Abstract
Pediatric primary care providers play a critical role in managing obesity yet often lack the resources and support systems to provide effective care to children with obesity. The objective of this study was to identify system-level barriers to managing obesity and resources desired to better managing obesity from the perspective of pediatric primary care providers. A 64-item survey was electronically administered to 159 primary care providers from 26 practices within a large pediatric primary care network. Bivariate analyses were performed to compare survey responses based on provider and practice characteristics. Also factor analysis was conducted to determine key constructs that effect pediatric interventions for obesity. Survey response rate was 69% (n = 109), with the majority of respondents being female (77%), physicians (67%), and without prior training in obesity management (74%). Time constraints during well visits (86%) and lack of ancillary staff (82%) were the most frequently reported barriers to obesity management. Information on community resources (99%), an on-site dietitian (96%), and patient educational materials (94%) were most frequently identified as potentially helpful for management of obesity in the primary care setting. Providers who desired more ancillary staff were significantly more likely to practice in clinics with a higher percentage of obese, Medicaid, and Hispanic patients. Integrating ancillary lifestyle expert support into primary care practices and connecting primary care practices to community organizations may be a successful strategy for assisting primary care providers with managing childhood obesity, especially among vulnerable populations.
Keywords: Medical home, obesity resources, pediatric obesity, primary care
Introduction
Obesity in children is an international public health priority, with more than 41 million children in the world affected currently and over 60 million children (prevalence rate of 9%) expected to be affected by 2020 (World Health Organization, 2017). The problem is even worse in the United States, with almost 20% of children affected by obesity (Ogden et al., 2016). Children with obesity are at risk for the development of associated comorbidities such as cardiovascular disease (Skinner et al., 2015), type 2 diabetes (Abbasi et al., 2017), and behavioral health issues (Pulgarón, 2013). In the United States, expert guidelines recommend a staged approach to the management of childhood obesity, starting with efforts in the primary care setting and advancing to intensive interdisciplinary treatment in tertiary care settings if needed (Spear et al., 2007). While tertiary care treatment can be an effective option, access to these programs is limited and these programs require significant resources that are often not available in areas of the United States and the world (Hampl et al., 2016; Skelton et al., 2008). Therefore, it is important to enhance the scope of obesity care available in pediatric primary care practices in order to prevent and treat childhood obesity with approaches that are accessible and cost-effective.
Primary care providers in the United States are faced with challenges and issues of childhood obesity among their patient population: they cite barriers to providing optimal care to children with obesity (Van Gerwen et al., 2009). While some of these barriers are at the individual provider or patient level, many exist at the practice level, including poor reimbursement, lack of resources to help support lifestyle counseling, and lack of time to conduct appropriate counseling during health supervision visits (Ciupitu and Babitsch, 2011; Spivack et al., 2010; Staiano et al., 2017). These system-level barriers are similarly voiced by primary care providers in other countries (Maryon-Davis, 2005).
Identifying and addressing practice-level barriers to obesity care in the primary care setting can increase a practice’s capacity as a patient-centered medical home (PCMH) by enhancing their internal resources and improving their internal processes (Miller et al., 2010). The PCMH is an ideal model for the management of chronic diseases like obesity because it provides continuous, coordinated, and comprehensive team-based care; integrates services across settings and providers; and promotes high-quality care by leveraging health information technology (Agency for Healthcare Research and Quality, 2018). For example, several studies in the United States have demonstrated successful management of obesity through the integration of dietitians, behavioral health specialists, or lifestyle-trained providers into pediatric primary care settings (Eneli et al., 2014; Pomietto et al., 2009; Steele et al., 2012; Taveras et al., 2017). Other studies have demonstrated successful use of electronic health records (EHRs) based on clinical decision support systems (Rattay et al., 2009; Taveras et al., 2015) and obesity counseling tools in pediatric primary care settings (McGaffey et al., 2011; Polacsek et al., 2009; Sanders et al., 2014). Finally, interventions that have offered opportunities for practices to enhance established partnerships with local organizations and improve access to community resources for patients have also demonstrated success (Ariza et al., 2012; Polacsek et al., 2009).
Integrated primary care, supported by several international medical associations, including the Canadian Medical Association and National Institute for Health and Care Excellence, has found that counseling by primary care providers is most effective when delivered by an interdisciplinary team as part of an integrated comprehensive approach (NICE, 2014; Parkin et al., 2015).
While these studies have demonstrated success in integrating different resources to support obesity care in individual pediatric primary care settings, prior studies have not comprehensively explored provider perspectives about which of a multitude of integrated resources, including those represented in most multidisciplinary weight management programs, they believe would best augment their care delivery to children with obesity across multiple practice settings. Each of these practices operates as individual complex adaptive systems and may have different barriers and needs based on provider and practice characteristics (Abatemarco et al., 2008). Understanding system or practice barriers and structuring supports on the practice level has the ability to change individual care (Abatemarco et al., 2012).
Aims
We conducted a comprehensive prospective survey of primary care providers within a large children’s health system, with the objective of identifying perceived barriers to obesity management and resources needed to manage childhood obesity within their practice based on integrating intervention components of the PCMH. We then analyzed the barriers and needs by provider and practice characteristics. The intent of our research was to design and pilot a survey to identify resources needed by providers to integrate into their practice to augment their care of children with obesity as well as to inform future interventional studies.
