Abstract
Background Context
The optimal number of visits for the care of cervicogenic headache (CGH) with spinal manipulative therapy (SMT) is unknown.
Purpose
To identify the dose-response relationship between visits for SMT and chronic CGH outcomes; to evaluate the efficacy of SMT by comparison with a light massage control.
Study Design/Setting
Two-site, open-label randomized controlled trial.
Patient Sample
Participants were 256 adults with chronic CGH.
Outcome Measures
The primary outcome was days with CGH in the prior 4 weeks evaluated at the 12- and 24-week primary endpoints. Secondary outcomes included CGH days at remaining endpoints, pain intensity, disability, perceived improvement, medication use, and patient satisfaction.
Methods
Participants were randomized to 4 dose levels of chiropractic SMT: 0, 6, 12, or 18 sessions. They were treated 3 times per week for 6 weeks and received a focused light-massage control at sessions when SMT was not assigned. Linear dose effects and comparisons to the no-manipulation control group were evaluated at 6, 12, 24, 39, and 52 weeks. This study was funded by the National Center for Complementary and Integrative Health (R01AT006330) and is registered at ClinicalTrials.gov (NCT01530321). The authors declare no conflicts of interest.
Results
A linear dose-response was observed for all follow-ups, a reduction of approximately 1 CGH day/4 weeks per additional 6 SMT visits (p<.05); a maximal effective dose could not be determined. CGH days/4 weeks were reduced from about 16 to 8 for the highest and most effective dose of 18 SMT visits. Mean differences in CGH days/4 weeks between 18 SMT visits and control were -3.3 (p=.004) and -2.9 (p=.017) at the primary endpoints, and similar in magnitude at the remaining endpoints (p<.05). Differences between other SMT doses and control were smaller in magnitude (p > .05). CGH intensity showed no important improvement nor differed by dose. Other secondary outcomes were generally supportive of the primary.
Conclusion
There was a linear dose-response relationship between SMT visits and days with CGH. For the highest and most effective dose of 18 SMT visits, CGH days were reduced by half, and about 3 more days per month than for the light-massage control.
Keywords: Cervicogenic headache, Dose-response, Spinal manipulative therapy, Massage, Chiropractic, Randomized controlled trial
Introduction
Headaches are a substantial public health and financial burden on society [1] with over half of the global population experiencing headaches during their lifetimes [2]. Approximately 157 million days of work are lost each year in the US, costing $50 billion in work absenteeism and medical benefits annually [3]. Cervicogenic headache (CGH) is defined as a secondary headache related to a neck disorder [4,5]. The point prevalence ranges from 0.4 to 4.6% [6-8] and is found in up to 18% of the chronic headache population [9].
Many US adults use complementary and integrative health therapies for headache and neck pain [10,11], with spinal manipulative therapy (SMT) among the most common [12]. A growing body literature supports use of SMT for headache including CGH; there has been no other intervention shown to be superior [13-16]. However, there remains little consensus on the appropriate dose of SMT to achieve maximum clinical benefit for CGH [17].
Our group conducted the first pilot randomized trials evaluating the important yet understudied issue of dose-response of SMT [17,18]. These studies had promising clinically important results favoring higher numbers of SMT visits to a chiropractor for short-term pain and disability improvement. We therefore conducted the first full-scale dose-response trial for the purpose of identifying optimal care of CGH with SMT and informing the design of future comparative effectiveness studies. The key hypothesis was that there is a linear relationship between the number of SMT visits and clinical outcomes. Intimately related is an efficacy hypothesis: SMT at selected dose levels is superior to a hands-on control. The trial evaluated the unique effects of SMT compared to a brief light massage which controlled for contextual effects related to the provider-patient interaction [19].
Methods
Design
This study was a two-site, prospective, open-label randomized controlled trial conducted in greater Portland, Oregon and Minneapolis, Minnesota metropolitan regions. The trial protocol has been published elsewhere [20]. We randomized 256 participants with chronic CGH, half at each site, to 1 of 4 dose levels of SMT (Fig. 1). The dosage schedules were informed by pilot study experience and a previous randomized trial on low back pain [17,21]. All participants were scheduled for 18 visits over 6 weeks. Participants were randomly assigned to 0, 6, 12, or 18 visits for SMT (i.e., 0 to 3 per week). They received a brief light massage at all remaining visits to control for provider attention and touch. Follow-up was by headache diary and mailed questionnaire at 6, 12, 24, 39 and 52 weeks. The predetermined primary outcome was days with CGH evaluated with the headache diary. Diaries and questionnaires were completed without any influence by study personnel. Providers had no access to these documents.
Fig. 1.
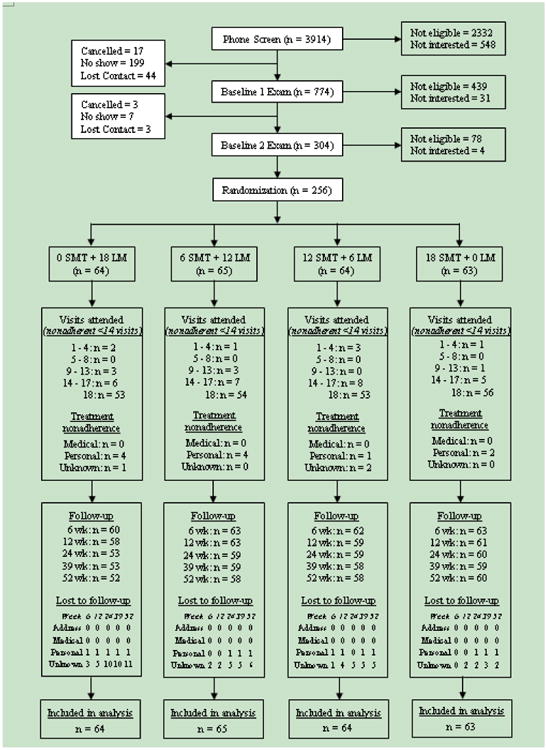
Study flow diagram. All participants were assigned 18 treatment visits. They received either spinal manipulative therapy (SMT) or light-massage control (LM) at any one visit. Under treatment nonadherence, “medical” refers to health conditions and “personal” refers to life events such as moving away or a new job that that interfered with the participant's ability to attend study visits. “Lost to follow-up” indicates missing data at a single time point only.
