when administering antibiotics via IV push that are normally administered as extended or continuous infusions.
Acknowledgments
The authors gratefully acknowledge Jack Rasmussen, PharmD candidate, for his support in data collection.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Samantha Spencer  https://orcid.org/0000-0002-8496-3554
https://orcid.org/0000-0002-8496-3554
Heather Ipema  https://orcid.org/0000-0002-0981-1358
https://orcid.org/0000-0002-0981-1358
References
- 1. Robinson DC, Cookson TL, Grisafe JA. Concentration guidelines for parenteral antibiotics in fluid-restricted patients. Drug Intell Clin Pharm. 1987;21(12):985–989. [DOI] [PubMed] [Google Scholar]
- 2. McLaughlin JM, Scott RA, Koenig SL, Mueller SW. Intravenous push cephalosporin antibiotics in the emergency department: a practice improvement project. Adv Emerg Nurs J. 2017;39(4):295–299. [DOI] [PubMed] [Google Scholar]
- 3. Tran A, O’Sullivan D, Krawczynski M. Cefepime intravenous push versus intravenous piggyback on time to administration of first-dose vancomycin in the emergency department. J Pharm Pract. 2017:897190017734442. [DOI] [PubMed] [Google Scholar]
- 4. American Society of Health-Systems Pharmacists website. Small-volume parenteral solutions shortages. https://www.ashp.org/Drug-Shortages/Shortage-Resources/Publications/Small-Volume-Parenteral-Solutions-Shortages. Accessed December 16, 2017.
- 5. Gilbert DN, Chambers HF, Eliopoulos GM, Saag MS. The Sanford Guide to Antimicrobial Therapy 2017. 47th ed. Sperryville, VA: Antimicrobial Therapy, Inc; 2017. [Google Scholar]
- 6. Food and Drug Administration website. Orange book: approved drug products with therapeutic equivalence evaluations. https://www.accessdata.fda.gov/scripts/cder/ob/. Accessed December 16, 2017.
- 7. Amikacin sulfate: full prescribing information. Eatontown, NJ: West-ward; 2016. [Google Scholar]
- 8. Gentamicin sulfate: full prescribing information. Lake Forest, IL: Hospira Inc; 2017. [Google Scholar]
- 9. Tobramycin: full prescribing information. North Brunswick, NJ: Claris Lifesciences Inc; 2016. [Google Scholar]
- 10. Invanz (ertapenem): full prescribing information. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2017. [Google Scholar]
- 11. Merrem (meropenem): full prescribing information. Wilming-ton, DE: Astrazeneca Pharmaceuticals Lp; 2016. [Google Scholar]
- 12. Cefazolin: full prescribing information. Weston, FL: Apotex Corp; 2017. [Google Scholar]
- 13. Maxipime (cefepime): full prescribing information. Lake Forest, IL: Hospira Inc; 2017. [Google Scholar]
- 14. Claforan (cefotaxime): full prescribing information. Bridgewater, NJ: Sanofi-Aventis US LLC; 2016. [Google Scholar]
- 15. Cefotan (cefotetan): full prescribing information. Buena, NJ: Teligent Pharma Inc; 2017. [Google Scholar]
- 16. Cefoxitin: full prescribing information. Weston, FL: Apotex Corp; 2017. [Google Scholar]
- 17. Tazicef (ceftazidime): full prescribing information. Lake Forest, IL: Hospira Inc; 2016. [Google Scholar]
- 18. Fortaz (ceftazidime): full prescribing information. Buena, NJ: Teligent Pharma Inc; 2017. [Google Scholar]
- 19. Ceftriaxone: full prescribing information. Weston, FL: Apotex Corp; 2017. [Google Scholar]
- 20. Cefuroxime sodium: full prescribing information. Schaumburg, IL: Sagent Pharmaceuticals; 2016. [Google Scholar]
- 21. Cubicin (daptomycin): full prescribing information. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2017. [Google Scholar]
- 22. Cubicin RF (daptomycin): full prescribing information. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2017. [Google Scholar]
