Abstract
Background:
Alcohol use disorder (AUD) is a costly public health concern; yet, many individuals with AUD never receive formal treatment. Prior studies have identified that “hitting bottom” may be an important factor in seeking treatment for AUD) and the notion that “hitting bottom” is necessary for recovery is commonly portrayed in the popular media. Yet, “hitting bottom” has never been formally operationalized.
Objectives:
The present article aimed to operationalize “hitting bottom.”
Methods:
A multiphase process was used to develop a measure of hitting bottom among individuals experiencing alcohol problems: the Noteworthy Aspects of Drinking Important to Recovery (NADIR). Psychometric evaluation of the measure was conducted using online data collected from individuals who identified as moderate to heavy drinkers (N=597).
Results:
The NADIR included five lower-order dimensions and one higher-order dimension (“hitting bottom”), had strong concurrent validity with measures of alcohol use severity and alcohol-related problems, and was found to have excellent internal consistency reliability (α > 0.90). An overall summary score on the NADIR of 50+ (factor scores>0) differentiated individuals who had previously sought treatment for AUD and reported more excessive alcohol use compared to those with no treatment history and lower levels of alcohol use. Thus, the NADIR with a cutoff of 50 may be a good starting point for future researchers to test as a method to identify individuals who have hit bottom.
Conclusions/Importance:
The NADIR provides a viable operational definition of hitting bottom. Future research should evaluate the predictive validity of the NADIR.
Keywords: hitting bottom, hitting rock bottom, alcohol use disorder, recovery, treatment seeking, treatment outcomes
Introduction
Background
Alcohol use disorder (AUD) is a significant public health problem (World Health Organization (WHO), 2004). Societal and economic costs associated with problematic alcohol use exceed hundreds of billions of dollars worldwide annually (WHO, 2014). Some of the consequences associated with AUD include unemployment, interpersonal conflict, and increased risk of injury and medical problems (WHO, 2004). Interestingly, the majority of individuals with AUD never receive formal treatment (Callaghan et al., 2005; Substance Abuse and Mental Health Services Administration (SAMHSA, 2009). Of those individuals who explicitly felt they needed treatment, the majority chose not to receive treatment for a variety of reasons (e.g., because they did not feel “ready” to stop drinking; SAMHSA, 2009). In order to address disparities in treatment utilization, it is important to understand individual reasons to seek treatment. Further, there is a clear need to develop effective screening tools that may encourage treatment seeking among individuals experiencing problems related to their alcohol use.
In an effort to understand treatment seeking and utilization, many studies have examined factors that are associated with treatment entry. Cunningham and colleagues (2005) found that current heavy drinkers with more severe alcohol problems and greater perceived risk of drinking were more likely to consider changing their alcohol use than individuals with fewer alcohol problems and less perceived risk. Similarly, Cunningham and colleagues (1994) found 10 primary reasons (e.g., external life events, negative experiences associated with chronic alcohol use) for seeking alcohol treatment through a content analysis of interviews with individuals who had successfully resolved an alcohol problem (see Sobell, Sobell, Toneatto, & Leo, 1993 for description of original study). One of the 10 reasons included a term that is common in the addiction treatment vernacular: “hitting rock bottom” (p. 693, Cunningham et al., 1994). The concept of “hitting bottom” has been described for over 50 years, with the term mentioned for the first time in a paper on the treatment of alcohol addiction in 1965, which indicated people must “hit rock bottom” before they may change (British Medical Journal Publishing Group, 1965). Endorsement of “hitting rock bottom” has been identified as an important factor in treatment entry and was also associated with greater treatment compliance (Cunningham et al., 1994). Accordingly, hitting bottom remains a relevant concept for many individuals, yet it has never been operationally defined.
In addition to the consistent relevance of hitting bottom for potential clients, this construct remains relevant in theoretical models that continue to guide addiction research and treatment. For example, the transtheoretical model, which conceptualizes changes in behavior occurring across stages (ranging from precontemplation to maintenance of change), is very consistent with the idea of hitting bottom (TTM; Prochaska, DiClemente, & Norcross, 1992). Previous research has found that experiences of negative consequences from substance use were associated with transitioning from one stage of change into a more motivated stage of change (Życińska, 2006). This finding is congruent with the idea that hitting bottom (e.g., which has often been described in-part as an accumulation of consequences) may be helpful for some clients’ progression through stages of behavior change.
In addition to the alignment of hitting bottom with the TTM, hitting bottom is directly relevant to 12-Step treatment programs, which are prominent recovery models for the general public (Cunningham, Blomqvist, & Cordingley, 2007). The concept of hitting bottom has been widely endorsed as a part of the recovery process by individuals who subscribe to the model of addiction described in 12-step programs (e.g., Alcoholics Anonymous (AA), 2001; Jellinek, 1960). For example, the “Big Book” from AA states that most individuals “have to be pretty badly mangled before they really commence to solve their [alcohol] problems” (p. 43; AA, 2001).
Given the qualitative evidence and theoretical agreement about the importance of hitting bottom as a step in recovery, formally identifying hitting bottom may help individuals who previously chose not to seek treatment to do so. For instance, individuals who may be ambivalent about treatment may use a formal quantitative measure of hitting bottom to objectively evaluate whether or not their drinking warrants treatment. However, the construct of hitting bottom has yet to be defined operationally and has been studied primarily in qualitative surveys or by asking individuals retrospectively whether they had hit bottom or not (see review by Kirouac, Frohe, & Witkiewitz, 2015). This is particularly problematic as hitting bottom may be perceived as an individualized concept, and individuals may not view his or her “bottom” as warranting treatment. Moreover, the concept of hitting bottom among individuals with alcohol problems in the general public (i.e., those not in treatment) has yet to be examined. A quantitative measure operationally defining “bottom” may be useful for evaluating if there is some commonality underlying all individual experiences of hitting bottom, such as a cognitive appraisal that drinking itself is causing problems in life domains. Accordingly, data from individuals not in treatment may be a useful way to examine the construct of hitting bottom through an objective, quantitative lens to allow researchers to fully examine if hitting bottom can be operationalized.
Operationalization of Hitting Bottom Based on Extant Literature and Current Study
In the alcohol research field, “hitting bottom” is a phrase that has been used to describe a tipping point at which an individual decides to change his or her drinking behavior. This tipping point is often conceptualized in-part as a culmination of alcohol-related problems; however, this tipping point of hitting bottom may be different for each individual. For example, one individual may perceive his or her drinking as hitting bottom after losing his or her job, spouse, and home, whereas another individual’s hitting bottom may consist of experiencing serious physical problems caused or exacerbated by alcohol use (e.g., liver cirrhosis) that lead the individual to feel a need to change his or her drinking behavior. “Hitting bottom” is a term used to describe a multidimensional, individualized construct that can range from a “high bottom” to a “low bottom” and may be comprised of various components (see Kirouac et al., 2015 for narrative review of historical evolution of conceptualizations of “hitting bottom”). Such components may include: social networks; physical, mental, and emotional health problems; existential issues; situational and environmental factors; and cognitive appraisal (Kirouac et al., 2015).
Hitting bottom is a concept that may include alcohol-related problems but also extends much further to include aspects of the impact of alcohol use (e.g., cognitive appraisal) that are not assessed in current measures of alcohol-related consequences. Having a quantitative measure of hitting bottom is important to address these gaps in the literature. The aim of the present study was to operationalize the construct of hitting bottom by developing and then empirically examining the psychometric properties of a self-report measure designed to measure hitting bottom. Specifically, the present study goals were to develop a questionnaire tapping the construct of hitting bottom, evaluate the construct validity of the measure via factor analysis, to evaluate the concurrent validity of the measure with existing measures that might be related to hitting bottom (e.g., alcohol-related problems), and to evaluate the internal consistency reliability of the measure.
Method
Measures
Hitting Bottom.
The measure for assessing hitting bottom was developed in a multiphase process that included an extensive literature review, qualitative analyses, and expert consensus.
Step 1: Literature Review.
The first step of measurement development consisted of a literature review for terms relevant to hitting bottom and recovery. Search terms listed in Table 1 were subjected to a systematic literature search using PsycInfo, Web of Science, Google, Google Scholar, and PubMed. Scholarly results from these searches were included if they were written in English, peer-reviewed, and involved human subjects research. Relevant materials included in this review included both scholarly articles as well as materials from non-academic resources (e.g., blogs) to gather a wide representation of how hitting bottom has been conceptualized. Results from these sources were synthesized to identify commonly reported themes that may be important to the operationalization of hitting bottom and the processes underlying recovery more broadly.
Table 1.