An adaptive computer-generated rank-minimization scheme was used to allocate eligible participants to study group [22]. The web-based program balanced 7 participant characteristics: CGH days, CGH pain intensity, gender, age, differential confidence in success of SMT and massage control, previous SMT or massage CGH care, and tension-type headache. At each site, one web-based program was used for participants with infrequent migraines and one for participants without migraines. The allocation algorithm was prepared by the study statistician before enrollment, and its administration was conducted after final eligibility screening. Hence, treatment-group assignment was concealed from participants and all study personnel prior to allocation.
Ethical approval and trial registration
Ethical approval was granted by the institutional review boards of the participating institutions: University of Western States (IRB20110127), Northwest Health Sciences University (1-98-10-11), and the University of Minnesota (1408M53163). The trial was registered on ClinicalTrials.gov (NCT01530321) and was monitored by an independent data and safety monitoring board approved by the funder.
Protocol overview
Standardized protocols were established for screening, data collection, and intervention procedures [23-26]. Participants were recruited through mailers, craigslist, local newspapers, provider referrals, Facebook, and local TV station website. Initial screening was conducted by study staff in a telephone interview, followed by eligibility assessment at two baseline visits approximately 4 weeks apart. At the first baseline visit, staff collected informed consent from all participants and administered the baseline questionnaire and diary. Screening exams were conducted by licensed chiropractors with 3 to 30 years of experience and eligibility determined by case conference held by the investigators. Eligibility was confirmed at the second baseline visit by a treating chiropractor, followed by allocation to treatment group by staff entering the balancing variables into the adaptive computer algorithm. Care was provided by licensed chiropractors with 6 to 35 years of clinical experience. Participants were compensated for each treatment visit, mailed questionnaire, and phone interview for a maximum of $600.
Participants
Participants were required to have CGH as defined by the International Headache Society [4,5]. Additional CGH characteristics were a history of at least 3 months, at least 5 headaches in the 4 weeks prior to start of care, a minimum average pain intensity of 3 (0 to 10 scale), and clear temporal sequence linking the source of CGH to the neck. Participants were required to be candidates for SMT indicated by cervical joint tenderness or restricted motion (joint play or end play) [23,27]. They also had to be at least 18 years of age, ambulatory and English literate.
The protocol [20] includes an exhaustive list of exclusion criteria summarized here. Participants were ineligible if they had contraindications to spinal manipulation [23,27], complicating conditions possibly related to clinical outcomes, or other confounding factors. They were excluded for conflicting obligations or inability to meet study requirements, litigation, pregnancy, neck or headache care with SMT/massage/exercise in the prior 3 months or other treatment in the prior 4 weeks from a licensed professional, regular analgesic or corticosteroid use, and other types of headache with the exception of tension-type and occasional migraine (1 per month). Candidates were also excluded for brain or cervical spine surgery in the past 5 years, cancer, spinal pathology, inflammatory arthropathies, anticoagulant conditions, autoimmune disorders, and neurodegenerative disease.
Intervention
The intervention period was 6 weeks. Time-controlled treatment visits of 10 minutes were delivered to approximate chiropractic practice [28]. During the first 5 minutes, the treating chiropractors conducted a brief history and recorded adverse events as defined in our protocol [20]. A hot pack was applied to relax spine musculature. In the second 5-minutes, a brief exam and SMT or the light-massage control were performed. To minimize intervention bias and contextual effects introduced by providers, protocol standardization and provider equipoise (equal enthusiasm) across groups was monitored using office observation by a chiropractor on the study team and participant questionnaire [29]. During the treatment phase, abortive over-the-counter analgesics were permitted, but all other care for CGH was discouraged in the absence of intolerable symptoms. There were no restrictions on care following completion of the 6 weeks of study care.
SMT consisted of manual, high velocity, low amplitude thrust manipulation in the cervical and upper thoracic regions [27]. The specific site of application was determined by brief, standard palpation exam including: cervical global range of motion, palpation of the cervical and upper thoracic spine from occiput to the third thoracic vertebra, and palpation of the paraspinal musculature [23,27]. SMT was conducted at all sites of joint dysfunction (palpatory joint restriction or pain); it was not conducted in the absence of joint dysfunction. Modification of intervention in the form of low velocity, low amplitude mobilization was permitted for older participants and cases of acute exacerbation.
Light massage consisted of gentle effleurage (gliding) and gentle pétrissage (kneading) of the neck and shoulder muscles [27,30]. Treatment was focused on the sight of pain/dysfunction to add credibility. The light massage was gentler and of shorter duration than recommended for therapeutic massage practice [28]. Hence, it was minimalist therapy to control for touch and was not a true sham.
Outcome and baseline variables
The primary outcome was CGH frequency defined as the number of days with CGH in the 4 weeks prior to the 12 and 24-week follow-up. Electronic diaries were administered to participants using a Short Message Service (SMS) or email response (SMS-Track ApS, Denmark, https://www.sms-track.com/). Paper diaries were provided to participants for use as a back-up when the electronic platform was not available. They were also used as the primary diary-data capturing system by participants without or uncomfortable with daily Internet or mobile phone access.
Data were taken from the headache diaries with recall of CGH days reported on the questionnaire used as backup for missing or invalid diary data. The International Headache Society guidelines for randomized trials recommend headache frequency as the appropriate primary outcome for efficacy studies [31]. The primary endpoints were predetermined to be 12 and 24 weeks in order to include a short-term and a long-term primary outcome. CGH frequency evaluated at 6, 39, and 52 weeks were prespecified as secondary outcomes and the baseline value as a covariate for the analysis.
The principal secondary outcome was average CGH pain intensity computed from the daily diary entries for days with cervicogenic headache and using recall backup from the questionnaires. Pain intensity was measured using the reliable and valid 11-point numerical rating scale with anchors no pain (0) and worse possible pain (10) [32]; its use is recommended by the International Headache Society [31]. The headache diaries also included the number of days taking medication for CGH and days with headaches other than cervicogenic in the past 4 weeks.