Methods
Participants
We surveyed all pediatric primary care providers (n = 159), including physicians (MD), advanced nurse practitioners, and registered nurses (RNs), employed by 26 primary care practices in a large children’s health system in the United States. These practices are located in urban, suburban, and rural communities, ranging in distance from 3 miles to 98 miles from a tertiary care setting that includes a comprehensive pediatric weight management program and with variable access to obesity resources and obesity training (see Results section for further detail). The practices included in this study serve pediatric patient populations from diverse ethnic and economic backgrounds (see Results section for further detail). Among these primary care practices within this health system, 14 were located in the Mideast United States and 12 were located in the Southeast United States. The Mideast is a highly populated area with approximately 7 million predominately African Americans (43%), Caucasian (41%), and Hispanic inhabitants (12%). It has the ninth largest economy among 382 metropolitan areas in the United States. The Southeast in contrast has a population around 21 million, with a predominately Caucasian demographic (77%), followed by 25% Hispanic and 16% African American, and has the fourth largest economy in the United States (United States Census Bureau, 2017; United States Department of Commerce, Bureau of Economic Analysis, 2017).
Survey administration
An anonymous survey was collected using REDCap software version 7.6.6, a secure web-based application for building and managing online surveys and databases (Harris et al., 2009). An e-mail from the research team was sent through the REDCap software to the work e-mail of participants with a secure link to the online survey. Time to complete the survey was approximately 10 minutes.
Completion of the survey by a participant was documented in REDCap in a database separate from and not linked to survey responses to protect participant anonymity. This process of anonymity was described in detail in the consent. Providers who completed the survey were mailed a US$10 gift card for participation. Providers who had not completed the survey were sent weekly reminder e-mails over five weeks through an automated system in REDCap. Each reminder was delivered on a different day and at a different time, until survey completion. This survey strategy had been successfully utilized with primary care providers in another research study with a participation rate of 70% (DiGuglielmo et al., 2013). Providers who did not respond to the e-mail reminders received a reminder call prior to the end of the study.
Pediatric primary care obesity resource survey
The Pediatric Primary Care Obesity Resource Survey (Online Appendix 1) was developed by an expert committee consisting of four pediatricians with expertise in childhood obesity and population health and a population health researcher with expertise in pediatric practice change. The 64-item survey assessed provider demographics and aspects of clinical training and practice, including area of training, length of time since training, receipt of obesity-specific training, and practice location. If a provider provided direct obesity care for children, they were directed to take an additional portion of the survey that assessed three domains: (1) impact of system-level barriers on their ability to manage obesity, (2) providers’ current use of 11 commonly available obesity resources and how helpful they believed these resources to be, and (3) helpfulness of nine potential obesity resources whether integrated into their practice and how frequently would they be used by the providers. All questions in the survey were assessed on a five-point Likert-type scale and an open-ended question was asked in each domain to allow for qualitative responses.
The survey was developed based on evidence from prior studies assessing primary care provider views about obesity management and barriers to obesity management (Feinson et al., 2010; Perrin et al., 2005; Rattay et al., 2009; Spear et al., 2007; Spivack et al., 2010). Additionally, the items in the two domains related to obesity resources were based on elements of Wagner’s chronic care model (Wagner, 1998) and the PCMH, including an integrated care team, health information technology tools, educational resources for self-management, and community resources. The survey was pilot tested in focused interviews with five primary care providers from diverse practices in the network and reviewed with the institution’s primary care practice-based research network to solicit feedback about the survey content, comprehension, and format, which was incorporated into a revised survey.
Practice characteristics
De-identified data from the EHR were extracted to describe the patient population treated at each practice for the year prior to the survey administration, including demographic composition (age, gender, race, ethnicity, and insurance status) and rates of overweight and obesity (body mass index (BMI) ≥ 85% for age based on the US Center for Disease Control and Prevention growth curves (CDC, 2016). Practices were also identified as ‘academic’ if trainees received education and provided patient care at the practice. Practices in the children’s health system were categorized as either Mideast or Southeast based on their geographic location.
Statistical analysis
Demographic characteristics of providers and practice populations and responses to survey questions were described with proportions for categorical variables and means and standard deviations for continuous variables. The frequency of responses for which an item received a rating of 4 or 5 (agree or strongly agree, often or always, or somewhat helpful or very helpful depending on the type of question asked) was calculated as positive responses for the purpose of analyses. Chi-square and independent t-test analyses were performed to compare survey responses based on provider and practice characteristics. Additionally, we conducted psychometric analyses for the new survey: (1) correlation analyses to examine intra-domain reliability and internal consistency and (2) exploratory principal components factor analyses with a varimax rotation to examine the emergent factor structure of the questions. Data analysis was performed using SPSS version 22 (IBM Corporation, 2013).
Ethics consideration
This study was approved by the Children’s Health System’s Institutional Research Board (IRB no 731053–6) and Primary Care Practice Based Research Network. Participants signed an e-consent as part of the electronic survey.