Search Terms for Literature Review for NADIR Measurement Development
| “rock bottom” |
| “hit bottom” |
| “high bottom’’ |
| “tipping point”‘‘ AND alcohol |
| “tipping point” AND addiction |
| “tipping point” AND substance use |
| “tipping point” AND substance abuse |
| “tipping point” AND drugs |
| “behavior change” AND alcohol |
| “behavior change” AND addiction |
| “behavior change” AND substance use |
| “behavior change” AND substance abuse |
| “behavior change” AND drugs |
| “reasons for behavior change” AND alcohol |
| “reasons for behavior change” AND addiction |
| “reasons for behavior change” AND substance use |
| “reasons for behavior change” AND substance abuse |
| “reasons for behavior change” AND drugs |
| “mechanisms of behavior change” AND alcohol |
| “mechanisms of behavior change” AND addiction |
| “mechanisms of behavior change” AND substance use |
| “mechanisms of behavior change” AND substance abuse |
| “mechanisms of behavior change” AND drugs |
| “positive life events” AND “behavior change” AND alcohol |
| “positive events” AND “behavior change” AND alcohol |
| “negative events” AND “behavior change” AND alcohol |
| motivation AND “behavior change” AND alcohol |
| “readiness to change” AND alcohol |
| “eliciting change talk” |
| “spontaneous remission” AND alcohol |
| “self-help” AND “behavior change”‘‘ AND alcohol |
| “cognitive appraisal” OR “cognitive evaluation” AND alcohol AND “behavior change” |
| “resiliency” AND alcohol AND “behavior change” |
| “loss of control” AND alcohol AND “behavior change” |
| “locus of control” AND alcohol AND “behavior change” |
| snowball AND alcohol AND “behavior change” |
| “escalation of problems” AND alcohol AND “behavior change” |
| “treatment seeking factors” AND alcohol |
| “help-seeking” AND alcohol AND “behavior change” |
| “subjective evaluation” AND alcohol AND “behavior change” |
| “re-evaluation” AND alcohol AND “behavior change” |
| “ambivalence resolution” AND alcohol AND “behavior change” |
| “functional significance” AND alcohol AND “behavior change” |
| “rock bottom” AND “recovery” |
| “rock-bottom concept” (in Psychology) |
| “rock-bottom concept” (in Addictions) |
| “hitting bottom in addictions” |
| “define hitting bottom” |
| “rock bottom” in addiction |
| historical evolution of the concept of “rock bottom” |
| “rock bottom” AND “addiction history” |
| “spontaneous remission” |
| “Benjamin Rush” |
| “Jellinek” |
| “The Oxford Group” |
Step 2: Qualitative Analyses.
In addition to the literature review described above, efforts were undertaken to further allow for public perceptions of hitting bottom. Specifically, qualitative analyses were conducted using content analysis of recovery success stories from QuitAndRecovery.org. QuitAndRecovery.org is a website “dedicated to learning from success in addiction recovery” that allows individuals to share their personal recovery stories with others. Such stories were analyzed for thematic content, such as “family problems,” to identify the various themes that arose in recovery stories and their relative frequency.
Next, a small sample of undergraduate students at a southwestern university (N=75) were surveyed via part of a larger online data collection project (see Brown and colleagues (2015) for a full description of the parent study). Qualitative data from these participants were collected to include an additional perspective on recovery and hitting bottom that may not be conflated with personal experience with recovery. Participants were an average age of 20.3 (SD=5.1), 72.0% were female, 57.3% Caucasian, 12.0% American Indian or Alaska Native, 12.0% Asian, 2.7% Black or African American, 1.3% Native Hawaiian or Pacific Islander, 12.0% self-identified as “other” race (with multiple responses allowed for race), and 49.3% identified as Hispanic. Two open-ended items assessed participants’ thoughts on the essential components for triggering help-seeking and the essential components of hitting bottom for individuals with alcohol problems: (a) “what things are the biggest reasons people decide to get help with or change their alcohol use?” (with responses to this item thought to reflect general recovery processes); and (b) “what things do you think it takes for someone to ‘hit bottom’?” (with responses to this item thought to reflect the process of hitting bottom).
Data from these participants were analyzed using a hybrid content analysis approach that combined top-down and grounded-theory approaches to use both literature-derived hypotheses and participant responses for content codes (Ryan & Bernard, 2003). Responses were coded by two raters and interrater reliability was assessed using SPSS 21 (κ=0.92 for general recovery; κ=0.88 for hitting bottom responses), and indicated 92.3% and 88.4% agreement among raters, respectively (Cohen, 1960). Procedures were approved by the Institutional Review Board (IRB) of the participating university. Results from Steps 1 and 2 were synthesized and overlapping domains were identified as relevant to the construct of hitting bottom. Preliminary question items were then written to assess each identified domain.
Step 3: Expert Consensus.
The preliminary measure of hitting bottom was next sent electronically to individuals who were identified as content “experts” based on the Step 1 literature review. Specifically, we identified 26 experts in the research and treatment of AUD and other substance use disorder (SUD), of whom nine experts (n=9; 11% female; 34.6% response rate) provided feedback via email and online survey response regarding the rewording of some items of the initial measure as well as a recommendation to add a previously unassessed potential facet of hitting bottom: change in role obligation (e.g., “new role obligations interfere with my drinking”). Overall, experts agreed with the conceptualization of hitting bottom as portrayed in the items of the initial measure.
Using the three steps described above, we created the Noteworthy Aspects of Drinking Important to Recovery (NADIR). The initial version of the NADIR was a 114-item measure that assessed hitting bottom across multiple domains: family problems, social pressure and support, physical health problems, psychological and emotional problems, employment/financial/housing problems, legal problems, identity and values conflict, spiritual change, cost-benefit analysis, loss of control, traumatic “key” events, positive “key” events, motivation/self-efficacy, role-obligation changes, cognitive appraisal of drinking’s influence, and importance of considering changes in drinking one’s drinking. Thus, the NADIR was conceptualized as a higher-order factor model including an overall “hitting bottom” factor and several domain sub-factors. All items had ordered-categorical response options ranging from 0 to 3 (“false,” “somewhat true,” “mostly true,” “definitely true”) in order to have a response gradient with a true zero value. An even number of response options was selected to have forced-choice (i.e., respondents could not select a middle/neutral option). Literacy and reading levels were less than 8th-grade levels as recommended for scale development (DeVellis, 2012; Holmbeck & Devine, 2009).
Drinking Severity Measures.
In addition to basic demographic data, participants were asked to respond to measures of drinking intensity and alcohol-related consequences. Specifically, a version of the Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985) was used to assess how many standard drinks (e.g., one 12-ounce can or bottle of beer) participants consumed for each day of the week and over how many hours for a “typical” drinking week and the “heaviest” or “peak” drinking week for the past 30 days. The Short Inventory of Problems (SIP-2L; Miller, Tonigan, & Longabaugh, 1995) is a 15-item, dichotomous (i.e., “yes” or “no”) assessment of alcohol-related consequences. Alcohol-related consequences also were assessed via the 10-item Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993). Internal consistency of the SIP and AUDIT in the current sample were α=0.90 and α=0.87, respectively. These assessments were administered to examine if participants who self-identified as “moderate to heavy drinkers” also endorsed problematic alcohol consumption and related consequences. Additionally, these measures were administered to evaluate the concurrent validity of the NADIR with existing measures of problematic alcohol use since hitting bottom is partly comprised of alcohol-related problems.
Participants were also asked to complete a treatment history form that assessed for any lifetime history of treatment attendance for substance use problems, including: 12-step meetings (e.g., AA meetings), individual counseling/therapy, inpatient treatment, intensive outpatient treatment, aftercare, relapse prevention groups, medications, and other treatment specifically related to drinking. Due to scarcity of data in any of the individual treatment categories, data on the treatment history form were dichotomized as having any lifetime drinking treatment history or not.
Participants
Data in the present study were collected via web-based assessment. Participants (N=601) were recruited from two primary sources: Amazon Mechanical Turk (MTurk; Buhrmester, Kwang, & Gosling, 2011) and Craigslist. MTurk is an online survey system for recruiting and surveying participants who are registered with the MTurk system. Craigslist is an online forum where jobs and volunteer opportunities, such as completing an online survey, can be advertised. MTurk and Craigslist provide an opportunity for a nationally representative sample of individuals to self-select to take an online survey. Participants recruited from both MTurk and Craigslist were eligible if they were at least 18 years old, reportedly understood English, consumed alcohol in the past 30 days, and identified themselves as a current “moderate to heavy drinker.” Four of the participants had nearly all incomplete data (i.e., > 90% missing data for the NADIR) and were removed from the present analyses for a total of 597 participants with relatively complete data. Of the 597 individuals available for analysis, 196 were recruited from MTurk at a reimbursement rate of up to $1.50 per respondent. The majority of participants (n=401) were recruited from Craigslist in major cities across the United States and were entered into a raffle to win $25 or $100 gift card prizes. The cities for the nationwide Craigslist ad were selected based on the study sites from two large randomized clinical trials for AUD, the COMBINE Study and Project MATCH (Anton et al., 2006; Project MATCH Research Group, 1998) and included Albuquerque, NM; Boston, MA; Charleston, SC; Houston, TX; Philadelphia, PA; Los Angeles, CA; Miami, FL; and Seattle, WA. Participant demographics and drinking measures are described in Table 2. All participants provided electronic consent to participate and all data collection procedures were approved by the Institutional Review Board of the home institution.