- 23. Azactam (aztreonam): full prescribing information. Princeton, NJ: Bristol-Myers Squibb; 2013. [Google Scholar]
- 24. Chloramphenicol sodium succinate: full prescribing information. Schaumburg, IL: Fresenius Kabi USA LLC; 2016. [Google Scholar]
- 25. Coly-Mycin M (colistimethate): full prescribing information. Chestnut Ridge, NY: Par Pharmaceutical; 2017. [Google Scholar]
- 26. Ampicillin sodium: full prescribing information. Lake Zurich, IL: Fresenius Kabi USA LLC; 2017. [Google Scholar]
- 27. Unasyn (ampicillin and sulbactam): full prescribing information. New York, NY: Pfizer Inc; 2017. [Google Scholar]
- 28. Nafcillin: full prescribing information. Austria: Sandoz GmbH; 2017. [Google Scholar]
- 29. Oxacillin: full prescribing information. Newtown, PA: Renaissance SSA LLC; 2017. [Google Scholar]
- 30. Penicillin G potassium: full prescribing information. Princeton, NJ: Sandoz Inc; 2015. [Google Scholar]
- 31. Zosyn (piperacillin and tazobactam): full prescribing information. Philadelphia, PA: Wyeth Pharmaceuticals Inc; 2017. [Google Scholar]
- 32. Teflaro (ceftaroline): full prescribing information. New York, NY: Forest Pharmaceuticals Inc; 2016. [Google Scholar]
- 33. Zerbaxa (ceftolozane and tazobactam): full prescribing information. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2016. [Google Scholar]
- 34. Avycaz (ceftazidime and avibactam): full prescribing information. Irvine, CA: Allergan USA; 2017. [Google Scholar]
- 35. Doripenem: full prescribing information. Weston, FL: Apotex Corp; 2016. [Google Scholar]
- 36. Primaxin (imipenem and cilastatin): full prescribing information. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2016. [Google Scholar]
- 37. Vabomere (meropenem and vaborbactam): full prescribing information. Parsippany, NJ: The Medicines Company; 2017. [Google Scholar]
- 38. Dalvance (dalbavancin): full prescribing information. Parsippany, NJ: Durata Therapeutics US Limited; 2016. [Google Scholar]
- 39. Orbactive (oritavancin): full prescribing information. Parsippany, NJ: The Medicines Company; 2016. [Google Scholar]
- 40. Vibativ (telavancin): full prescribing information. South San Francisco, CA: Theravance Biopharma US Inc; 2016. [Google Scholar]
- 41. Vancomycin: full prescribing information. Lake Zurich, IL: Fresenius Kabi USA LLC; 2017. [Google Scholar]
- 42. Doxy 100 (doxycycline): full prescribing information. Lake Zurich, IL: Fresenius Kabi USA LLC; 2015. [Google Scholar]
- 43. Minocin (minocycline): full prescribing information. Parsippany, NJ: The Medicines Company; 2015. [Google Scholar]
- 44. Tygacil (tigecycline): full prescribing information. Philadelphia, PA: Wyeth Pharmaceuticals Inc; 201. [Google Scholar]
- 45. Polymyxin B: full prescribing information. Pine Brook, NJ: Alvogen Inc; 2017. [Google Scholar]
- 46. Streptomycin: full prescribing information. Big Flats, NY: X-Gen Pharmaceuticals Inc; 2013. [Google Scholar]
- 47. Zithromax (azithromycin): full prescribing information. New York, NY: Pfizer Inc; 2017. [Google Scholar]
- 48. Cleocin (clindamycin): full prescribing information. New York, NY: Pharmacia and Upjohn Company LLC; 2016. [Google Scholar]
- 49. Erythrocin lactobionate (erythromycin): full prescribing information. Lake Forest, IL: Hospira Inc; 2016. [Google Scholar]
- 50. Lincocin (lincomycin): full prescribing information. New York, NY: Pharmacia and Upjohn Company LLC; 2017. [Google Scholar]
- 51. Zyvox (linezolid): full prescribing information. New York, NY: Pharmacia and Upjohn Company LLC; 2017. [Google Scholar]