Other secondary outcomes were evaluated on baseline and follow-up questionnaires. These included the validated Headache Impact test (HIT-6) for headache disability [33], quality of life using the 0 to 100-point visual analog scale from the EuroQol-5D [34,35], and days with neck pain and neck pain intensity evaluated as for CGH. Global improvement was evaluated on a 9-point ordinal scale ranging from symptom free to as bad as could be, while CGH pain improvement was rated on a -10 to +10 numerical rating scale. Improvement ratings have been shown to be reliable and responsive [36]. Satisfaction was monitored with a 7-point Likert scale on certitude of treatment success [37], a 6-point Likert scale ranging from very dissatisfied to very satisfied with care, and a 5-point Likert scale evaluating willingness to seek the same care in the future. Secondary outcomes that will be reported elsewhere include cost-effectiveness and healthcare utilization, cervical kinematics [38], pressure pain thresholds [39], and participants perspectives related to treatment collected via qualitative interviews.
Statistical analysis
The prespecified primary analysis consisted of regression models to identify the adjusted linear effect of SMT dose (slope=mean outcome increment/6 SMT sessions) and adjusted mean differences for comparisons of the SMT groups to the no-SMT control group. The primary and secondary outcomes were regressed at each time point on dose as a continuous variable (slope models) and regressed on a set of 3 indicator variables with the control as the reference group (dose-group comparison models). For the primary outcome only, longitudinal effects across all follow-ups were modeled with generalized estimating equations utilizing independent working correlation structure to account for within-person correlation between time points [40]. All models included as covariates the balancing and stratification variables used in the rank-minimization allocation program.
Intention-to-treat analysis was conducted including all participants in the dose group to which they were originally allocated. Missing data were imputed for the primary analysis using linear interpolation, followed by the last datum carried forward for cases with no subsequent data. Sensitivity analysis was conducted on the primary outcome only. For handling missing data, first the missing data were excluded in a complete-case analysis conducted separately for each follow-up time point as in a previous study [21]. Second, 2 multiple imputation methods, Bayesian regression and predictive mean matching implemented with R package mice [41], were used to address possible bias introduced by some imbalance between treatment and control groups in the use of last datum carried forward. Other sensitivity analyses tested for the presence of site × dose interaction, assessed nonlinear dose effects by comparing the R2 between the linear dose model and the saturated categorical dose model, and treated site as a random effect using linear mixed models.
Responder analysis was conducted for the primary outcome. CGH days was dichotomized using a 30% and a 50% improvement threshold. The first threshold is considered a demarcation for minimal clinically important change [42], while the second threshold is a common measure of important improvement for headache research [31]. Models used the proportion of participants attaining the improvement threshold as the dependent variable and the same independent variables as the primary analysis. Because of failure of the originally stipulated multivariate binomial regression models to converge, ordinary least-squares regression was performed using nonparametric bootstrap (N=4,999 resamples) to calculate confidence intervals and p-values [43].
The sample size (n = 64/group) was determined a priori to yield 80% power to detect a linear effect (slope) of 1.1 CGH days between adjacent doses and 3.5 CGH days between SMT and control group using a two-tailed test at the .05 level of significance and taking into account a 10% dropout rate. The residual standard deviation of 7 headaches used in the sample size simulations was taken from our pilot study [17]. All analyses were conducted using R 3.4.0 (The R Foundation for Statistical Computing, Vienna, Austria, https://www.r-project.org)
Results
Participants were enrolled from October 2012 to August 2015 with the final one-year follow-up collected in August 2016. The study flowchart (Fig. 1) shows that allocation was approximately equal across dose groups and sites. The percentage of participants attending at least 14 of the 18 treatment sessions was between 92% (0 SMT group) and 97% (18 SMT group) and there were no deviations from the protocol in treatments assigned. Some degree of joint dysfunction was identified and manipulation performed on each participant at all SMT visits. Compliance with follow-up data collection was greater than 89% at all time points for the 3 SMT groups. It was comparable in the control group in the short-term, but fell to 82% in the long term starting at 24 weeks. Between 4% and 11% of the follow-up data before imputation were replacement data from the questionnaires.
Additional professional care for CGH from a non-study provider was well balanced across groups with no statistically significant differences between groups at any follow-up time point (p > .05). The median number of visits in the prior 4 weeks was 0 for all groups at all follow-up time points. The overall mean number of visits ranged from 0.3 at 6 weeks to 0.9 at 24 weeks, and the maximum mean difference between groups at each follow-up time point ranged from 0.6 to 0.7 visits in the prior 4 weeks. The mean medication use for CGH during the study was between 3 and 5 days in the prior 4 weeks, and there was no more than a 1-day difference between groups at any follow-uptime point (p > .05).
Baseline characteristics were balanced across groups (Table 1). Most characteristics were also well balanced across the two data collection sites. Exceptions were a greater proportion of participants reporting lost work and had a household income less than $40,000 in Oregon, and a greater proportion were married (or living together) in Minnesota. The mean participant age was 41 years. The majority had any one of the following characteristics: white non-Hispanic, women, college graduate, married or living together, comorbidity, or had previous experience with a study intervention. They reported a mean of 15.6 days per 4 weeks with CGH and 18.3 days per 4 weeks with neck pain. The mean duration of their CGH problem was 7.3 years.