Table 2.
Participant Demographics and Drinking Severity (N = 597)
| Demographics/Drinking Severity | Total Sample (N = 597) M (SD) or N (%) |
MTURK (n = 196) M (SD) or N (%) |
Craigslist (n = 401) M (SD) orN (%) |
|---|---|---|---|
| Age | 31.9 (1 0.5) | 30.8 (8.7) | 32.5 (11.3) |
| Gender | |||
| Male | 287.0 (48.6%) | 116.0 (59.5%) | 171.0 (43.3%) |
| Female | 299.0 (50.7%) | 79.0 (40.5%) | 220 (55.7%) |
| Trans gender | 4.0 (0.7%) | 0.0 (0%) | 4.0 (1.0%) |
| Race | |||
| American Indian or Alaska Native | 14.0 (2.4%) | 5.0 (2.6%) | 9.0 (2.3%) |
| Asian | 22.0 (3.8%) | 13.0 (6.6%) | 9.0 (2.3%) |
| Black or African American | 75.0 (12.8%) | 10.0 (5.1%) | 65.0 (16.7%) |
| White or Caucasian | 402.0 (68.6%) | 154.0 (78.6%) | 248.0 (63.6%) |
| Other | 35.0 (6.0%) | 2.0 (1.0%) | 33.0 (8.5%) |
| Multi-Racial | 37.0 (6.3%) | 12.0 (6.1%) | 26.0 (6.7%) |
| Ethnicity (Hispanic) | 127.0 (21.6%) | 27.0 (14.0%) | 100.0 (25.4%) |
| Typical # of drinks per week | 28.5 (23.0) | 27.4 (19.9) | 29.4 (24.4) |
| Typical # of drinking days per week | 5.0 (2.0) | 5.0 (2.0) | 5.1 (2.0) |
| DDD: typical week | 5.5 (3.7) | 5.5 (3.9) | 5.4 (3.5) |
| Peak # of drinks per week | 37.2 (30.7) | 38.2 (28.4) | 37.6 (32.1) |
| Peak # of drinking days per week | 5.1 (2.2) | 5.3 (2.0) | 5.0 (2.3) |
| DDD: peak week | 6.9 (4.5) | 6.9 (4.7) | 6.9 (4.4) |
| SIP summary score | 7.6 (4.5) | 7.0 (4.2)*a | 8.0 (4.6)*a |
| AUDIT summary score | 17.2 (8.6) | 15.3 (7.7) | 17.7 (8.9) |
Note.
p < 0.05 in one-way ANOVA between sites.
p < 0.05 Levene homogeneity of variance test.
Data Preparation and Analysis
The 114-item original NADIR was created with multiple items hypothesized to measure the same latent construct (e.g., family problems) such that exploratory factor analysis (EFA) and item response theory (IRT) could be used to retain only the strongest items for each latent construct. EFA was used to remove items that contributed weakly to the primary factor and IRT was used to remove items with poor item difficulty and item discrimination for that latent trait (DeVellis, 2012). After eliminating items via EFA and IRT we used confirmatory factor analysis (CFA) to evaluate the fit of the hypothesized higher-order model of hitting bottom.
All models were estimated using Mplus version 7.1 (Muthén & Muthén, 2012). Principal axis factoring (PAF) extraction was used for the EFA. Items in the EFA were specified as categorical and a geomin rotation (an oblique rotation) was used to allow for correlations between factors. We then used the EFA to inform the model tested in the CFA. The number of factors to be estimated in the CFA was based on the change in model fit for each additional factor in the EFA and the Kaiser rule of each factor having an eigenvalue greater than 1.0 (Kaiser, 1960; see Table 3 for eigenvalues). Additionally, we performed parallel analyses for the number of items in each EFA to assure the number of factors extracted did not exceed the number of factors that could be expected by chance alone (see Figure 1; Zwick & Velicer, 1986).
Table 3.
Exploratory Factor Analysis Eigenvalues for Sample Correlation Matrix
| Factor | Eigenvalue |
|---|---|
| 1 | 62.32 |
| 2 | 7.466 |
| 3 | 4.725 |
| 4 | 3.873 |
| 5 | 3.333 |
| 6 | 2.509 |
| 7 | 2.329 |
| 8 | 2.117 |
| 9 | 1.949 |
| 10 | 1.629 |
| 11 | 1.603 |
| 12 | 1.296 |
| 13 | 1.235 |
| 14 | 1.097 |
| 15 | 0.99 |
| 16 | 0.871 |
| 17 | 0.864 |
| 18 | 0.835 |
| 19 | 0.77 |
| 20 | 0.717 |
Figure 1.
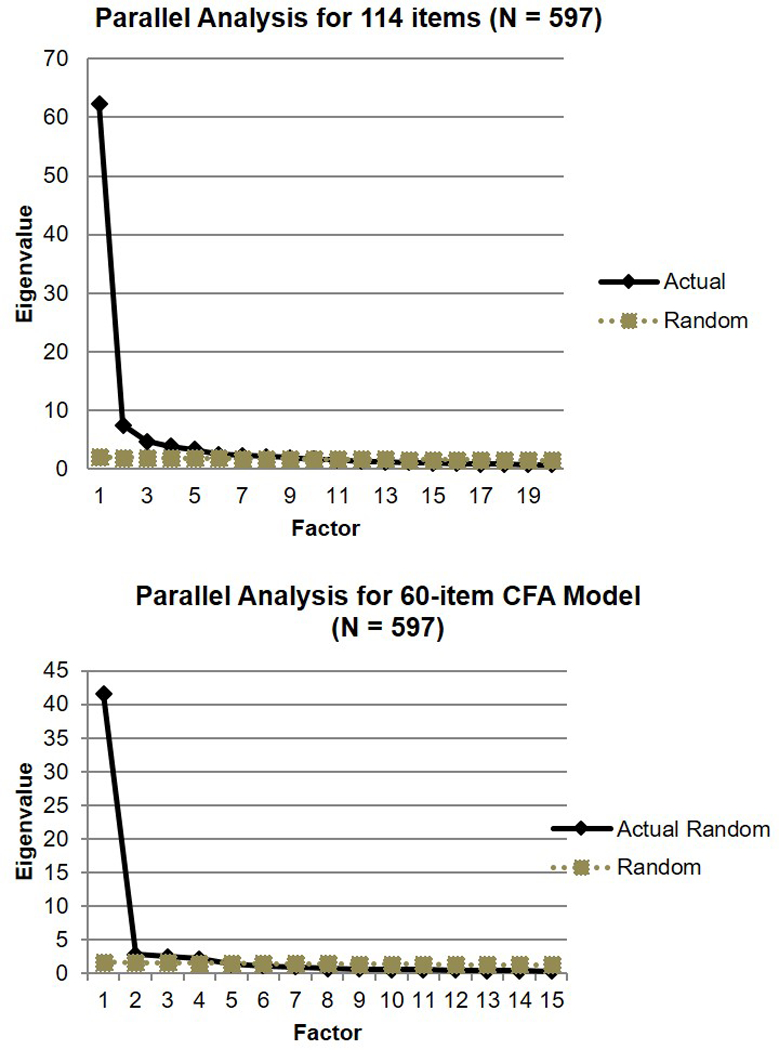
Parallel analyses for the original 114-item NADIR and the reduced model tested via CFA.