- 52. Metronidazole: full prescribing information. Lake Forest, IL: Hospira Inc; 2017. [Google Scholar]
- 53. Synercid (quinupristin and dalfopristin): full prescribing information. New York, NY: Pfizer Laboratories Inc; 2017. [Google Scholar]
- 54. Rifadin (rifampin): full prescribing information. Bridgewater, NJ: Sanofi-Aventis US LLC; 2017. [Google Scholar]
- 55. Sivextro (tedizolid): full prescribing information. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2017. [Google Scholar]
- 56. Sulfamethoxazole and trimethoprim: full prescribing information. Rockford, IL: Mylan Institutional LLC; 2017. [Google Scholar]
- 57. Levofloxacin: full prescribing information. East Windsor, NJ: AuroMedics Pharma LLC; 2017. [Google Scholar]
- 58. Moxifloxacin: full prescribing information. Rockford, IL: Mylan Institutional LLC; 2017. [Google Scholar]
- 59. Ciprofloxacin: full prescribing information. North Brunswick, NJ: Claris Lifesciences Inc; 2016. [Google Scholar]
- 60. Clinical pharmacology [database online].Tampa, FL: Gold Standard Inc; 2017. http://clinicalpharmacology.com/. Accessed December 18, 2017. [Google Scholar]
- 61. LexiComp online [database online].Hudson, OH: Wolters-Kluwer Health; 2017. http://online.lexi.com/lco/action/home. Accessed December 18, 2017. [Google Scholar]
- 62. McEvoy GK, ed. AHFS Drug Information. 2016th ed. Bethesda, MD: American Society of Health-System Pharmacists, Inc; 2016. https://www.medicinescomplete.com/mc/. Accessed December 18, 2017. [Google Scholar]
- 63. McEvoy G. Handbook on Injectable Drugs. 19th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2017. [Google Scholar]
- 64. Bing CD, Nowobilski-Vasilios A. Extended Stability for Parenteral Drugs. 6th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2017. [Google Scholar]
- 65. Phelps SJ, Hagemann TM, Lee KR, Thompson AJ. Pediatric Injectable Drugs. 10th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2013. [Google Scholar]
- 66. Gahart BL, Nazareno AR, Ortega MQ. Gahart’s 2017 Intravenous Medications: A Handbook for Nurses and Health Professionals. 33rd ed. St. Louis, MO: Elsevier, Inc; 2017. [Google Scholar]
- 67. Loewenthal MR, Dobson PM. Tobramycin and gentamicin can safely be given by slow push. J Antimicrob Chemother. 2010;65(9):2049–2050. [DOI] [PubMed] [Google Scholar]
- 68. Mendelson J, Portnoy J, Dick V, Black M. Safety of the bolus administration of gentamicin. Antimicrob Agents Chemother. 1976;9(4):633–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Meunier F, Van der Auwera P, Schmitt H, de Maertelaer V, Klastersky J. Pharmacokinetics of gentamicin after i.v. infusion or iv bolus. J Antimicrob Chemother. 1987;19(2):225–231. [DOI] [PubMed] [Google Scholar]
- 70. Scott DK, Edwards C. Optimization of blood sampling time after intravenous bolus doses of gentamicin. J Clin Pharm Ther. 1989;14(1):61–70. [DOI] [PubMed] [Google Scholar]
- 71. Kresel JJ, Smith AL, Siber GR. Stability of gentamicin in plastic syringes. Am J Hosp Pharm. 1977;34(6):570–575. [PubMed] [Google Scholar]
- 72. Weiner B, McNeely DJ, Kluge RM, Stewart RB. Stability of gentamicin sulfate injection following unit dose repackaging. Am J Hosp Pharm. 1976;33(12):1254–1259. [PubMed] [Google Scholar]
- 73. Chrai SS, Ambrosio TJ. Gentamicin sulfate injection repackaging in syringes. Am J Hosp Pharm. 1977;34(9):920. [PubMed] [Google Scholar]
- 74. Aoyama H, Izawa Y, Nishizaki A, Okuda J. Optimal conditions for injection of tobramycin and cefmenoxime into burn patients. Burns Incl Therm Inj. 1987;13(4):269–276. [DOI] [PubMed] [Google Scholar]