Results
Provider characteristics
Of 159 potential participants, 109 completed the survey (response rate of 69%) and there were fewer than 2% of responses missing for any item. Of the 109 participants who completed the survey, 22 (20%) reported that they did not provide direct patient care and did not complete the survey portion of the survey. Data are reported for the 87 participants who reported that they provided direct patient care. The demographic characteristics of all the respondents are characterized in Table 1. The majority of providers were female pediatricians over the age of 45 years, practicing in a nonacademic practice in the Mideast. The majority of providers had not received obesity-specific training and had been practicing for at least five years.
Table 1.
Pediatric primary care provider characteristics (N = 87).
| Provider characteristic | N(%) |
|---|---|
| Practice location | |
| Mideast region | 67 (77.0) |
| Southeast region | 20 (23.0) |
| Type of provider | |
| Physicians | 58 (66.7) |
| Received specific training in obesity | 16 (27.6) |
| RNs | 29 (33.3) |
| Received specific training in obesity | 7 (24.1) |
| Female | 68 (77.3) |
| Age | |
| Less than 45 years | 43 (49.4) |
| 45 years or older | 44 (50.6) |
| Type of training | |
| Pediatrics | 85 (97.7) |
| Med-Peds or family medicine | 2 (2.3) |
| Practicing in an academic setting | 27(31.0) |
| Time since training (years) | |
| Under 5 years | 21 (24.1) |
| 5 or more years | 79 (75.9) |
RN: registered nurse.
Patient characteristics at practices
Within the 26 primary care practices, 76,877 patients from birth to 18 years old were seen in the year prior to survey completion (Table 2), representing a diverse patient population (37% African Americans, 12% Hispanic, and 45% with public insurance). Among the patient population, 15% (n = 11,531) had overweight (85th to 94th percentile), 12% (n = 9,225) had obesity (95th to 98th percentile), and 5% (n = 3,843) had severe obesity (≥ 99th percentile) based on their documented BMI percentile for age at their last clinic visit, based on CDC growth charts.
Table 2.
Characteristics of practices’ patient population (N = 76,877 in 25 practices).
| Patient characteristic | Mean % of practice patients (SD) |
|---|---|
| Age | |
| <5 years | 35.0 (3.6) |
| 5–1 1 years | 35.0 (2.8) |
| 12–18 years | 30.0 (4.1) |
| Female | 49.0 (2.9) |
| Race | |
| White | 41.0 (19.5) |
| Black | 37.0 (21.7) |
| Other | 22.0 (14.1) |
| Ethnicity | |
| Non-Hispanic | 81.0 (17.4) |
| Hispanic | 12.0 (8.8) |
| Other | 7.0 (11.0) |
| Language spoken | |
| English | 91.0 (8.1) |
| Spanish | 6.0 (8.2) |
| Other | 3.0 (2.2) |
| Public insurance | 45.0 (26.0) |
| Weight status | |
| Under or normal weight (BMI < 85th) | 69.0 (5.3) |
| Overweight (BMI = 85th to 94.9th) | 15.0 (1.7) |
| Obesity (BMI = 95th to 98.9th) | 12.0 (2.3) |
| Morbid obesity (BMI > 99th) | 5.0 (1.6) |
SD: standard deviation; BMI: body mass index.
System-level barriers to obesity care
The most frequently agreed upon barriers to obesity management (rated as agree or strongly agree) were time constraints during well visits (routine preventive checkups, 86%) and lack of ancillary staff (82%; Figure 1). The majority of providers also agreed that access to schedule obesity-specific visits, lack of patient education materials, and lack of administrative support on an organizational level were barriers to obesity management. Poor reimbursement was less frequently endorsed. Providers with no obesity training were significantly more likely to agree that lack of culturally appropriate educational handouts was a barrier to obesity management compared to providers with obesity training (66% vs. 38%, p = .02).
Figure 1.
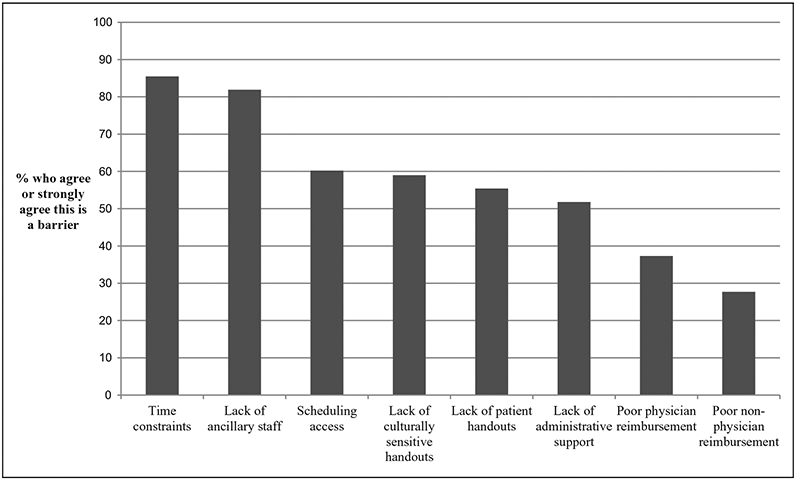
Perceived system-level barriers to obesity care among pediatric primary.