Table 1. Baseline characteristics.
| Oregon | Minnesota | SMT 0 (n = 64) | SMT 6 (n=65) | SMT 12 (n = 64) | SMT 18 (n = 63) | All (n=256) | |
|---|---|---|---|---|---|---|---|
| Sociodemographic information | |||||||
| Age (y) | 37 (12) | 45 (12) | 40 (12) | 40 (12) | 43 (13) | 42 (14) | 41 (13) |
| Female | 95 (74.2%) | 87 (68.0%) | 48 (75.0%) | 45 (69.2%) | 45 (70.3%) | 44 (69.8%) | 182 (71.1%) |
| White non-Hispanic | 104 (81.2%) | 110 (85.9%) | 53 (82.8%) | 58 (89.2%) | 51 (79.7%) | 52 (82.5%) | 214 (83.6%) |
| Married or living together | 66 (51.6%) | 92 (71.9%) | 39 (60.9%) | 34 (52.3%) | 42 (65.6%) | 43 (68.3%) | 158 (61.7%) |
| College graduate | 86 (67.2%) | 85 (66.4%) | 36 (56.2%) | 46 (70.8%) | 41 (64.1%) | 48 (76.2%) | 171 (66.8%) |
| Household income < $40,000 | 62 (48.4%) | 24 (19.2%) | 20 (31.7%) | 30 (46.9%) | 18 (28.6%) | 18 (28.6%) | 86 (34.0%) |
| Smoker | 11 (8.6%) | 10 (7.8%) | 6 (9.4%) | 5 (7.7%) | 5 (7.8%) | 5 (7.9%) | 21 (8.2%) |
| Confidence in treatment success (expectations) | |||||||
| Spinal manipulation (1–7 scale)* | 5.1 (1.1) | 5.0 (1.0) | 5.0 (1.1) | 5.0 (1.0) | 5.2 (1.2) | 5.1 (1.0) | 5.1 (1.1) |
| Light massage ((1–7 scale)* | 4.8 (1.4) | 4.8 (1.2) | 4.9 (1.2) | 4.7 (1.3) | 4.9 (1.4) | 4.8 (1.4) | 4.8 (1.3) |
| Difference (manipulation – light massage) | 0.3 (1.6) | 0.2 (1.2) | 0.1 (1.5) | 0.3 (1.4) | 0.4 (1.5) | 0.3 (1.3) | 0.3 (1.4) |
| Physical activity (Minutes / day) | 86 (106) | 85 (120) | 95 (130) | 69 (85) | 69 (85) | 99 (143) | 85 (113) |
| (Days / wk) | 5.4 (1.5) | 5.2 (1.7) | 5.3 (1.5) | 5.3 (1.6) | 5.4 (1.6) | 5.1 (1.7) | 5.3 (1.6) |
| Previous care for CGH | |||||||
| Chiropractic | 67 (52.3%) | 59 (46.1%) | 29 (45.3%) | 28 (43.1%) | 34 (53.1%) | 35 (55.6%) | 126 (49.2%) |
| Massage | 60 (46.9%) | 46 (35.9%) | 27 (42.2%) | 23 (35.4%) | 31 (48.4%) | 25 (39.7%) | 106 (41.4%) |
| Chiropractic or massage | 77 (60.2%) | 63 (49.2%) | 34 (53.1%) | 30 (46.2%) | 40 (62.5%) | 36 (57.1%) | 140 (54.7%) |
| Headache and neck complaint | |||||||
| Days with CGH ( last 4 wk) | 15.8 (6.7) | 15.3 (6.6) | 15.1 (6.3) | 15.2 (7.2) | 16.2 (6.9) | 15.8 (6.1) | 15.6 (6.6) |
| Average CGH pain intensity (0–10 scale)† | 4.5 (1.1) | 4.5 (1.1) | 4.4 (1.0) | 4.4 (1.0) | 4.5 (1.1) | 4.7 (1.1) | 4.5 (1.1) |
| CGH Duration (y) | 7.9 (8.0) | 6.7 (7.9) | 5.7 (6.4) | 8.1 (9.3) | 8.4 (8.5) | 6.9 (7.1) | 7.3 (7.9) |
| CGH-related disability (36–78)† | 58.7 (4.6) | 56.1 (4.9) | 58.5 (4.6) | 56.0 (5.2) | 57.2 (5.1) | 57.9 (4.4) | 57.4 (4.9) |
| Lost work due to CGH | |||||||
| 1/2 day or more | 69 (53.9%) | 36 (28.1%) | 25 (38.5%) | 26 (40.6%) | 27 (42.9%) | 69 (53.9%) | 105 (41.0%) |
| If yes, days with lost work (last 4 wk) | 2.0 (3.7) | 1.2 (4.3) | 1.4 (3.7) | 1.7 (4.6) | 1.8 (4.1) | 1.4 (3.8) | 1.6 (4.1) |
| Days with non-CGH headaches (last 4 wk) | 2.3 (2.7) | 2.3 (3.0) | 2.3 (3.1) | 2.4 (3.0) | 2.3 (2.4) | 2.2 (3.1) | 2.3 (2.9) |
| Days with neck pain (last 4 wk) | 18.8 (7.2) | 17.9 (7.8) | 19.2 (7.6) | 18.8 (7.2) | 18.2 (8.0) | 17.1 (7.3) | 18.3 (7.5) |
| Average neck pain intensity (0–10 scale)† | 4.6 (1.5) | 4.6 (1.5) | 4.5 (1.5) | 4.5 (1.4) | 4.5 (1.5) | 4.8 (1.5) | 4.6 (1.5) |
| Health Status | |||||||
| Tension Type Headache | 30 (23.4%) | 23 (18.0%) | 14 (21.9%) | 13 (20.0%) | 13 (20.3%) | 13 (20.6%) | 53 (20.7%) |
| Migraine | 31 (24.2%) | 25 (19.5%) | 14 (21.9%) | 15 (23.1%) | 14 (21.9%) | 13 (20.6%) | 56 (21.9%) |
| Lower back problems | 43 (33.6%) | 43 (33.6%) | 19 (29.7%) | 20 (30.8%) | 22 (34.4%) | 25 (39.7%) | 86 (33.6%) |
| Any back problems‡ | 70 (54.7%) | 70 (54.7%) | 37 (57.8%) | 32 (49.2%) | 35 (54.7%) | 36 (57.1%) | 140 (54.7%) |
| Any comorbidity‡ | 90 (70.3%) | 87 (68.0%) | 45 (70.3%) | 39 (60.0%) | 49 (76.6%) | 44 (69.8%) | 177 (69.1%) |
| EuroQol “Health State Today” (0–100 VAS)† | 74.4 (13.7) | 76.7 (13.2) | 74.9 (13.7) | 76.3 (11.3) | 76.1 (13.9) | 74.8 (15.0) | 75.5 (13.5) |
| Days taking medication for CGH (last 4 wk) | 6.3 (4.9) | 6.3 (4.6) | 5.6 (4.5) | 5.9 (4.0) | 6.6 (5.4) | 7.0 (4.8) | 6.3 (4.7) |
SMT, spinal manipulative therapy; CGH, cervicogenic headache; VAS, visual analog scale.