- 75. Seitz DJ, Archambault JR, Kresel JJ, Brinck-Johnsen T. Stability of tobramycin sulfate in plastic syringes. Am J Hosp Pharm. 1980;37(12):1614–1615. [PubMed] [Google Scholar]
- 76. Wiskirchen DE, Housman ST, Quintiliani R, Nicolau DP, Kuti JL. Comparative pharmacokinetics, pharmacodynamics, and tolerability of ertapenem 1 gram/day administered as a rapid 5-minute infusion versus the standard 30-minute infusion in healthy adult volunteers. Pharmacotherapy. 2013;33(3):266–274. [DOI] [PubMed] [Google Scholar]
- 77. Jain JG, Sutherland C, Nicolau DP, Kuti JL. Stability of ertapenem 100 mg/mL in polypropylene syringes stored at 25, 4, and -20 degrees C. Am J Health Syst Pharm. 2014;71(17):1480–1484. [DOI] [PubMed] [Google Scholar]
- 78. Garrelts JC, Ast D, LaRocca J, Smith DF, Jr, Peterie JD. Postinfusion phlebitis after intravenous push versus intravenous piggyback administration of antimicrobial agents. Clin Pharm. 1988;7(10):760–765. [PubMed] [Google Scholar]
- 79. Poole SM, Nowobilski-Vasilios A, Free F. Intravenous push medications in the home. J Intraven Nurs. 1999;22(4):209–215. [PubMed] [Google Scholar]
- 80. Bornstein M, Thomas PN, Coleman DL, Boylan JC. Stability of parenteral solutions of cefazolin sodium. Am J Hosp Pharm. 1974;31(3):296–298. [PubMed] [Google Scholar]
- 81. Borst DL, Sesin GP, Cersosimo RJ. Stability of selected beta-lactam antibiotics stored in plastic syringes. NITA. 1987;10(5):368–372. [PubMed] [Google Scholar]
- 82. Donnelly RF. Stability of cefazolin sodium in polypropylene syringes and polyvinylchloride minibags. Can J Hosp Pharm. 2011;64(4):241–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Stewart JT, Warren FW, Maddox FC. Stability of cefepime hydrochloride injection in polypropylene syringes at -20 degrees C, 4 degrees C, and 22-24 degrees C. Am J Health Syst Pharm. 1999;56(5):457–459. [DOI] [PubMed] [Google Scholar]
- 84. Stewart JT, Maddox FC, Warren FW. Stability of cefepime hydrochloride in polypropylene syringes. Am J Health Syst Pharm. 1999;56(11):1134. [DOI] [PubMed] [Google Scholar]
- 85. Garrelts JC, Wagner DJ. The pharmacokinetics, safety, and tolerance of cefepime administered as an intravenous bolus or as a rapid infusion. Ann Pharmacother. 1999;33(12):1258–1261. [DOI] [PubMed] [Google Scholar]
- 86. Stewart JT, Warren FW, Johnson SM, Fox JL, Mullaney J. Stability of ceftazidime in plastic syringes and glass vials under various storage conditions. Am J Hosp Pharm. 1992;49(11):2765–2768. [PubMed] [Google Scholar]
- 87. Plumridge RJ, Rieck AM, Annus TP, Langton SR. Stability of ceftriaxone sodium in polypropylene syringes at -20, 4, and 20 degrees C. Am J Health Syst Pharm. 1996;53(19):2320–2323. [DOI] [PubMed] [Google Scholar]
- 88. Robinson RF, Nahata MC. Safety of intravenous bolus administration of gentamicin in pediatric patients. Ann Pharmacother. 2001;35(11):1327–1331. [DOI] [PubMed] [Google Scholar]
- 89. Dobbs SM, Mawer GE. Intravenous injection of gentamicin and tobramycin without impairment of hearing. J Infect Dis. 1976;134 Suppl:S114–S117. [DOI] [PubMed] [Google Scholar]
- 90. Stratford BC, Dixson S, Cobcroft AJ. Serum levels of gentamicin and tobramycin after slow intravenous bolus injection. Lancet. 1974;1(7854):378–379. [DOI] [PubMed] [Google Scholar]
- 91. Van de Walle J, Adriaensen H. Letter: serum-gentamicin levels after intravenous bolus injection. Lancet. 1974;2(7879):525–526. [PubMed] [Google Scholar]
- 92. Lynn KL, Neale TJ, Little PJ, Bailey RR. Gentamicin by intravenous bolus injection. N Z Med J. 1974;80(528):442–443. [PubMed] [Google Scholar]