To conduct the IRT analyses, response options were dichotomized to either “false” (i.e., 0) or any degree of “true” (i.e., response categories 1, 2, and 3). Next, item characteristic curves (ICCs) were used to judge each item’s discrimination and difficulty and items with poor discrimination and difficulty were removed from the model (see Figure 2). Item discrimination is represented by the slope of the ICC where items with steeper slopes providing greater discrimination of the latent trait. For the present study, poor item discrimination was conceptualized as that item being weakly related to the latent construct of hitting bottom. Item difficulty is how much of a given characteristic is required to endorse an item. In the present study, item difficulty was conceptualized as how severe hitting bottom must be to endorse an item on the NADIR (e.g., “my health has suffered because of my drinking” would have lower item difficulty than “my drinking is killing me”). Items with poor item difficulty would have ICCs located lower or higher along the X-axis of Figure 2, representing items with lower and higher item difficulty. Although items with varying difficulty may indicate various levels of bottom (e.g., “high bottom” versus “low bottom”), items with varying difficulty may also indicate events that occur too commonly (e.g., hangovers) or too rarely (e.g., identity crisis) to be useful. Items endorsed too commonly would fail to distinguish individuals who have hit bottom from individuals who drink without more severe pathology. Items endorsed too rarely would result in empty cells in the matrices examined in latent variable modeling, which could cause non-positive definite matrices (Kline, 2010). Consequently, items with ICCs spread across the X-axis or with slopes that deviated from the majority of items were removed. See Table 4 for list of retained and removed NADIR items.
Figure 2.
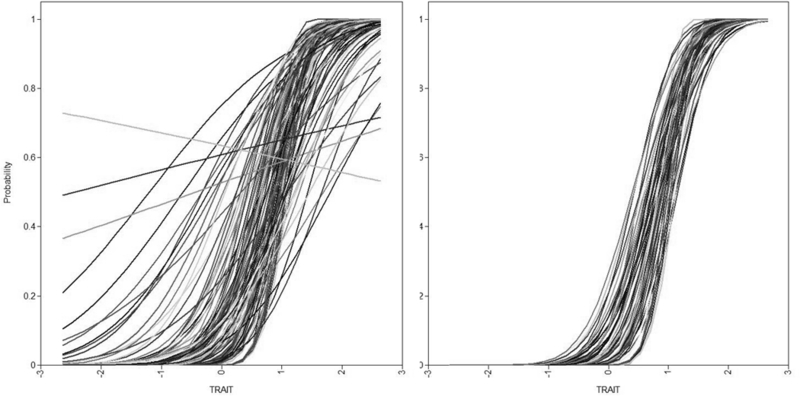
Item Characteristic Curves (ICCs) from IRT analyses: left are the original, 114-item NADIR ICCs; right are the 60-item NADIR ICCs.
Table 4.
114-Item NADIR
| Item | FALSE | Somewhat true |
Mostly true |
Definitely true |
|
|---|---|---|---|---|---|
| 1 | I fight with members of my family because of my drinking. | 0 | 1 | 2 | 3 |
| 2 | Members of my family do not talk to me because of my drinking.a | 0 | 1 | 2 | 3 |
| 3 | I have lost relationships with members of my family because of my drinking. | 0 | 1 | 2 | 3 |
| 4 | My drinking has hurt my family. | 0 | 1 | 2 | 3 |
| 5 | Members of my family tell me they dislike my drinking. | 0 | 1 | 2 | 3 |
| 6 | Members of my family have told me my drinking negatively affects them. | 0 | 1 | 2 | 3 |
| 7 | I am bothered by problems with members of my family caused by my drinking. | 0 | 1 | 2 | 3 |
| 8 | Problems with members of my family make me think about changing my drinking. | 0 | 1 | 2 | 3 |
| 9 | My drinking has made people pressure me to get help. | 0 | 1 | 2 | 3 |
| 10 | As a result of my drinking, people have told me to go to treatment. | 0 | 1 | 2 | 3 |
| 11 | People talk about me needing to go to treatment for my drinking. | 0 | 1 | 2 | 3 |
| 12 | I know my drinking makes people want me to go to treatment. | 0 | 1 | 2 | 3 |
| 13 | People say I need help with my drinking. | 0 | 1 | 2 | 3 |
| 14 | People pressure me to reduce my drinking. | 0 | 1 | 2 | 3 |
| 15 | I am bothered by problems I have with other people regarding my drinking. | 0 | 1 | 2 | 3 |
| 16 | Problems I have with people make me think about changing my drinking. | 0 | 1 | 2 | 3 |
| 17 | My friends and loved ones are supportive of me getting help with my drinking.a | 0 | 1 | 2 | 3 |
| 18 | My friends and loved ones would support me if I got help with my drinking. A | 0 | 1 | 2 | 3 |
| 19 | My friends and loved ones are available and willing to help me reduce my drinking.a | 0 | 1 | 2 | 3 |
| 20 | My friends and loved ones are supportive of me changing my drinking.a | 0 | 1 | 2 | 3 |
| 21 | Support from my friends and loved ones is important to me.a | 0 | 1 | 2 | 3 |
| 22 | Support from my friends and loved ones makes me think about changing my drinking.a | 0 | 1 | 2 | 3 |
| 23 | I know my drinking is making me sick. | 0 | 1 | 2 | 3 |
| 24 | My health has suffered because of my drinking. | 0 | 1 | 2 | 3 |
| 25 | My drinking has made me less healthy than I should be.a | 0 | 1 | 2 | 3 |
| 26 | My drinking is killing me.a | 0 | 1 | 2 | 3 |
| 27 | I’ve been told drinking is bad for my health.a | 0 | 1 | 2 | 3 |
| 28 | A medical professional has told me my drinking is unhealthy for me.a | 0 | 1 | 2 | 3 |
| 29 | My health problems related to my drinking bother me.a | 0 | 1 | 2 | 3 |
| 30 | My health problems make me think about changing my drinking.a | 0 | 1 | 2 | 3 |
| 31 | Because of my drinking, I feel sad more often than not. | 0 | 1 | 2 | 3 |
| 32 | My mental health has suffered because of my drinking. | 0 | 1 | 2 | 3 |
| 33 | Because of my drinking, I struggle to control my emotions. | 0 | 1 | 2 | 3 |
| 34 | My drinking makes me feel mentally ill. | 0 | 1 | 2 | 3 |
| 35 | People have told me that drinking negatively affects my mood. | 0 | 1 | 2 | 3 |
| 36 | People have told me that drinking negatively affects my mental health.a | 0 | 1 | 2 | 3 |
| 37 | My emotional/mental health problems related to my drinking bother me. | 0 | 1 | 2 | 3 |
| 38 | My emotional/mental health problems make me think about changing my drinking. | 0 | 1 | 2 | 3 |
| 39 | My work has suffered because of my drinking. | 0 | 1 | 2 | 3 |
| 40 | My drinking has caused problems with my job. | 0 | 1 | 2 | 3 |
| 41 | I have problems at work because of my drinking. | 0 | 1 | 2 | 3 |
| 42 | I have a lot of debt because of my drinking. | 0 | 1 | 2 | 3 |
| 43 | I have problems with money related to my drinking. | 0 | 1 | 2 | 3 |
| 44 | I spend too much money because of my drinking.a | 0 | 1 | 2 | 3 |
| 45 | I have problems with housing because of my drinking. | 0 | 1 | 2 | 3 |
| 46 | My drinking has caused difficulty in keeping stable housing. | 0 | 1 | 2 | 3 |
| 47 | I am bothered by problems with my job caused by my drinking. | 0 | 1 | 2 | 3 |
| 48 | I am bothered by problems with money caused by my drinking. | 0 | 1 | 2 | 3 |
| 49 | I am bothered by problems with housing caused by my drinking. | 0 | 1 | 2 | 3 |
| 50 | Problems with my job make me think about changing my drinking. | 0 | 1 | 2 | 3 |
| 51 | Problems with money make me think about changing my drinking. | 0 | 1 | 2 | 3 |
| 52 | Problems with housing make me think about changing my drinking. | 0 | 1 | 2 | 3 |
| 53 | I have been aiTested because of my drinking. | 0 | 1 | 2 | 3 |
| 54 | I have had problems with the law because of my drinking. | 0 | 1 | 2 | 3 |
| 55 | My drinking has caused me to engage in illegal behavior.a | 0 | 1 | 2 | 3 |
| 56 | I have gotten in trouble for alcohol-related crimes. | 0 | 1 | 2 | 3 |
| 57 | I am bothered by legal problems my drinking has caused. | 0 | 1 | 2 | 3 |
| 58 | Legal problems make me think about changing my drinking.a | 0 | 1 | 2 | 3 |
| 59 | When I drink, I’m not who I should be. | 0 | 1 | 2 | 3 |
| 60 | I don’t like the person I am when I drink. | 0 | 1 | 2 | 3 |
| 61 | I don’t recognize the person I am when I drink. | 0 | 1 | 2 | 3 |
| 62 | I have compromised my morals when drinking.a | 0 | 1 | 2 | 3 |
| 63 | I have done things against my values (e.g., things I regret) while drinking.a | 0 | 1 | 2 | 3 |
| 64 | I have done things I know are bad while drinking.a | 0 | 1 | 2 | 3 |