Values are mean (standard deviation) or number (percentage).
Seven-point Likert scale from extremely doubtful (1) to extremely confidence (7) in treatment success.
Lower scores are more favorable with the exception of the EuroQol VAS.
Any back problems includes upper, middle, and lower back. Comorbidity includes any of the following: diabetes or arthritis, back, lung, cardiovascular, gastrointestinal, urinary, gynecological, or prostate problems.
Primary outcome
Reduction in the number of days with CGH was observed in all groups by the end of care and was sustained to 52 weeks following enrollment (Table 2 and Fig. 2). Over this time period, CGH days were reduced by about a third for the control group and by about half, or up to about 8 days per month, for the 18 SMT visits group.
Table 2. Primary outcomes.
|
|
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Observed unadjusted mean (SD) | Slope (95% CI) | Adjusted Mean difference (95% CI) | ||||||||
|
| ||||||||||
| Oregon | Minnesota | SMT 0 | SMT 6 | SMT 12 | SMT 18 | Per 6 SMT sessions | SMT 0 vs SMT 6 | SMT 0 vs SMT 12 | SMT 0 vs SMT 18 | |
| Days with CGH (last 4 wk) | ||||||||||
| 0 wk | 15.8 (6.7) | 15.3 (6.6) | 15.1 (6.3) | 15.2 (7.2) | 16.2 (6.9) | 15.8 (6.1) | ||||
| 6 wk | 12.3 (8.0) | 11.0 (7.9) | 12.5 (8.2) | 12.2 (8.2) | 11.2 (7.5) | 10.6 (8.0) | -0.8 (-1.5, -0.2)* | -0.2 (-2.1, 1.7) | -1.8 (-3.7, 0.2) | -2.3 (-4.2, -0.3)* |
| 12 wk | 10.6 (8.0) | 9.8 (8.2) | 11.2 (7.9) | 11.2 (8.4) | 10.3 (8.7) | 8.1 (7.4) | -1.1 (-1.9, -0.4)* | -0.3 (-2.5, 1.9) | -1.9 (-4.1, 0.4) | -3.3 (-5.6, -1.0)* |
| 24 wk | 10.4 (8.5) | 9.2 (8.0) | 10.8 (8.1) | 10.0 (8.2) | 9.7 (8.7) | 8.6 (8.0) | -1.0 (-1.7, -0.2)* | -0.5 (-2.8, 1.8) | -1.7 (-4.1, 0.6) | -2.9 (-5.2, -0.5)* |
| 39 wk | 9.4 (8.1) | 8.9 (8.1) | 10.2 (8.1) | 9.3 (8.5) | 8.9 (8.1) | 8.2 (7.8) | -0.9 (-1.7, -0.1)* | -0.6 (-3.1, 1.8) | -1.8 (-4.3, 0.6) | -2.6 (-5.1, -0.1)* |
| 52 wk | 9.6 (8.6) | 9.5 (8.4) | 10.6 (8.5) | 10.1 (9.1) | 9.6 (8.7) | 8.2 (7.5) | -1.1 (-1.9, -0.3)* | -0.2 (-2.6, 2.2) | -1.7 (-4.1, 0.7) | -3.2 (-5.6, -0.7)* |
| 6 to 52 wk† | -1.0 (-1.6, -0.4)* | -0.4 (-2.3, 1.6) | -1.8 (-3.8, 0.2) | -2.8 (-4.9, -0.8)* | ||||||
SD, standard deviation; CI, confidence interval; UWS, University of Western States; NWHSU, Northwestern Health Sciences University; SMT, spinal manipulation; CGH, cervicogenic headache.
Primary endpoints were prespecified as days with CGH in the prior 4 weeks evaluated at the 12 and 24-week follow-up. Unadjusted means are from original data without imputation; slopes and mean differences are computed from imputed data and adjusted for baseline covariates.
Negative signs of slopes and risk differences favor higher doses of manipulation.
p<.05.
Longitudinal profile using generalized estimating equations.
Fig. 2.
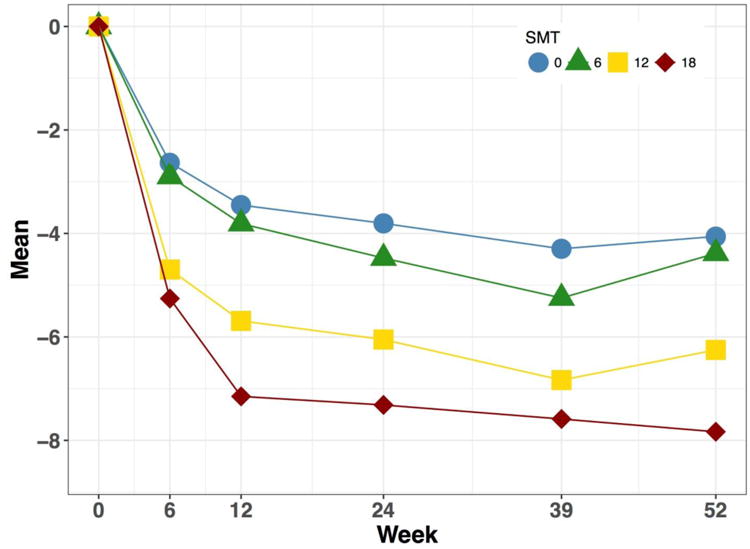
Time profiles. The plots show the development over time of improvement from baseline in days with cervicogenic headache days in the prior 4 weeks for each of the 4 study groups. SMT, spinal manipulative therapy.