Resources used in obesity management
Among commonly available resources to manage obesity, those most utilized (most frequently rated as used often or always) and cited as helpful (most frequently rated as somewhat or very helpful) by providers were patient educational handouts (49%) and referrals to tertiary care weight management clinics (48%; Table 3). There were significant differences between utilization of available resources between practices in the Mideast and Southeast regions, with more frequent utilization of websites in the Southeast (35% vs. 13%, t (85) = 2.221, p = .03) versus more frequent utilization of tertiary care weight management clinics (55% vs. 25%,t(85) = 2.426, p = .02) and psychologists (27% vs. 5%, t (85) = 2.106, p = .04) in the Mideast region. In both obesity-trained providers reported making areas, more referrals to exercise programs compared to nonobesity-trained providers (30% vs. 11%, t (85) 2.219, p .03). More providers in the Mideast region believed social workers to be helpful in managing obesity (64% vs. 25%, respectively, t (54) = 2.473, p = .02). Providers also commented that they referred patients to pediatric endocrine or gastroenterology specialists.
Table 3.
Frequency of use and perceived helpfulness of available resources for obesity management.
| Currently available obesity resource | Providers who use the resource often or always (N (%)) | Of those who use the resource, believe the resource is somewhat or very helpful (N (%)) |
|---|---|---|
| Educational handouts | 43 (49.4) | 61 (82.4) |
| EHR discharge instructions | 24 (27.6) | 39 (73.6) |
| Websites | 16 (18.4) | 34(61.8) |
| Nutrition props | 14 (16.1) | 29 (69.0) |
| EHR smart tools | 14 (16.1) | 28 (52.8) |
| Mobile apps | 7 (8.0) | 17 (58.6) |
| Tertiary care weight management clinic | 42 (48.3) | 68 (88.3) |
| Dietitian | 25 (28.7) | 60 (80.0) |
| Psychologist | 19 (21.8) | 51 (70.8) |
| Community exercise program | 14 (16.1) | 50 (75.8) |
| Social worker | 6 (6.9) | 31 (55.4) |
| Other weight management program | 6 (6.9) | 26 (53.1) |
EHR: electronic health record.
Desired resources for obesity management
Each of the 11 suggested resources to augment obesity management, based on the PCMH, was endorsed as potentially helpful (rated as somewhat or very helpful) by the majority of providers (Table 4). Information on community resources, an on-site dietitian, and patient educational materials were the resources that providers most frequently reported they would find helpful (98.7%, 96.1%, and 94.1%, respectively). Resource providers would use most often (rated as would use often or always) including information on community resources, an on-site dietitian, and an on-site exercise physiologist (96.1%, 94.7%, and 93.6%, respectively).
Table 4.
Potential resources to augment obesity management.
| Obesity resource | Providers would use the resource often or always (N (%)) | Providers agree or strongly agree the resource would be helpful (N (%)) |
|---|---|---|
| Information about community resources | 73 (96.1) | 75 (98.7) |
| Patient educational materials | 62 (92.5) | 64 (94.1) |
| Culturally sensitive educational materials | 68 (93.2) | 68 (91.9) |
| Patient portal | 59 (76.6) | 67 (83.8) |
| Physician EHR dashboard | 56 (74.7) | 60 (75.0) |
| On-site dietitian | 72 (94.7) | 73(96.1) |
| On-site exercise physiologist | 73 (93.6) | 70 (88.6) |
| On-site psychologist | 40 (76.9) | 44 (81.5) |
| On-site social worker/case manager | 34 (59.6) | 42 (71.2) |
| Telehealth connections to tertiary care | 38 (58.5) | 42 (71.2) |
| Health coach | 57 (72.2) | 69 (63.3) |
EHR: electronic health record.
A greater proportion of physicians reported that an on-site dietitian would be helpful, while a greater proportion of RNs reported that telehealth services would be helpful (Table 5). Younger physicians were more likely to report that electronic dashboards and portals would be helpful, while those without obesity training or practicing in nonacademic settings were more likely to endorse that more patient educational handouts would be helpful. Providers were significantly more likely to report that additional on-site lifestyle specialists would be helpful if they came from practices with higher percentages of patients with obesity, with public insurance, and of Hispanic ethnicity (Table 6).
Table 5.
Differences in desired resources based on provider characteristics.
| Desired resource | Provider characteristic | N(%) | χ2 | df | P |
|---|---|---|---|---|---|
| On-site dietitians | Physician* | 51 (100.0) | 6.37 | 1 | .01 |
| RN | 22 (88.0) | ||||
| Telehealth | Physician | 34 (64.2) | 4.74 | 1 | .03 |
| RN* | 18 (90.0) | ||||
| Culturally sensitive handouts | Obesity trained | 15 (78.9) | 5.75 | 1 | .02 |
| Not obesity trained* | 53 (96.4) | ||||
| Electronic dashboard for physicians to track weight and goals | < 45 years old* | 34 (89.5) | 8.09 | 1 | .004 |
| ≥ 45 years old | 26 (61.9) | ||||
| Electronic portal for patients to track weight and goals | < 45 years old* | 36 (94.7) | 6.42 | 1 | .01 |
| ≥ 45 years old | 31 (73.8) | ||||
| Patient educational materials | Academic practice | 17 (85.0) | 4.25 | 1 | .04 |
| Nonacademic* practice | 47 (97.9) |
RN: registered nurse.