| 65 | People have told me I change when I’m drinking.a | 0 | 1 | 2 | 3 |
| 66 | People have told me I am a bad person when I’m drinking. | 0 | 1 | 2 | 3 |
| 67 | I am bothered by the person I am when drinking. | 0 | 1 | 2 | 3 |
| 68 | I think about changing my drinking because of how I feel about the person I become when drinking. | 0 | 1 | 2 | 3 |
| 69 | I have recently experienced spiritual emptiness.a | 0 | 1 | 2 | 3 |
| 70 | I have recently found the power of spirituality.a | 0 | 1 | 2 | 3 |
| 71 | I have recently started going to church or other religious services.a | 0 | 1 | 2 | 3 |
| 72 | I have recently changed my religious or spiritual beliefs.a | 0 | 1 | 2 | 3 |
| 73 | Changes to my spirituality and/or religious beliefs are important to me.a | 0 | 1 | 2 | 3 |
| 74 | Changes in my spirituality make me think about changing my drinking.a | 0 | 1 | 2 | 3 |
| 75 | I’ve thought recently that my alcohol use is more bad than good.a | 0 | 1 | 2 | 3 |
| 76 | I think my drinking causes more problems than it’s worth. | 0 | 1 | 2 | 3 |
| 77 | I have been weighing the pros and cons of my drinking.a | 0 | 1 | 2 | 3 |
| 78 | I have been thinking that my drinking has some advantages and some disadvantages.a | 0 | 1 | 2 | 3 |
| 79 | Thinking of the pros and cons of my drinking bothers me.a | 0 | 1 | 2 | 3 |
| 80 | Thinking of the pros and cons of my drinking makes me think about changing my drinking.a | 0 | 1 | 2 | 3 |
| 81 | My life is out of control because of my drinking. | 0 | 1 | 2 | 3 |
| 82 | I have lost control over my drinking. | 0 | 1 | 2 | 3 |
| 83 | My drinking has made my life uncontrollable. | 0 | 1 | 2 | 3 |
| 84 | My problems are out of my control because of my drinking. | 0 | 1 | 2 | 3 |
| 85 | My life is out of control.a | 0 | 1 | 2 | 3 |
| 86 | I have no control over things.a | 0 | 1 | 2 | 3 |
| 87 | Losing control of things bothers me.a | 0 | 1 | 2 | 3 |
| 88 | Losing control of things makes me think about changing my drinking. | 0 | 1 | 2 | 3 |
| 89 | A bad thing happened that made me realize I need to change my drinking. | 0 | 1 | 2 | 3 |
| 90 | Something bad happened that changed the way I see my drinking. | 0 | 1 | 2 | 3 |
| 91 | There is a clear moment I can think of that was so bad it made me seriously think about my drinking. | 0 | 1 | 2 | 3 |
| 92 | One bad event has made me think about reducing my drinking. | 0 | 1 | 2 | 3 |
| 93 | I am bothered by at least one bad event that has really impacted me.a | 0 | 1 | 2 | 3 |
| 94 | At least one bad event has made me think about changing my drinking. | 0 | 1 | 2 | 3 |
| 95 | Something good has happened that made me realize I should change my drinking.a | 0 | 1 | 2 | 3 |
| 96 | A positive change in my life has changed the way I think about my <hinking.a | 0 | 1 | 2 | 3 |
| 97 | Something good has recently changed my life.a | 0 | 1 | 2 | 3 |
| 98 | Something recently happened that was so good it has changed the way I see my drinking.a | 0 | 1 | 2 | 3 |
| 99 | At least one good event has become important to me.a | 0 | 1 | 2 | 3 |
| 100 | At least one good event has made me think about changing my drinking.a | 0 | 1 | 2 | 3 |
| 101 | I really want to change my drinking. | 0 | 1 | 2 | 3 |
| 102 | I have a lot of reasons to change my drinking. | 0 | 1 | 2 | 3 |
| 103 | I feel ready to change my drinking.a | 0 | 1 | 2 | 3 |
| 104 | If I tried, I would be able to reduce my drinking.a | 0 | 1 | 2 | 3 |
| 105 | I can change my drinking for good.a | 0 | 1 | 2 | 3 |
| 106 | I would be able to reduce my drinking if I wanted to.a | 0 | 1 | 2 | 3 |
| 107 | Being motivated to change my drinking is important to me.a | 0 | 1 | 2 | 3 |
| 108 | Being motivated to change my drinking would help me think about changing my drinking.a | 0 | 1 | 2 | 3 |
| 109 | Feeling confident that I could change my drinking is important to me.a | 0 | 1 | 2 | 3 |
| 110 | Feeling confident that I could change my drinking would help me think about changing my drinking.a | 0 | 1 | 2 | 3 |
| 111 | New role obligations interfere with my drinking.a | 0 | 1 | 2 | 3 |
| 112 | Drinking no longer fits in my life.a | 0 | 1 | 2 | 3 |
| 113 | A challenge in my life makes it necessary to change my drinking.a | 0 | 1 | 2 | 3 |
| 114 | Things in my life are not the same now, so I am forced to change my drinking.a | 0 | 1 | 2 | 3 |
Note. Instructions to participants are: “Please indicate how true you feel each of the following statements is for you right now.”
Indicates this item was removed after IRT-driven factor analyses.
Results from the EFA and IRT and the hypothesized components of hitting bottom informed the selection of items and the factor structure for the CFA. The CFA, shown in Figure 3, was estimated with categorical items of the NADIR as indicators of the five lower-order factors, which were estimated as indicators of a higher-order “hitting bottom” factor. Model parameters were estimated using a weighted least squares means and variances (WLSMV) estimator with Delta parameterization. Model fit of the CFA was evaluated using the root mean square error of approximation (RMSEA), the comparative fit index (CFI), and Tucker-Lewis index (TLI). Models were considered to provide an adequate fit to the data with RMSEA < 0.08 (Browne & Cudeck, 1993) and CFI > 0.90 (Bentler, 1990).
Figure 3.
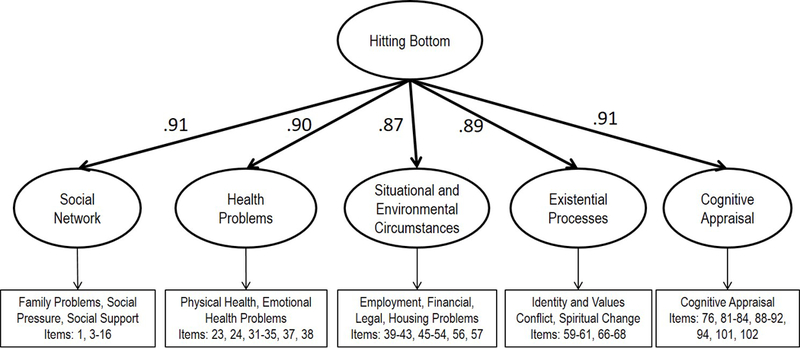
Visual representation of the final factor solution from CFA analyses and original item numbering (χ2 (245) = 6539.549, p < 0.001; RMSEA = 0.069 (90% CI: 0.067, 0.071; CFI = 0.962; TLI = 0.960).
Results
Preliminary Analyses
Descriptive analyses indicated the overall sample drank an average of 28.5 drinks on a typical week and 37.2 on a heavy drinking week with an average of approximately 5 drinking days per week for both typical and heavy drinking weeks (see Table 2). Moreover, the average summary SIP score was 7.6 out of 15 alcohol-related consequence items, indicating the overall sample experienced a number of alcohol-related consequences. This finding is similar to the overall average AUDIT summary score of 17.2, which was more than twice the summary score of 8 that is considered indicative of hazardous alcohol use (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001) and over the summary score of 16 that is considered indicative of a high level of alcohol problems (Miller, Zweben, DiClemente, & Rychtarik, 1992). Overall, 38% of participants reported at least some type of treatment related to their drinking during their lifetime. Accordingly, the overall sample appeared to be representative of individuals experiencing a number of alcohol-related problems and who were engaging in heavy alcohol use. Moreover, 84.4% (n=504) of the present sample reported that hitting bottom was helpful for at least some individuals in their recovery, indicating the hitting bottom remains a relevant concept among individuals with problematic alcohol use.
Exploratory Factor Analyses and Item Response Theory Models
First, a preliminary EFA was conducted to examine the possible number of factors comprising the 114 item NADIR that was initially developed based on the literature review, qualitative data collection, and expert consensus. Factors 1–14 yielded eigenvalues > 1.0 (see Table 3). Parallel analysis of a 114-item measure with N=597 (see Figure 1) suggested ten or more factors would be found due to chance alone, so models that contained more than nine primary factors were not considered for the following analyses.