A linear dose-response was observed for all follow-up time points and collectively over time in the longitudinal profile (Table 2 and Fig. 3), a reduction of approximately 1 CGH day (in the prior 4 weeks) for each additional 6 visits for spinal manipulation (p<.05). The slopes were specifically -1.1 (p=.002) and -1.0 (p=.010) CGH days / 6 SMT visits at the 12-week and 24-week primary endpoints, respectively.
Fig. 3.
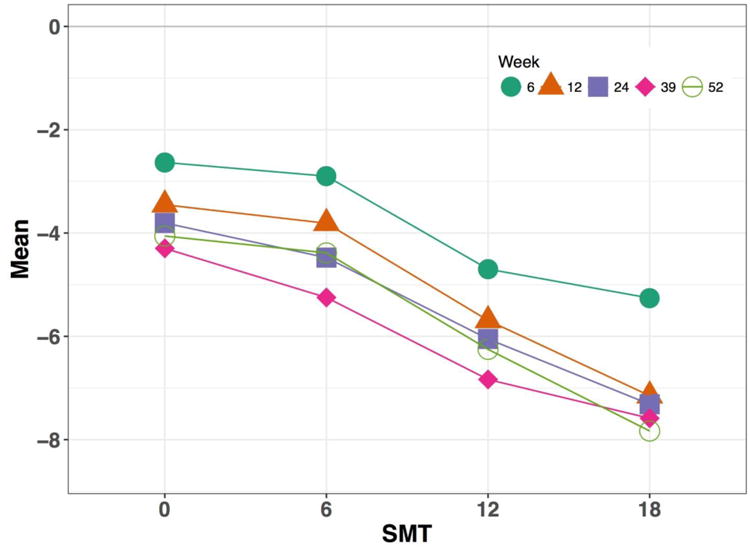
Dose-response curves. The dose-response plots show gradients for improvement in days with cervicogenic headache over the prior 4 weeks for each follow-up time point. SMT, spinal manipulative therapy.
Table 2 also shows that 6 SMT visits had similar outcomes to the no-SMT control and 12 SMT visits demonstrated some advantage over the control, albeit comparisons were not statistically significant. The greatest benefit of SMT compared to the minimal-massage control was found for 18 SMT visits at all time points (p<.05). The adjusted mean differences comparing 18 SMT visits to the control were -3.3 CGH days (p=.004) and -2.9 CGH days (p=.017) in the prior 4 weeks for the 12-week and 24-week primary endpoints, and -2.8 CGH days (p=.005) over all follow-ups in the longitudinal profile.
Sensitivity analysis
There were no important changes in slopes and group comparisons in CGH days when imputed data were excluded in a complete-case analysis. Slope estimates were within ±0.1 days of the primary analysis. Changes in the adjusted mean differences between manipulation groups and the control group at all time points were within ±0.2 CGH days with the exception of one comparison.
Multiple imputation yielded slopes that were the same or slightly smaller than slopes from the primary analysis. The greatest deviation was found for the 24-week follow-up, where the slope was -0.8 for the multiple imputation analysis compared to -1.0 for the primary analysis. Multiple imputation also tended to yield slightly smaller adjusted mean differences between manipulation groups and the control group. The largest deviations from the primary analysis were ±0.5 CGH days in the prior 4 weeks.
Other sensitivity analyses revealed the following. There were no clinically important or statistically significant site × group interactions, so that results can be considered comparable for the 2 data-collection sites. There were no notable nonlinear effects and inclusion of site as a random effect yielded no material differences from the primary analysis.
Responder analysis
Table 3 shows that over half of participants in each group attained 30% reduction in CGH days by 24 weeks; earlier attainment occurred for the higher dose groups only. Generally, less than half of participants in each group reported at least 50% reduction in CGH days with the exception of the highest dose group. The dose-response slopes indicate that an additional 5% to 11% of participants became responders per additional 6 SMT visits. Substantial risk differences favoring SMT over the control were mostly found for 18 SMT visits. For the primary endpoints, the risk difference in responders for this group was 0.35 (p<.001) at 12 weeks and 0.27 (p=.001) at 24 weeks for a minimal clinically important 30% improvement; these correspond to a clinically meaningful number needed to treat of 3 and 4. The risk difference for the 50% improvement threshold was 0.26 (p=.004) at 12 weeks and 0.15 (p=.088) at 24 weeks, corresponding to a number needed to treat of 4 and 7.
Table 3. Responders.
| Observed unadjusted number (%) of responders | Slope (95%CI) | Adjusted risk difference in responders (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Time | Oregon | Minnesota | SMT 0 | SMT 6 | SMT 12 | SMT 18 | per 6 SMT sessions | SMT 0 vs SMT 6 | SMT 0 vs SMT 12 | SMT 0 vs SMT 18 |
| Cervicogenic headache days (≥30% improvement) | ||||||||||