Characteristic of providers who were more likely to rate resource as helpful.
Table 6.
Differences in desired resources by practice characteristics.
| Patient characteristic | Obesity resource | Percentage of patients in practice with characteristic (mean (SD)) | t Value | df | P |
|---|---|---|---|---|---|
| Obesity | Desire on-site dietitian* | 11.5 (2.4) | 2.10 | 70 | .04 |
| Don’t desire on-site dietitian | 8.6 (2.5) | ||||
| Public insurance | Desire on-site dietitian* | 45.1 (12.7) | 2.23 | 70 | .03 |
| Don’t desire on-site dietitian | 7.8 (28.7) | ||||
| Public insurance | Desire on-site exercise* specialist | 46.4 (27.5) | 2.22 | 73 | .03 |
| Don’t desire on-site exercise specialist | 24.4 (30.9) | ||||
| Hispanic ethnicity | Desire on-site psychologist* | 13.8 (8.6) | 2.41 | 48 | .02 |
| Don’t desire on-site psychologist | 6.8 (5.9) |
SD: standard deviation.
Obesity resource desired by providers from practices with a greater percentage of patients with noted characteristic.
Reliability of survey
Factor analysis of the survey resulted in several key constructs from each domain, falling within expected theoretical constructs with high reliability (Cronbach’s α = .65–.86; Table 7).
Table 7.
Emerging constructs from factor analysis of pediatric obesity survey.
| Constructs | Barriers | Cronbach α |
|---|---|---|
| Practice level | Time constraints, lack of ancillary staff, poor MD reimbursement, and poor non-MD reimbursement | .78 |
| Patient resources | Lack of educational materials and culturally sensitive educational materials | .86 |
| Administrative | Scheduling access, lack of ancillary staff, and lack of administrative support | .65 |
| Current resource utilization | ||
| External personnel | Dietitian, psychologist, social worker, and tertiary care weight management clinic | .79 |
| External resources | Nutrition props, websites, and mobile apps | .70 |
| Internal resources | EHR smart tools, EHR discharge instructions, and educational materials | .72 |
| Helpfulness of potential integrated resources | ||
| On-site personnel | Dietitian, exercise physiologist, psychologist, and social worker | .78 |
| Information technology | Telehealth, physician dashboard, and patient portal | .79 |
| Educational resources | Health coach, educational materials, and culturally sensitive educational materials | .71 |
| Community resources | Information about community resources | .94 |
| Reported utilization frequency of potential integrated resources | ||
| On-site personnel | Dietitian, exercise physiologist, psychologist, and social worker | .82 |
| Educational and community resources | Educational materials, culturally sensitive educational materials, and community resources | .85 |
| Information technology and provider extenders | Telehealth, health coach, EHR dashboard, and patient portal | .84 |
EHR: electronic health record; MD: Medical Doctor.
Discussion
We conducted a primary care provider survey to describe perceived barriers to obesity management as well as the need for resources that could be integrated within the pediatric primary care setting, based on the PCMH, to improve obesity management. This research had three main findings. First, time constraints and lack of ancillary staff were the greatest system-level barriers to managing childhood obesity endorsed by providers. Second, few resources to manage obesity were being used by providers at the time of the survey, with the exception of patient educational handouts and referrals to tertiary care weight management clinics. Finally, providers most frequently reported that information on community resources and ancillary on-site lifestyle experts would be helpful resources to have in the primary care setting.
Consistent with prior studies, providers in this study reported many similar system-level barriers to managing obesity in their primary care practice, including time constraints, lack of patient educational materials, and lack of reimbursement. The most frequently endorsed items of lack of time and ancillary staff were frequently cited in other studies (Ciupitu and Babitsch, 2011; Findholt et al., 2013; Spivack et al., 2010; Staniford, 2011) and signal the potential utility of integrating additional staffing into settings to supplement care and reduce the time burden related to obesity counseling. Lack of physician and nonphysician reimbursement was not widely endorsed and even less frequently endorsed than in prior studies (Perrin et al., 2005). This may be due to new reimbursement mechanisms under the Medicaid Early and Periodic Screening, Diagnostic, and Treatment for nutrition and obesity screening and counseling for children that have been in place in the United States since 2010 (Sebelius, 2014), the lack of which may pose more challenges for providers in practices globally.
Less than half of providers endorsed using any of the 11 obesity resources that are currently available in their practices. This supports the idea that providers are not equipped to provide adequate care for obesity in their current setting (Spivack et al., 2010). Of these resources, patient educational handouts and referrals to tertiary care weight management clinics were the ones most often used by providers but have limitations. While patient educational materials can be useful at reinforcing messaging about healthy lifestyles, they require time on the part of providers to explain and often times are not literacy or culturally appropriate for families (Klingbeil et al., 2016).
Notably, tertiary care weight management clinics and psychologists were more often used in the Mideast, which is likely due to the greater access to specialists in the Mideast practices. However, while children who attend tertiary care weight management clinics demonstrate improvements in weight status, they pose several limitations (Hampl et al., 2016; Skelton et al., 2008; Whitlock et al., 2010). For example, tertiary care weight management clinics have high attrition rates, present access challenges for families, are resource intensive, and are not commonly available in many areas of the United States and other countries (Children’s Hospital Association, 2014; Dhaliwal et al., 2014), suggesting a need to find other solutions for primary care providers.