- 93. Edwards C, Bint AJ, Venables CW, Scott DK. Sampling time for serum gentamicin levels. J Antimicrob Chemother. 1992;29(5):575–578. [DOI] [PubMed] [Google Scholar]
- 94. Korsager S. Administration o gentamicin to obese patients. Int J Clin Pharmacol Ther Toxicol. 1980;18(12):549–553. [PubMed] [Google Scholar]
- 95. Daschner FD, Eschenbruch E, Metz B, Bayer E, Schmuziger M. Penetration of gentamicin into heart valves, subcutaneous and muscular tissue of patients undergoing open heart surgery. J Cardiovasc Surg (Torino). 1981;22(6):581–584. [PubMed] [Google Scholar]
- 96. Bastone EB, Li SC, Ioannides-Demos LL, Spicer WJ, McLean AJ. Kill kinetics and regrowth patterns of Escherichia coli exposed to gentamicin concentration-time profiles simulating in vivo bolus and infusion dosing. Antimicrob Agents Chemother. 1993;37(4):914–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Gillett AP, Falk RH, Andrews J, Wise R, Melikian V. Rapid intravenous injection of tobramycin: suggested dosage schedule and concentrations in serum. J Infect Dis. 1976;134 Suppl:S110–S113. [DOI] [PubMed] [Google Scholar]
- 98. Lilliestierna H, Alestig K, Holm S. Tobramycin therapy–two or three doses per day? Scand J Infect Dis. 1985;17(3):323–325. [DOI] [PubMed] [Google Scholar]
- 99. Adeboyeku D, Jones AL, Hodson ME. Twice vs three-times daily antibiotics in the treatment of pulmonary exacerbations of cystic fibrosis. J Cyst Fibros. 2011;10(1):25–30. [DOI] [PubMed] [Google Scholar]
- 100. Blouin RA, Mann HJ, Griffen WO, Jr, Bauer LA, Record KE. Tobramycin pharmacokinetics in morbidly obese patients. Clin Pharmacol Ther. 1979;26(4):508–512. [DOI] [PubMed] [Google Scholar]
- 101. Nafziger AN, Schwartzman MS, Bertino JS., Jr Absence of tobramycin pharmacokinetic and creatinine clearance variation during the menstrual cycle: implied absence of variation in glomerular filtration rate. J Clin Pharmacol. 1989;29(8):757–763. [DOI] [PubMed] [Google Scholar]
- 102. Pechere JC, Dugal R, Pechere MM. Pharmacokinetics of intravenous amikacin after rapid and slow infusion with special reference to hemodialysis. Eur J Drug Metab Pharmacokinet. 1979;4(1):49–56. [DOI] [PubMed] [Google Scholar]
- 103. Limthongkul S, Charoenlap P, Nuchprayoon CJ, Udompanich V, Songkhla YN. Amikacin pharmacokinetics in plasma and pleural fluid. J Med Assoc Thai. 1989;72(2):90–96. [PubMed] [Google Scholar]
- 104. Yates RA, Mitchard M. Disposition studies with amikacin after rapid intravenous and intramuscular administration to human volunteers. J Antimicrob Chemother. 1978;4(4):335–341. [DOI] [PubMed] [Google Scholar]
- 105. Somani P, Freimer EH, Gross ML, Higgins JT., Jr. Pharmacokinetics of imipenem-cilastatin in patients with renal insufficiency undergoing continuous ambulatory peritoneal dialysis. Antimicrob Agents Chemother. 1988;32(4):530–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Biggar C, Nichols C. Comparison of postinfusion phlebitis in intravenous push versus intravenous piggyback cefazolin. J Infus Nurs. 2012;35(6):384–388. [DOI] [PubMed] [Google Scholar]
- 107. Baumgartner JD, Glauser MP. Single daily dose treatment of severe refractory infections with ceftriaxone. Cost savings and possible parenteral outpatient treatment. Arch Intern Med. 1983;143(10):1868–1873. [PubMed] [Google Scholar]
- 108. Grubbauer HM, Dornbusch HJ, Dittrich P, et al. Ceftriaxone monotherapy for bacterial meningitis in children. Chemotherapy. 1990;36(6):441–447. [DOI] [PubMed] [Google Scholar]