Results from the EFA also suggested a single factor (with eigenvalue=62.32) was largely driving the measure (see eigenvalues in Table 3). The first factor eigenvalue suggested that most of the variance was explained by one dimension and thus unidimensionality, a requirement of IRT, was assumed. We then used IRT analyses to remove items whose ICCs deviated from the majority of the items (see Figure 2 for before and after ICCs). Based on these ICCs, we removed 54 items, leaving 60 of the original 114 items.
Confirmatory Factor Analyses
With the remaining 60-items, we tested a CFA model that was based on the hypothesized conceptualization of the NADIR. Specifically, we conceptualized the various domains of the NADIR as comprising the factors and tested a model with five primary factors (labeled social network, health problems, situational and environmental circumstances, existential issues, and cognitive appraisal) and one higher-order factor for the NADIR (conceptualized as a higher-order factor for “hitting bottom”). Results from the CFA suggested this model provided adequate fit to the observed data based on RMSEA, CFI and TLI (χ2 (245)=6539.549, p < 0.001; RMSEA=0.069 (90% CI: 0.067, 0.071); CFI=0.962; TLI=0.960). See Figure 3 for a visual representation of this model. See Table 5 for factor loadings.
Table 5.
Final 60-Item NADIR Used in Final CFA Model, with Factor Loadings
| Item | Social network |
Health problems |
Situation Environ. |
Existential issues |
Cognitive appraisal |
||
|---|---|---|---|---|---|---|---|
| 1 | I fight with members of my family because of my drinking. | 0.913 | |||||
| 2 | I have lost relationships with members of my family because of my drinking. | 0.897 | |||||
| 3 | My drinking has hurt my family. | 0.937 | |||||
| 4 | Members of my family tell me they dislike my drinking. | 0.885 | |||||
| 5 | Members of my family have told me my drinking negatively affects them. | 0.92 | |||||
| 6 | I am bothered by problems with members of my family caused by my drinking | 0.92 | |||||
| 7 | Problems with members of my family make me think about changing my | 0.873 | |||||
| 8 | My drinking has made people pressure me to get help. | 0.945 | |||||
| 9 | As a result of my drinking, people have told me to go to treatment. | 0.96 | |||||
| 10 | People talk about me needing to go to treatment for my drinking. | 0.98 | |||||
| 11 | I know my drinking makes people want me to go to treatment. | 0.955 | |||||
| 12 | People say I need help with my drinking. | 0.95 | |||||
| 13 | People pressure me to reduce my drinking. | 0.876 | |||||
| 14 | I am bothered by problems I have with other people regarding my drinking. | 0.928 | |||||
| 15 | Problems I have with people make me think about changing my drinking. | 0.93 | |||||
| 16 | I know my drinking is making me sick. | 0.88 | |||||
| 17 | My health has suffered because of my drinking. | 0.855 | |||||
| 18 | Because of my d1inking, I feel sad more often than not. | 0.904 | |||||
| 19 | My mental health has suffered because of my drinking. | 0.924 | |||||
| 20 | Because of my drinking, I struggle to control my emotions. | 0.906 | |||||
| 21 | My drinking makes me feel mentally ill. | 0.923 | |||||
| 22 | People have told me that drinking negatively affects my mood. | 0.905 | |||||
| 23 | My emotional/mental health problems related to my drinking bother me. | 0.924 | |||||
| 24 | My emotional/mental health problems make me think about changing my drinking | 0.922 | |||||
| 25 | My work has suffered because of my drinking. | 0.911 | |||||
| 26 | My drinking has caused problems with my job. | 0.954 | |||||
| 27 | I have problems at work because of my drinking. | 0.954 | |||||
| 28 | I have a lot of debt because of my drinking. | 0.916 | |||||
| 29 | I have problems with money related to my drinking. | 0.907 | |||||
| 30 | I have problems with housing because of my drinking. | 0.972 | |||||
| 31 | My drinking has caused difficulty in keeping stable housing. | 0.978 | |||||
| 32 | I am bothered by problems with my job caused by my drinking. | 0.951 | |||||
| 33 | I am bothered by problems with money caused by my drinking. | 0.913 | |||||
| 34 | I am bothered by problems with housing caused by my drinking. | 0.947 | |||||
| 35 | Problems with my job make me think about changing my drinking. | 0.953 | |||||
| 36 | Problems with money make me think about changing my drinking. | 0.866 | |||||
| 37 | Problems with housing make me think about changing my drinking. | 0.954 | |||||
| 38 | I have been arrested because of my drinking. | 0.955 | |||||
| 39 | I have had problems with the law because of my d1inking. | 0.929 | |||||
| 40 | I have gotten in trouble for alcohol-related crimes. | 0.914 | |||||
| 41 | I am bothered by legal problems my drinking has caused. | 0.847 | |||||
| 42 | When I drink, I’m not who I should be. | 0.897 | |||||
| 43 | I don’t like the person I am when I drink. | 0.923 | |||||
| 44 | I don’t recognize the person I am when I drink. | 0.917 | |||||
| 45 | People have told me I am a bad person when I’m drinking. | 0.946 | |||||
| 46 | I am bothered by the person I am when drinking. | 0.967 | |||||
| 47 | I think about changing my drinking because of how I feel about the person become when drinking. | 0.949 | |||||
| 48 | I think my drinking causes more problems than it’s worth. | 0.857 | |||||
| 49 | My life is out of control because of my d1inking. | 0.983 | |||||
| 50 | I have lost control over my drinking. | 0.93 | |||||
| 51 | My drinking has made my life uncontrollable. | 0.982 | |||||
| 52 | My problems are out of my control because of my drinking. | 0.992 | |||||
| 53 | Losing control of things makes me think about changing my drinking. | 0.894 | |||||
| 54 | A bad thing happened that made me realize I need to change my drinking. | 0.933 | |||||
| 55 | Something bad happened that changed the way I see my drinking. | 0.945 | |||||
| 56 | There is a clear moment I can think of that was so bad it made me seriously think about my drinking. | 0.917 | |||||
| 57 | One bad event has made me think about reducing my drinking. | 0.897 | |||||
| 58 | At least one bad event has made me think about changing my drinking. | 0.871 | |||||
| 59 | I really want to change my drinking. | 0.842 | |||||
| 60 | I have a lot of reasons to change my drinking. | 0.849 |
Psychometrics and Concurrent Validity of Final Measure
The internal consistency of the 60 item measure was excellent (α=0.986). In addition, the internal consistency reliability of the five domain factors was also excellent (social network: α=0.974; health: α=0.947; situational/environmental: α=0.960; existential: α=0.947, cognitive appraisal: α=0.954), as was the internal consistency of the higher-order factor (α=0.986).
Correlations between the factors of the final CFA model with drinking quantity and frequency, SIP scores, and AUDIT scores were all significant (see Table 6), with associations ranging from small correlations to very large correlations (r=0.170 to r=0.827). The situation/environment factor was most strongly correlated with the SIP (r=0.756) and the higher-order NADIR factor was most strongly correlated with the AUDIT (r=0.827) scores. The factors of the NADIR, reported in Table 7, were also highly correlated with one another, showing some construct overlap.
Table 6.
Correlations between Factors and Drinking Variables
| Social network factor |
Health problem factor |
Situation/ Environment factor |
Existential issues factor |
Cognitive appraisal factor |
NADIR factor |
|
|---|---|---|---|---|---|---|
| SIP | .747** | .736** | .756** | .706** | .752** | .748** |
| AUDIT | .795** | .782** | .794** | .731** | .792** | .827** |
| Total drinks per typical week | .456** | .409** | .472** | .369** | .452** | .458** |
| Total drinks per peak week | .410** | .333** | .413** | .297** | .376** | .387** |
| Total # of drinking days: typical week | .280** | .273** | .303** | .219** | .275** | .286** |
| Total # of drinking days: peak week | .191** | .174** | .224* | .170** | .214** | .205** |
| Average drinks per drinking day: typical week | .363** | .314** | .361** | .288** | .366** | .359** |
| Average d1inks per drinking day: peak week | .316** | .259** | .334** | .232** | .295** | .303** |
Note.
p < .01;
p < .05; SIP = Short Inventory of Problems; AUDIT = Alcohol Use Disorder Identification Test
Table 7.