The majority of providers believed that all of the obesity resources based on Wagner’s chronic care model and the PCMH would be useful if integrated into their practice setting, especially access to ancillary lifestyle staff and information about community resources. These findings align with the current United States Preventive Task Force recommendations that endorse integrated, intensive obesity interventions provided by a multidisciplinary care team within the medical home that includes clinic-community linkages (Wilfley et al., 2017). Indeed, lifestyle specialists like dietitians, exercise specialists, and psychologists are trained to provide healthy lifestyle education and counseling and can provide this expert care to families, reducing the time commitment needed for these important tasks from primary care providers (Vine et al., 2013). Our findings also speak to primary care provider acknowledgment of the importance of a child’s community environment in helping to promote health, which is supported by several studies describing successful community–practice partnerships for childhood obesity in the United States (Ariza et al., 2012; Polacsek et al., 2009). Indeed, a child’s local community is an important setting for obesity intervention in all countries and this survey speaks to primary care providers’ desire to be able to link their patients to available community resources.
There were several important differences in desired resources based on provider and practice characteristics. Better obesity counseling tools, particularly those that are tailored to a patient’s specific culture, have been shown to improve physician self-efficacy (Perrin et al., 2005) so it is not a surprise that providers who were not obesity trained and who were from nonacademic settings were more likely to desire more patient educational materials. Interestingly, providers younger than 45 years of age were more likely to report that EHR tools such as physician dashboards and patient portals would be helpful, which again is not surprising given the generational difference in comfort using technology (McAlearney et al., 2015). Perhaps, the most important difference is that providers from practices with a higher percent of obese, Hispanic, and Medicaid patients were more likely to think that the integration of on-site ancillary staff to assist with lifestyle behavior counseling would be helpful. This important finding suggests an acknowledgment by primary care providers of the need for greater interdisciplinary support to manage patient populations with more severe disease, more cultural barriers, and greater economic hardships (Ogden et al., 2016; Skelton et al., 2008).
This study has several strengths worth noting. First, we obtained accurate demographic characteristics of the patient population treated at these 26 practices using objective data abstracted from the EHR instead of relying on provider report and therefore could accurately describe how responses about obesity resources varied based on practice characteristics. Our survey administration methods, modeled after DiGuglielmo et al. (2013) and importantly stressing anonymity of response, were an effective strategy in achieving a good survey response rate (69%), particularly among physicians who are typically poor survey responders (Delnevo et al., 2004). Finally, the survey comprehensively assessed obesity resource utilization and needs from the perspective of primary care providers, who are on the front line of obesity prevention and treatment efforts but face many barriers. Factor analysis of the survey demonstrated strong intra-domain reliability with constructs grouping resources of similar characteristics.
There are several limitations to consider as well. Since participants represented a single, but large, health system’s providers in the United States, we are limited in our ability to generalize to pediatric providers in other states and countries. The primary care practices surveyed may also have increased access to obesity resources due to their affiliation with a hospital system with a comprehensive pediatric weight management program compared to independent primary care practices in the United States and abroad. However, we attempted to address this limitation by collecting data from practices of diverse sizes, types, and regions, located different distances from the comprehensive pediatric weight management program. In addition, providers with the greatest frustrations, successes, or interest in managing obesity may have been more likely to respond, leading to a selection bias. However, the diversity of our respondents and the near 70% participation rate lead us to believe that this bias is minimal in our survey.
Conclusion
Our study identified that lack of ancillary staff and time constraints currently obstruct effective obesity management in primary care practices. To combat these barriers, primary care providers recognize that the key components of a PCMH, including connections with the community and integrated inter-disciplinary staff, would help them overcome many of these barriers. This study suggests that integrated teams that include nutrition and exercise education capabilities, coupled with educational materials to enhance family’s self-management skills and information about community resources to strengthen the adoption of healthy lifestyle outside of the home and practice setting, may have an impact in improving care for children with obesity. Understanding these barriers to obesity care and then providing the resource and practice supports can positively influence a primary care provider’s behavior (Delnevo et al., 2003). While there have been a few promising examples of interdisciplinary obesity teams in the primary care setting (Eneli et al., 2014; Pomietto et al., 2009; Steele et al., 2012; Taveras et al., 2017), more studies are needed both nationally and internationally to show long-term impact on childhood obesity outcomes among diverse patient populations.
Supplementary Material
Acknowledgements
We thank the pediatric primary care providers who participated in the surveys, the Nemours Primary Care Practice Based Research Network for supporting our efforts, and Dr Marianna LaNoue for her assistance with data analysis.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Nemours Research Institute. Dr Phan also receives support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under award number K23HD083439.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental material
Supplementary material for this article is available online.