- 109. Schaad UB, Stoeckel K. Single-dose pharmacokinetics of ceftriaxone in infants and young children. Antimicrob Agents Chemother. 1982;21(2):248–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Lossos IS, Lossos A. Hazards of rapid administration of ceftriaxone. Ann Pharmacother. 1994;28(6):807–808. [DOI] [PubMed] [Google Scholar]
- 111. Schaad UB, Wedgwood-Krucko J, Tschaeppeler H. Reversible ceftriaxone-associated biliary pseudolithiasis in children. Lancet. 1988;2(8625):1411–1413. [DOI] [PubMed] [Google Scholar]
- 112. Bradley JS, Wassel RT, Lee L, Nambiar S. Intravenous ceftriaxone and calcium in the neonate: assessing the risk for cardiopulmonary adverse events. Pediatrics. 2009;123(4):e609–e613. [DOI] [PubMed] [Google Scholar]
- 113. Cervera C, Sanroma P, Gonzalez-Ramallo V, et al. Safety and efficacy of daptomycin in outpatient parenteral antimicrobial therapy: a prospective and multicenter cohort study (DAPTODOM trial). Infect Dis (Lond). 2017;49(3):200–207. [DOI] [PubMed] [Google Scholar]
- 114. Schmidt S, Sloan A, Maxwell A, Swindler J. Evaluation of a standardized daptomycin dosing nomogram. Am J Health Syst Pharm. 2016;73(17)(suppl 4):S106–S111. [DOI] [PubMed] [Google Scholar]
- 115. Aoki I, Ishikawa K, Wakana A, Aso M, Yoshinari T. Evaluation of the safety, tolerability, and pharmacokinetics of a single bolus injection of daptomycin in healthy Japanese subjects. J Infect Chemother. 2015;21(3):170–175. [DOI] [PubMed] [Google Scholar]
- 116. Caulder CR, Sloan A, Yasir A, Bookstaver PB. Infusion-related reaction following daptomycin two-minute rapid intravenous administration. Hosp Pharm. 2014;49(7):644–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Ljungberg B, Nilsson-Ehle I. Pharmacokinetics of intravenous ciprofloxacin at three different doses. J Antimicrob Chemother. 1988;22(5):715–720. [DOI] [PubMed] [Google Scholar]
- 118. Adler D, Maier H. Gyrase inhibitor ciprofloxacin in human parotid saliva. J Clin Chem Clin Biochem. 1989;27(4):232–233. [PubMed] [Google Scholar]
- 119. Hoffken G, Lode H, Prinzing C, et al. Pharmacokinetics of ciprofloxacin after oral and parenteral administration. Antimicrob Agents Chemother. 1985;27(3):375–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Casthely PA, Ergin MA, Yoganathan T, et al. Hemodynamic changes after nafcillin administration during coronary artery bypass surgery. J Cardiothorac Anesth. 1989;3(2):168–171. [DOI] [PubMed] [Google Scholar]
- 121. Martin C, Cotin A, Giraud A, et al. Comparison of concentrations of sulbactam-ampicillin administered by bolus injections or bolus plus continuous infusion in tissues of patients undergoing colorectal surgery. Antimicrob Agents Chemother. 1998;42(5):1093–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Wallace SJ, Li J, Rayner CR, Coulthard K, Nation RL. Stability of colistin methanesulfonate in pharmaceutical products and solutions for administration to patients. Antimicrob Agents Chemother. 2008;52(9):3047–3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Conway SP, Etherington C, Munday J, Goldman MH, Strong JJ, Wootton M. Safety and tolerability of bolus intravenous colistin in acute respiratory exacerbations in adults with cystic fibrosis. Ann Pharmacother. 2000;34(11):1238–1242. [DOI] [PubMed] [Google Scholar]
- 124. Grayson ML. Kucers’ the Use of Antibiotics: A Clinical Review of Antibacterial, Antifungal, Antiparasitic and Antiviral Drugs. Vol 1, 6th ed. London, England: Edward Arnold; 2010. [Google Scholar]
- 125. Holloway WJ. Preliminary report on intravenous doxycycline. Del Med J. 1971;43(11):394–397. [PubMed] [Google Scholar]
- 126. Seifert CF, Swaney RJ, Bellanger-McCleery RA. Intravenous erythromycin lactobionate-induced severe nausea and vomiting. DICP. 1989;23(1):40–44. [DOI] [PubMed] [Google Scholar]