| 6 wk | 49 (40.8%) | 66 (51.6%) | 25 (41.7%) | 25 (39.7%) | 30 (48.4%) | 35 (55.6%) | 0.06 (0.01, 0.12)* | -0.02 (-0.18, 0.15) | 0.10 (-0.07, 0.27) | 0.17 (-0.00, 0.35) |
| 12 wk | 57 (50.0%) | 71 (55.9%) | 23 (39.7%) | 29 (46.0%) | 31 (52.5%) | 45 (73.8%) | 0.11 (0.06, 0.17)* | 0.08 (-0.09, 0.25) | 0.17 (0.01, 0.33)* | 0.35 (0.18, 0.52)* |
| 24 wk | 59 (56.2%) | 79 (62.7%) | 28 (52.8%) | 34 (57.6%) | 32 (54.2%) | 44 (73.3%) | 0.08 (0.03, 0.13)* | 0.09 (-0.08, 0.26) | 0.06 (-0.10, 0.23) | 0.27 (0.11, 0.43)* |
| 39 wk | 68 (65.4%) | 78 (62.4%) | 30 (56.6%) | 38 (64.4%) | 38 (65.5%) | 40 (67.8%) | 0.05 (-0.00, 0.11) | 0.11 (-0.07, 0.28) | 0.11 (-0.07, 0.28) | 0.17 (-0.00, 0.34) |
| 52 wk | 64 (62.1%) | 77 (61.6%) | 31 (59.6%) | 31 (53.4%) | 36 (62.1%) | 43 (71.7%) | 0.07 (0.01, 0.12)* | -0.01 (-0.18, 0.17) | 0.07 (-0.10, 0.24) | 0.20 (0.04, 0.37)* |
| Cervicogenic headache days (≥50% improvement) | ||||||||||
| 6 wk | 31 (25.8%) | 38 (29.7%) | 14 (23.3%) | 13 (20.6%) | 19 (30.6%) | 23 (36.5%) | 0.05 (0.00, 0.10)* | -0.02 (-0.16, 0.13) | 0.09 (-0.06, 0.25) | 0.14 (-0.01, 0.31) |
| 12 wk | 41 (36.0%) | 53 (41.7%) | 17 (29.3%) | 17 (27.0%) | 26 (44.1%) | 34 (55.7%) | 0.10 (0.04, 0.15)* | -0.02 (-0.18, 0.13) | 0.17 (0.02, 0.33)* | 0.26 (0.09, 0.43)* |
| 24 wk | 42 (40.0%) | 57 (45.2%) | 19 (35.8%) | 21 (35.6%) | 27 (45.8%) | 32 (53.3%) | 0.06 (0.00, 0.11)* | -0.01 (-0.18, 0.14) | 0.11 (-0.05, 0.27) | 0.15 (-0.02, 0.32) |
| 39 wk | 55 (52.9%) | 61 (48.8%) | 21 (39.6%) | 32 (54.2%) | 30 (51.7%) | 33 (55.9%) | 0.05 (-0.00, 0.11) | 0.14 (-0.04, 0.31) | 0.13 (-0.04, 0.31) | 0.18 (-0.01, 0.35) |
| 52 wk | 52 (50.5%) | 51 (40.8%) | 21 (40.4%) | 24 (41.4%) | 28 (48.3%) | 30 (50.0%) | 0.05 (-0.01, 0.10) | 0.03 (-0.14, 0.20) | 0.11 (-0.06, 0.28) | 0.13 (-0.04, 0.31) |
CI, confidence interval; UWS, University of Western States; NWHSU, Northwestern Health Sciences University; SMT, spinal manipulation. Unadjusted group counts and percentages are from original data without imputation; slopes and risk differences in responders across groups are computed from imputed data and adjusted for baseline covariates. Positive signs of slopes and risk differences favor higher doses of manipulation.
p<.05.
Secondary outcomes
The mean CGH pain averaged over the days with CGH showed no notable change over time within groups and there were no clinically important differences between groups (Table 4). On the other hand, all 3 SMT groups showed greater improvement than the control group in CGH-related disability. Notably, the 2 higher SMT dose groups had a clinically important and statistically significant advantage over the control in perceived pain change (recall), and the magnitude of perceived change was considerably greater than the change computed from the average pain intensity. Perceived global improvement followed the same pattern as perceived pain change. All SMT groups were superior to the control for confidence care is working, satisfaction with care, and the disposition to seek the same therapy in the future.
Table 4. Secondary outcomes.
|
|
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Observed unadjusted mean (SD) | Slope (95% CI) | Adjusted Mean difference (95% CI) | ||||||||
|
| ||||||||||
| Oregon | Minnesota | SMT 0 | SMT 6 | SMT 12 | SMT 18 | Per 6 SMT sessions | SMT 0 vs SMT 6 | SMT 0 vs SMT 12 | SMT 0 vs SMT 18 | |
| CGH pain intensity averaged over days with CGH in last 4 wk (0–10 scale)† | Anchors: “No pain” (0); “ As bad as pain could be” (10). | |||||||||
| 0 wk | 4.5 (1.1) | 4.5 (1.1) | 4.4 (1.0) | 4.4 (1.0) | 4.5 (1.1) | 4.7 (1.1) | ||||
| 6 wk | 3.9 (1.3) | 3.9 (1.2) | 4.1 (1.2) | 3.9 (1.2) | 3.8 (1.4) | 3.8 (1.2) | -0.1 (-0.2, -0.0)* | -0.3 (-0.7, 0.0) | -0.2 (-0.6, 0.1) | -0.5 (-0.8, -0.1)* |
| 12 wk | 4.0 (1.5) | 4.0 (1.3) | 4.2 (1.4) | 4.0 (1.4) | 3.8 (1.4) | 4.1 (1.5) | -0.1 (-0.2, 0.0) | -0.3 (-0.7, 0.1) | -0.4 (-0.8, 0.1) | -0.3 (-0.8, 0.1) |