References
- Abatemarco DJ, Kairys SW, Gubernick RS, et al. (2008) Expanding the pediatrician’s black bag: a psychosocial care improvement model to address the new morbidities. The Joint Commission Journal on Quality and Patient Safety 334: 106–115. [DOI] [PubMed] [Google Scholar]
- Abatemarco DJ, Kairys SW, Gubernick RS, et al. (2012). Using genograms to understand pediatric practices’ readiness for change to prevent abuse and neglect. Journal of Child Health Care 16(2): 153–65. [DOI] [PubMed] [Google Scholar]
- Abbasi A, Juszczyk D, van Jaarsveld CHM, et al. (2017) Body mass index and incident type 1 and type 2 diabetes in children and young adults: a retrospective cohort study. Journal of Endocrine Society 1(5): 524–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality (2018) Defining the PCMH. Available at: https://www.pcmh.ahrq.gov/page/defining-pcmh (accessed 30 March 2018).
- Ariza AJ, Ruch-Ross H, Sawyer A, et al. (2012) Obesity care strategies in primary care practices. Journal of Pediatrics 161(1): 152–155. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention (2016) CDC Growth Charts. Available at: https://www.cdc.gov/growthcharts/cdc_charts.htm (accessed 30 March 2018).
- Children’s Hospital Association (2014) 2013 Survey Findings of Children’s Hospitals Obesity Services. Available at: https://www.childrenshospitals.org/issues-andadvocacy/population-health/obesity/reports/2013/2013-survey-findings-of-childrenshospitals-obesity-services (accessed 30 March 2018).
- Ciupitu CC and Babitsch B (2011) Why is it not working? Identifying barriers to the therapy of paediatric obesity in an intercultural setting. Journal of Child Health Care 15(2): 140–150. [DOI] [PubMed] [Google Scholar]
- Delnevo CD, Abatemarco DJ and Steinberg MB (2004) Physician response rates to a mail survey by specialty and timing of incentive. American Journal of Preventative Medicine 26(3): 234–236. [DOI] [PubMed] [Google Scholar]
- Delnevo CD, Steinberg MB, Abatemarco DJ, et al. (2003). Correlates of clinical preventive practices among internal medicine residents. Preventative Medicine 36(6): 645–651. [DOI] [PubMed] [Google Scholar]
- Dhaliwal J, Nosworthy NM, Holt NL, et al. (2014) Attrition and the management of pediatric obesity: an integrative review. Childhood Obesity 10(6): 461–473. [DOI] [PubMed] [Google Scholar]
- DiGuglielmo M, Plesnick J, Greenspan J, et al. (2013) A new model to decrease time-to-appointment wait for gastroenterology evaluation. Pediatrics 131(5): e1632–e1638. [DOI] [PubMed] [Google Scholar]
- Eneli I, Polas P and Watawocz R (2014) The Primary Care Obesity Network (PCON): Building Clinic-Community Integration in Stage 1 and Stage 2 Programs. In: American Academy of Pediatrics Experience National Conference & Exhibition, San Diego, CA, 10 October 2014. [Google Scholar]
- Feinson J, Atkinson A and Hassink S (2010) How a primary care quality improvement initiative is implementing the expert recommendations on childhood obesity. Delaware Medical Journal 82(2): 57–65. [PubMed] [Google Scholar]
- Findholt NE, Davis MM and Michael YL (2013) Perceived barriers, resources, and training needs of rural primary care providers relevant to the management of childhood obesity. Journal of Rural Health 29(Suppl 1): s17–s24. [DOI] [PubMed] [Google Scholar]
- Hampl S, Borner K, Dean K, et al. (2016) Patient attendance and outcomes in a structured weight management program. Journal of Pediatrics 176: 30–35. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R and Thielke R (2009) Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics 42(2): 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corporation (2013) IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. [Google Scholar]
- Klingbeil C, Speece MW and Schubiner H (2016) Readability of pediatric patient education materials. Clinical Pediatrics 34(2): 96–102. [DOI] [PubMed] [Google Scholar]
- Maryon-Davis A (2005) Weight management in primary care: how can it be made more effective? Proceedings of the Nutrition Society 64(1): 97–103. [DOI] [PubMed] [Google Scholar]
- McAlearney AS, Hefner JL, Sieck C, et al. (2015) Fundamental issues in implementing an ambulatory care electronic health record. The Journal of the American Board of Family Medicine 28(1): 55–64. [DOI] [PubMed] [Google Scholar]
- McGaffey A, Abatemarco DJ, Jewell IK, et al. (2011) Fitwits MD™: an office-based tool and games for conversations with 9- to 12-year-old children about obesity. Journal of the American Board of Family Medicine 24(6): 768–771. [DOI] [PubMed] [Google Scholar]
- Miller WL, Crabtree BF, Nutting PA, et al. (2010) Primary care practice development: a relationship-centered approach. Annals of Family Medicine 8(Suppl 1): S68–S79; S92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE) (2014) Obesity: guidance on prevention, identification, assessment and management of overweight and obesity in adults and children. London (UK) Available at: https://www.nice.org.uk/guidance/cg189 (accessed 30 March 2018). [Google Scholar]
- Ogden CL, Carroll MD, Lawman HG, et al. (2016) Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. The Journal of the American Medical Association 315(21): 2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkin P, Gorber SC, Shaw E, et al. (2015) Recommendations for growth monitoring, and prevention and management of overweight and obesity in children and youth in primary care. Canadian Medical Association Journal 187(6): 411–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrin EM, Flower KB, Garrett JG, et al. (2005) Preventing and treating obesity: pediatricians’ self-efficacy, barriers, resources, and advocacy. Ambulatory Pediatrics 5: 150–156. [DOI] [PubMed] [Google Scholar]