- 127. Aucoin P, Beckner RR, Gantz NM. Clindamycin-induced cardiac arrest. South Med J. 1982;75(6):768. [DOI] [PubMed] [Google Scholar]
- 128. Waisbren BA. Lincomycin in larger doses. JAMA. 1968;206(9):2118. [PubMed] [Google Scholar]
- 129. Ljungberg B, Nilsson-Ehle I, Ursing B. Metronidazole: pharmacokinetic observations in severely ill patients. J Antimicrob Chemother. 1984;14(3):275–283. [DOI] [PubMed] [Google Scholar]
- 130. Lenz JR, Degnan DD, Hertig JB, Stevenson JG. A review of best practices for intravenous push medication administration. J Infus Nurs. 2017;40(6):354–358. [DOI] [PubMed] [Google Scholar]
- 131. Alexander M, Alsbrooks K, Andreica I, et al. ISMP safe practice guidelines for adult IV push medications. Institute for Safe Medication Practices website; https://www.ismp.org/Tools/guidelines/IVSummitPush/IVPushMedGuidelines.pdf. Published 2015. Accessed December 18, 2017 [Google Scholar]
- 132. Adams J, Bierman S, Mares A, et al. Infusion therapy standards of practice. J Infus Nurs. 2016;39(1S):S1–S156. [Google Scholar]
- 133. Nowobilski-Vasilios A, Poole SM. Development and preliminary outcomes of a program for administering antimicrobials by i.v. push in home care. Am J Health Syst Pharm. 1999;56(1):76–79. [DOI] [PubMed] [Google Scholar]
- 134. Santeiro ML, Sagraves R, Allen LV., Jr Osmolality of small-volume i.v. admixtures for pediatric patients. Am J Hosp Pharm. 1990;47(6):1359–1364. [PubMed] [Google Scholar]
- 135. Miano B, Wood W. Implementation of the i.v. push method of antibiotic administration using the FOCUS/PDCA approach. Home Healthc Nurse. 1998;16(12):831–837. [DOI] [PubMed] [Google Scholar]
- 136. Institute for Safe Medication Practices. Some IV medications are diluted unnecessarily in patient care areas, creating undue risk. Institute for Safe Medication Practices website. https://www.ismp.org/newsletters/acutecare/showarticle.aspx?id=82. Published June 19, 2014. Accessed December 18, 2017.
- 137. Centers for Disease Control Prevention. One and only campaign. Centers for Disease Control and Prevention website; http://www.oneandonlycampaign.org/. Accessed December 18, 2017. [Google Scholar]
- 138. Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26(1):1–10. [DOI] [PubMed] [Google Scholar]
- 139. Butterfield-Cowper JM, Burgner K. Effects of i.v. push administration on β-lactam pharmacodynamics. Am J Health Syst Pharm. 2017;74(9):e170–e175. [DOI] [PubMed] [Google Scholar]
- 140. Jaruratanasirikul S, Sriwiriyajan S, Punyo J. Comparison of the pharmacodynamics of meropenem in patients with ventilator-associated pneumonia following administration by 3-hour infusion or bolus injection. Antimicrob Agents Chemother. 2005;49(4):1337–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Lodise TP, Jr, Lomaestro B, Drusano GL. Piperacillin-tazobactam for Pseudomonas aeruginosa infection: clinical implications of an extended-infusion dosing strategy. Clin Infect Dis. 2007;44(3):357–363. [DOI] [PubMed] [Google Scholar]
- 142. Rhodes NJ, Liu J, O’Donnell JN, et al. Prolonged infusion piperacillin-tazobactam decreases mortality and improves outcomes in severely ill patients: results of a systematic review and meta-analysis. Crit Care Med. 2018;46:236–243. [DOI] [PubMed] [Google Scholar]
- 143. Dulhunty JM, Roberts JA, Davis JS, et al. Continuous infusion of beta-lactam antibiotics in severe sepsis: a multicenter double-blind, randomized controlled trial. Clin Infect Dis. 2013;56(2):236–244. [DOI] [PubMed] [Google Scholar]