Correlations between Factors
| Social network factor |
Health problem factor |
Situation/ Environment factor |
Existential Issues factor |
Cognitive appraisal factor |
NADIR factor |
|
|---|---|---|---|---|---|---|
| Health problem factor | 0.875 | |||||
| Situation/Environment factor | 0.855 | 0.832 | ||||
| Existential issues factor | 0.84 | 0.857 | 0.812 | |||
| Cognitive appraisal factor | 0.869 | 0.88 | 0.873 | 0.874 | ||
| NADIR factor | 0.947 | 0.947 | 0.921 | 0.931 | 0.957 |
To assist future researchers in empirically identifying a cutoff score to identify individuals who have hit bottom, independent sample t-tests were conducted to compare factor scores and total NADIR summary scores between individuals with and without any treatment history, with or without AUDIT scores > 16 (Miller et al., 1992) and with or without any days in typical and peak drinking weeks > WHO Very High Risk drinking levels (WHO, 2000; Witkiewitz et al., in press). Tables 8–11 present these results, which suggest mean score group differences by treatment history, AUDIT > 16, and WHO Very High Risk drinking levels were significant across all NADIR factor and NADIR summary variables (p < .001). Results suggest an overall NADIR summary score > 50 (factor scores > 0) might identify individuals who have hit bottom.
Table 8.
Independent Samples t-test Results of Average Factor Scores and NADIR Summary Scores Final 60-Item NADIR between individuals with and without Treatment History
| Treatment History | ||||||||
|---|---|---|---|---|---|---|---|---|
| Treatment History |
No Treatment History |
|||||||
| M | SD | n | M | SD | n | 95% FOR Mean Difference |
t(df) | |
| Social Factor Score |
.55 | .76 | 227 | −.22 | .65 | 370 | .66, .88 | 13.17(595)* |
| Health Factor Score |
.47 | .75 | 227 | −.19 | .64 | 370 | .54, .77 | 11.40(595)* |
| Environment Factor Score |
.50 | .72 | 227 | −.11 | .65 | 370 | .50, .73 | 10.72(595)* |
| Existential Factor Score |
.47 | .75 | 227 | −.17 | .66 | 370 | .52, .75 | 10.82(595)** |
| Cognitive Factor Score |
.44 | .75 | 227 | −.16 | .66 | 370 | .48, .71 | 10.40(595)* |
| Hitting Middle Factor Score |
.48 | .68 | 227 | −.17 | .60 | 370 | ,54, .75 | 12.20(595)* |
| NADIR Summary Score |
69.99 | 49.9 | 227 | 27.77 | 33.95 | 370 | 35.46, 48.97 | 12.28(595)* |
two-tailed p < .001
Table 11.
Independent Samples t-test Results of Average Factor Scores and NADIR Summary Scores Final 60-Item NADIR between individuals with and without Peak Week Drinking at or Above WHO Very High Risk
| WHO Very High Risk Drinking Level, Peak Week | ||||||||
|---|---|---|---|---|---|---|---|---|
| ≥WHO Very High Risk |
<WHO Very High Risk |
|||||||
| M | SD | n | M | SD | n | 95% for Mean Difference |
t(df) | |
| Social Factor Score |
.19 | .77 | 402 | -.27 | .73 | 168 | .28, .71 | 5.86(568)* |
| Health Factor Score |
.18 | .75 | 402 | -.27 | .68 | 168 | .28, .74 | 5.86(568)* |
| Environment Factor Score |
.26 | .72 | 402 | -.24 | .69 | 168 | .34, 74 | 5.86(568)* |
| Existential Factor Score |
.19 | .76 | 402 | -.22 | .71 | 168 | .20, .63 | 5.86(568)* |
| Cognitive Factor Score |
.20 | .71 | 402 | -.26 | .71 | 168 | .29, .69 | 5.86(568)* |
| Hitting Middle Factor Score |
.20 | .68 | 402 | -.25 | .66 | 168 | .29, .57 | 5.86(568)* |
| NADIR Summary Score |
50.77 | 47.26 | 402 | 25.00 | 35.40 | 168 | 12.50, 37.60 | 5.86(568)* |
two-tailed p < .001
Discussion
Results from the present study indicated acceptable model fit, high internal consistency and evidence of concurrent validity of a conceptually and empirically driven 60-item measure of hitting bottom, called the NADIR. Specifically, there were five domain factors and one higher-order factor (conceptualized as “hitting bottom”).
Internal consistency reliability of the 60 item NADIR and items loading on each of the factor subscales in the current sample exceeded Cronbach’s α > 0.90. Moreover, each of the six factors in the 60-item NADIR were correlated with drinking quantity and frequency, as well as total SIP and AUDIT scores, demonstrating good concurrent validity since hitting bottom is often conceptualized in-part as an accumulation of alcohol-related problems. Further, average NADIR summary scores > 50 and factor scores > 0 consistently differentiated individuals with versus without treatment history, with versus without AUDIT scores > 16, and with versus without WHO risk levels at or above very high risk. These results provide initial support for the potential validity of the NADIR in identifying those individuals who may be ready to seek treatment and/or could potentially benefit from treatment. These results also suggest a cutoff summary score of 50 and factor scores > 0 across the NADIR factors might be a useful starting point for future researchers to empirically identify and evaluate alternative cutoff values that prospectively predict treatment engagement and treatment success.
Limitations and Strengths
A primary limitation of the current study was the small sample size for measure development. Specifically, Bentler and Chu (1987) suggest a minimum ratio of 5 participants per parameter estimated when examining factor structure. There were 245 parameters estimated in the final model, so a sample size of at least N=1225 would be necessary. However, the N=597 provided initial evidence for the factor structure of the NADIR. Further, some research suggests parameter ratio is less important than overall sample size and a sample of N > 120 has been supported as sufficient for most factor analyses (Little, 2013).
Another limitation of the current study is that web-based data collection restricted the number and length of measures we could administer without overburdening participants. Most notably, we did not examine whether individuals were interested in treatment seeking and we were limited to a single measure of treatment history. We were also limited by a single assessment time point and thus could not assess potential changes in the NADIR over time. Future research should be conducted to include measures of the stages of change identified in the transtheoretical model as well as the full Drinker Inventory of Consequences (DrInC; Miller, Tonigan, & Longabaugh, 1995) rather than the shorter SIP measure used presently.
A final limitation to the present study is the cross-sectional design. As such, cutoff scores cannot be defined since we cannot examine the predictive validity of such scores. The present findings that NADIR summary scores > 50 and factor scores > 0 are preliminary and are simply proposed starting points for future research. These scores should be interpreted cautiously until longitudinal research can be conducted to potentially replicate these findings and assess whether NADIR scores predict treatment seeking, engagement, and/or treatment success.
Despite the above limitations, the present study has numerous strengths. For example, the present study consisted of a demographically diverse sample across multiple cities in the United States. Moreover, participants identified as current “moderate to heavy drinkers” rather than individuals who might identify as “alcoholics” or other labels that fail to capture the heterogeneity of individuals who experience alcohol problems. Accordingly, the present findings may be more generalizable to a variety of individuals who experience alcohol problems. The present study also offers the first attempt at operationalizing a construct that has been used in the addiction treatment literature for over 50 years that has never been formally defined.
Future Directions and Conclusions
The present findings suggest the NADIR is conceptually consistent with hitting bottom and may be an appropriate way to operationally the construct of hitting bottom. Research is needed to evaluate the predictive validity of the NADIR with respect to identifying individuals who are most likely to seek treatment and to determine whether higher scores on this measure of hitting bottom are predictive of better treatment outcomes.
Populations for which this measure could be particularly useful include individuals who do not acknowledge a need for help and who have access to treatment. For example, the NADIR could be used as a screening tool to identify individuals who may be approaching “hitting bottom” and for whom treatment would be recommended. Future research to identify cut points or scores on the NADIR that may identify individuals as having “hit bottom” would be necessary for the further development of the NADIR as a screening tool.
The present study used a variety of methods to develop a measure of hitting bottom, including literature review, preliminary data collection, expert consensus, and measurement administration. Accordingly, the Noteworthy Aspects of Drinking Important to Recovery (NADIR) measure represents a convergence of evidence of what domains comprise the construct of hitting bottom. The factor structure of this measure was largely consistent with the expected components of hitting bottom where social network variables, health problem variables, situational and environmental circumstances, existential issues, and cognitive appraisal of one’s drinking as problematic comprised the factor structure of the measure of hitting bottom. Accordingly, the NADIR represents more than a measure of alcohol-related problems and may allow researchers to evaluate the utility of hitting bottom. After existing for more than a half-century, the complex construct of “hitting bottom” may finally be operationally defined via the NADIR measure.
Table 9.