- Polacsek M, Orr J, Letourneau L, et al. (2009) Impact of a primary care intervention on physician practice and patient and family behavior: keep ME healthy – the Maine youth overweight collaborative. Pediatrics 123(Suppl 5): S258–S266. [DOI] [PubMed] [Google Scholar]
- Pomietto M, Docter AD, Van Borkulo B, et al. (2009) Small steps to health: building sustainable partnerships in pediatric obesity care. Pediatrics 123(5): S308–S316. [DOI] [PubMed] [Google Scholar]
- Pulgarón ER (2013) Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clinical Therapeutics 35: A18–A32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rattay KT, Ramakrishman M, Atkinson A, et al. (2009) Use of an electronic medical record system to support primary care recommendations to prevent, identify, and manage childhood obesity. Pediatrics 123: S100–S107. [DOI] [PubMed] [Google Scholar]
- Sanders LM, Perrin EM, Yin HS, et al. (2014) ‘‘Greenlight study’’: a controlled trial of low-literacy, early childhood obesity prevention. Pediatrics 133(6): e1724–e1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebelius K (2014) Report to Congress on Preventive Services and Obesity-related Services Available to Medicaid Enrollees. Available at: https://www.medicaid.gov/medicaid/quality-of-care/downloads/rtc-preventive-obesityrelated-services2014.pdf (accessed 30 March 2018).
- Skelton JA, Demattia LG and Flores G (2008) A pediatric weight management program for high risk populations: a preliminary analysis. Obesity 16(7): 1698–1701. [DOI] [PubMed] [Google Scholar]
- Skinner AC, Perrin EM, Moss LA, et al. (2015) Cardiometabolic risks and severity of obesity in children and young adults. New England Journal of Medicine 373(14): 1307–1317. [DOI] [PubMed] [Google Scholar]
- Spear BA, Barlow SE, Ervin C, et al. (2007) Recommendations for treatment of child and adolescent over-weight and obesity. Pediatrics 120(suppl 4): S254–S288. [DOI] [PubMed] [Google Scholar]
- Spivack JG, Swietlik M, Alessandrini E, et al. (2010) Primary care providers’ knowledge, practice, and perceived barriers to the treatment and prevention of childhood obesity. Obesity 18(7): 1341–1347. [DOI] [PubMed] [Google Scholar]
- Staiano A, Marker A, Liu M, et al. (2017) Childhood obesity screening and treatment practices of pediatric healthcare providers. The Journal of Louisiana State Medical Society 169(1): 2–10. [PMC free article] [PubMed] [Google Scholar]
- Staniford LJ, Breckon JD, Copeland JC, et al. (2011) Key stakeholders’ perspectives towards childhood obesity treatment: a qualitative study. Journal of Child Health Care 15(3): 230–244. [DOI] [PubMed] [Google Scholar]
- Steele RG, Aylward BS, Jensen CD, et al. (2012) Comparison of a family-based group intervention for youths with obesity with a brief individual family intervention: a practical clinical trial of positively fit. Journal of Pediatric Psychology 37(1): 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taveras EM, Marshall R, Kleinman KP, et al. (2015) Comparative effectiveness of childhood obesity interventions in pediatric primary care: a cluster-randomized clinical trial. The Journal of the American Medical Association Pediatrics 169(6): 535–542. [DOI] [PubMed] [Google Scholar]
- Taveras EM, Perkins M, Anand S, et al. (2017) Clinical effectiveness of the Massachusetts childhood obesity research demonstration initiative among low-income children. Obesity 25(7): 1159–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau (2017) Quickfacts. Available at: https://www.census.gov/quickfacts/FL (accessed 30 March 2018).
- United States Department of Commerce, Bureau of Economic Analysis (2017) Gross Domestic Product by Metropolitan Area, 2016. Available at: https://www.bea.gov/newsreleases/regional/gdp_metro/gdp_metro_newsrelease.htm (accessed 30 March 2018).
- Van Gerwen M, Franc C, Rosman S, et al. (2009) Primary care physicians’ knowledge, attitudes, beliefs and practices regarding childhood obesity: a systematic review. Obesity Reviews 10(2): 227–236. [DOI] [PubMed] [Google Scholar]
- Vine M, Hargreaves MB, Briefel RR, et al. (2013) Expanding the role of primary care in the prevention and treatment of childhood obesity: a review of clinic- and community based recommendations and interventions. Journal of Obesity 2013: 172035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner EH (1998) Chronic disease management: what will it take to improve care for chronic illness? Effective Clinical Practice 1(1): 2–4. [PubMed] [Google Scholar]
- Whitlock EP, O’Connor EA, Williams SB, et al. (2010) Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics 125(2): e396–e418. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Staiano AE, Altman M, et al. (2017) Improving access and systems of care for evidence-based childhood obesity treatment: conference key findings and next steps. Obesity 25: 16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2017) Childhood overweight and obesity. Available at: http://www.who.int/dietphysicalactivity/childhood/en/ (accessed 30 March2018).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