Independent Samples t-test Results of Average Factor Scores and NADIR Summary Scores Final 60-Item NADIR between individuals with and without AUDIT scores > 16
| ADUIT | ||||||||
|---|---|---|---|---|---|---|---|---|
| AUDIT≤ 16 |
AUDIT≤ 16 |
|||||||
| M | SD | n | M | SD | n | 95% for Mean Difference |
t(df) | |
| Social Factor Score |
.60 | .65 | 302 | −.46 | .50 | 295 | .97, 1.16 | 22.42(595)* |
| Health Factor Score |
.56 | .62 | 302 | −.44 | .50 | 295 | .91, 1.09 | 21.64(595)* |
| Environment Factor Score |
.61 | .59 | 302 | −.38 | .52 | 295 | .90, 7.07 | 21.57(595)* |
| Existential Factor Score |
.55 | .66 | 302 | −.42 | .50 | 295 | .88, 1.06 | 20.21(595)* |
| Cognitive Factor Score |
.57 | .55 | 302 | −.44 | .66 | 295 | .93, 1.10 | 23.19(595)* |
| Hitting Middle Factor Score |
.57 | .55 | 302 | −.43 | .60 | 295 | .92, 10.08 | 24.46(595)* |
| NADIR Summary Score |
.73.78 | 45.09 | 302 | 13.15 | 33.95 | 295 | 55.15, 66.12 | 21.72(595)* |
two-tailed p < .001
Table 10.
Independent Samples t-test Results of Average Factor Scores and NADIR Summary Scores Final 60-Item NADIR between individuals with and without Typical Week Drinking at or Above WHO Very High Risk
| WHO Very High Risk Drinking Level, Typical Week | ||||||||
|---|---|---|---|---|---|---|---|---|
| ≥WHO Very High Risk |
<WHO Very High Risk |
|||||||
| M | SD | n | M | SD | n | 95% for Mean Difference |
t(df) | |
| Social Factor Score |
.27 | .75 | 346 | -.22 | .75 | 238 | .33,.67 | 5.86(582)* |
| Health Factor Score |
.26 | .73 | 346 | -.23 | .69 | 238 | .35,.67 | 6.26(582)* |
| Environment Factor Score |
.32 | .70 | 346 | -.17 | .72 | 238 | .40,.72 | 6.99(582)* |
| Existential Factor Score |
.24 | .73 | 346 | -.17 | .75 | 238 | .29, .62 | 5.44(582)* |
| Cognitive Factor Score |
.28 | .69 | 346 | -.23 | .70 | 238 | .67,.68 | 6.58(582)* |
| Hitting Middle Factor Score |
.27 | .66 | 346 | -.2 | .68 | 238 | .35, 65 | 6.60(582)* |
| NADIR Summary Score |
54.61 | 46.91 | 346 | 27.82 | 38.83 | 238 | 18.45, 37.98 | 5.68(582)* |
two-tailed p < .001
Acknowledgements:
This research was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA; R01-AA022328; PI: Witkiewitz; R21-AA017137; PI: Witkiewitz). MK is supported by a doctoral grant (F31-AA024959; PI: Kirouac) from the NIAAA.
Footnotes
The authors report no conflicts of interest.
References
- Alcoholics Anonymous. (2001). Alcoholics Anonymous, 4th Edition New York: A.A. World Services. [Google Scholar]
- Anton RR, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, … & Zweben A (2006). Combined pharmacotherapies and behavioral interventions for alcohol dependence. Journal of the American Medical Association, 295(17), 2003–2017. doi: 10.1001/jama.295.17.2003 [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). The Alcohol Use Disorders Identification Test: Guidelines for use in primary care (2nd ed.). Geneva: World Health Organization. [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. [DOI] [PubMed] [Google Scholar]
- Bentler P, & Chu C (1987). Practical issues in structural modeling. Sociological Methods and Research, 16(1), 78–117. [Google Scholar]
- British Medical Journal Publishing Group. (1965). Treatment of alcohol addiction. British Medical Journal, 2(5455), 184–185. [PMC free article] [PubMed] [Google Scholar]
- Brown DB, Bravo AJ, Roos CR, & Pearson MR (2015). Five facets of mindfulness and psychological health: Evaluating a psychological model of the mechanisms of mindfulness. Mindfulness, 6, 1021–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit In Bollen KA & Long JS (Eds.), Testing Structural Equation Models (pp. 136–162). Beverly Hills, CA: Sage. [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk: A New Source of Inexpensive, Yet High-Quality, Data? Perspectives on Psychological Science, 6, 3–5. doi: 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Callaghan RC, Hathaway A, Cunningham JA, Vettese LC, Wyatt S, & Taylor L (2005). Does stage-of-change predict dropout in a culturally diverse sample of adolescents admitted to inpatient substance-abuse treatment? A test of the Transtheoretical Model. Addictive Behaviors, 30, 1834–1847. [DOI] [PubMed] [Google Scholar]
- Cohen J (1960). A coefficient agreement for nominal scales. Educational and Psychological Measurement, 20, 37–46. [Google Scholar]
- Collins RL, Parks GA, Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Blomqvist J, & Cordingley J (2007). Beliefs about drinking problems: Results from a general population telephone survey. Addictive Behaviors, 32, 166–169. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Blomqvist J, Koski-Jannes A, & Cordingley J (2005). Current heavy drinkers’ reasons for considering change: Results from a natural history general population survey. Addictive Behaviors, 30, 581–584. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Sobell LC, Sobell MB, & Gaskin J (1994). Alcohol and drug abusers’ reasons for seeking treatment. Addictive Behaviors, 19(6), 691–696. [DOI] [PubMed] [Google Scholar]
- DeVellis RF (2012). Scale Development: Theory and Applications (3rd ed.). Thousand Oaks, CA: SAGE Publications, Inc. [Google Scholar]
- Holmbeck GN, & Devine KA (2009). Editorial: An author’s checklist for measure development and validation manuscripts. Journal of Pediatric Psychology, 34(7), 691–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jellinek EM (1960). The Disease Concept of Alcoholism. New Haven, CT: Hillhouse. [Google Scholar]
- Kaiser HF (1960). The application of electronic computers to factor analysis. Educational and Psychological Measurement, 20, 141–151. [Google Scholar]
- Kirouac M, Frohe T, & Witkiewitz K (2015). Toward the operationalization and examination of “hitting bottom” for problematic alcohol use: A literature review. Alcoholism Treatment Quarterly, 33(2). [Google Scholar]
- Kline RB (2010). Principles and Practice of Structural Equation Modeling (3rd ed.). New York, NY: The Guilford Press. [Google Scholar]
- Little TD (2013). Longitudinal Structural Equation Modeling. New York, NY: Guilford Press. [Google Scholar]
- Miller WR, Tonigan JS, & Longabaugh R (1995). The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse Test manual (Project MATCH Monograph Series, Vol. 4). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC and Rychtarik RG (1992). Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence (Project MATCH Monograph Series, Vol. 2). Rockville MD: National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus users guide (Version 7). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Prochaska JO, DiClemente CC, & Norcross JC (1992). In search of how people change: Applicants to addictive behaviors. American Psychologist, 47(9), 1102–1114. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. (1998). Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism, Clinical and Experimental Research, 22(6), 1300–1311. [DOI] [PubMed] [Google Scholar]
- Ryan GW, Bernard HR (2003). Techniques to Identify Themes. Field Methods, 15(1), 85–109. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption. Addiction, 88(6), 791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Toneatto T, & Leo GI (1993). What triggers the resolution of alcohol problems without treatment? Alcoholism: Clinical and Experimental Research, 17(2), 217–224. doi: 10.1111/j.1530-0277.1993.tb00752.x [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies. (2009). The NSDUH Report: Alcohol Treatment: Need, Utilization, and Barriers. Rockville, MD. [Google Scholar]
- Witkiewitz K, Hallgren KA, Kranlzer HR, Mann KF, Hasin DS, Falk DE, Little RZ, & Anton RF (in press). Clinical validation of reduced alcohol consumption after treatment for alcohol dependence: Using the World Health Organization risk drinking levels. Alcoholism: Clinical and Experimental Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2000). International guide for monitoring alcohol consumption and related harm. Geneva, Switzerland: Author. [Google Scholar]
- World Health Organization (WHO). (2004). Global status report on alcohol 2004. Geneva, Switzerland: Author. [Google Scholar]
- World Health Organization. (2014). Global status report on alcohol and health 2014. Global Status Report on Alcohol, 1–392. http://doi.org//entity/substance_abuse/publications/global_alcohol_report/en/index.html
- Zwick WR, & Velicer WF (1986). Comparison of five rules for determining the number of components to retain. Psychological Bulletin, 99(3), 432–442. doi: 10.1037/0033-2909.99.3.432 [DOI] [Google Scholar]
- Życińska J (2006). Cognitive components and health-related behaviors as predictors in the process of smoking cessation. Polish Psychological Bulletin, 37(2), 101–110. [Google Scholar]