| 24 wk | 4.1 (1.5) | 3.9 (1.2) | 4.3 (1.5) | 3.8 (1.2) | 3.8 (1.3) | 4.1 (1.5) | -0.1 (-0.2, 0.1) | -0.5 (-0.9, -0.1) | -0.3 (-0.7, 0.1) | -0.3 (-0.7, 0.1) |
| 39 wk | 4.1 (1.6) | 4.0 (1.3) | 4.1 (1.4) | 4.1 (1.4) | 4.0 (1.5) | 4.1 (1.4) | -0.1 (-0.2, 0.1) | -0.2 (-0.6, 0.2) | -0.1 (-0.5, 0.4) | -0.3 (-0.8, 0.1) |
| 52 wk | 4.0 (1.6) | 4.0 (1.3) | 4.1 (1.3) | 4.1 (1.3) | 3.8 (1.5) | 4.0 (1.5) | -0.1 (-0.3, 0.0) | -0.2 (-0.6, 0.2) | -0.3 (-0.7, 0.2) | -0.4 (-0.9, 0.0) |
| 6 to 52 wk | -0.1 (-0.2, -0.0)* | -0.3 (-0.6, 0.0) | -0.2 (-0.6, 0.1) | -0.4 (-0.7, -0.0)* | ||||||
| CGH-related disability (36–78 scale)† | ||||||||||
| 0 wk | 58.7 (4.6) | 56.1 (4.9) | 58.5 (4.6) | 56.0 (5.2) | 57.2 (5.1) | 57.9 (4.4) | ||||
| 6 wk | 52.4 (6.5) | 51.2 (6.2) | 54.1 (5.9) | 52.1 (5.8) | 49.7 (7.0) | 51.3 (6.1) | -1.3 (-2.0, -0.6)* | -2.4 (-4.6, -0.3)* | -4.5 (-6.7, -2.3)* | -3.6 (-5.8, -1.4)* |
| 12 wk | 52.7 (6.7) | 50.1 (6.6) | 54.0 (6.5) | 51.5 (6.2) | 49.4 (6.8) | 50.3 (6.9) | -1.4 (-2.1, -0.7)* | -2.1 (-4.3, 0.1) | -4.4 (-6.6, -2.2)* | -3.8 (-6.0, -1.5)* |
| 24 wk | 52.2 (7.6) | 50.4 (6.7) | 52.6 (5.9) | 50.4 (7.1) | 51.4 (7.6) | 50.4 (7.8) | -0.9 (-1.7, -0.1)* | -2.4 (-4.8, -0.1)* | -2.2 (-4.6, 0.2) | -3.1 (-5.5, -0.7)* |
| 39 wk | 52.5 (7.8) | 50.8 (7.3) | 53.8 (6.4) | 51.1 (7.1) | 51.0 (8.3) | 50.6 (8.1) | -1.0 (-1.9, -0.2)* | -2.3 (-4.8, 0.2) | -2.8 (-5.4, -0.3)* | -3.3 (-5.9, -0.7)* |
| 52 wk | 52.5 (7.6) | 50.3 (7.2) | 53.4 (6.7) | 51.1 (6.6) | 50.6 (7.9) | 50.3 (8.1) | -1.1 (-1.9, -0.3)* | -2.0 (-4.4, 0.5) | -3.0 (-5.4, -0.5)* | -3.4 (-5.9, -0.9)* |
| 6 to 52 wk | -1.1 (-1.8, -0.5)* | -2.3 (-4.1, -0.4)* | -3.4 (-5.3, -1.4)* | -3.4 (-5.3, -1.5)* | ||||||
| Perceived CGH pain change since baseline (-10–10 scale)† | Anchors: “Pain has decreased” (-10 to -1); “No change” (0); “Pain has increased” (1 to 10). | |||||||||
| 6 wk | -3.6 (3.0) | -2.7 (2.9) | -2.1 (2.9) | -2.6 (2.6) | -3.6 (2.7) | -4.1 (3.2) | -0.7 (-1.0, -0.3)* | -0.5 (-1.5, 0.5) | -1.6 (-2.6, -0.5)* | -1.8 (-2.9, -0.8)* |
| 12 wk | -3.2 (2.9) | -2.6 (2.9) | -1.4 (2.5) | -2.8 (2.7) | -3.5 (3.1) | -3.6 (2.9) | -0.6 (-0.9, -0.3)* | -1.1 (-2.1, -0.1)* | -2.1 (-3.1, -1.1)* | -1.8 (-2.8, -0.7)* |
| 24 wk | -2.5 (3.0) | -2.8 (3.2) | -1.8 (2.8) | -1.8 (2.6) | -3.2 (3.3) | -3.8 (3.5) | -0.6 (-0.9, -0.2)* | 0.3 (-0.8, 1.3) | -1.3 (-2.3, -0.2)* | -1.4 (-2.5, -0.3)* |
| 39 wk | -2.7 (3.5) | -2.5 (3.4) | -1.5 (3.0) | -2.5 (3.5) | -3.2 (3.3) | -3.2 (3.6) | -0.4 (-0.8, -0.0)* | -0.3 (-1.5, 0.9) | -1.4 (-2.6, -0.2)* | -1.0 (-2.2, 0.3) |
| 52 wk | -2.9 (3.5) | -3.1 (3.6) | -2.1 (3.3) | -2.2 (3.3) | -3.6 (3.8) | -4.0 (3.5) | -0.6 (-1.0, -0.2)* | 0.4 (-0.9, 1.6) | -1.4 (-2.6, -0.1)* | -1.4 (-2.7, -0.2)* |
| 6 to 52 wk | -0.6 (-0.8, -0.3)* | -0.2 (-1.1, 0.6) | -1.5 (-2.4, -0.7)* | -1.5 (-2.4, -0.6)* | ||||||
| Anchors: “No symptoms” (1); “Much better” (2); “Somewhat better” (3); “A little better”(4); No change” (5); | ||||||||||
| Perceived CGH global improvement since baseline (1–9 scale)† | “A little worse” (6); “Somewhat worse” (7);“Much worse” (8); ”As bad as it could be” (9). | |||||||||
| 6 wk | 3.1 (1.3) | 3.5 (1.2) | 4.0 (1.2) | 3.6 (1.2) | 2.9 (1.0) | 2.9 (1.2) | -0.4 (-0.5, -0.3)* | -0.4 (-0.8, 0.0) | -1.1 (-1.6, -0.7)* | -1.1 (-1.5, -0.7)* |
| 12 wk | 3.2 (1.2) | 3.5 (1.3) | 4.1 (1.1) | 3.4 (1.1) | 3.0 (1.2) | 3.0 (1.2) | -0.4 (-0.5, -0.2)* | -0.6 (-1.0, -0.2)* | -1.2 (-1.6, -0.8)* | -1.0 (-1.4, -0.6)* |
| 24 wk | 3.4 (1.2) | 3.5 (1.4) | 3.9 (1.3) | 3.7 (1.2) | 3.2 (1.3) | 3.0 (1.1) | -0.3 (-0.4, -0.2)* | -0.1 (-0.5, 0.3) | -0.7 (-1.2, -0.3)* | -0.8 (-1.3, -0.4)* |
| 39 wk | 3.4 (1.4) | 3.6 (1.3) | 4.1 (1.2) | 3.7 (1.3) | 3.1 (1.3) | 3.2 (1.4) | -0.3 (-0.5, -0.2)* | -0.2 (-0.7, 0.2) | -0.9 (-1.4, -0.4)* | -0.8 (-1.3, -0.3)* |
| 52 wk | 3.5 (1.3) | 3.5 (1.4) | 3.9 (1.3) | 3.8 (1.3) | 3.1 (1.2) | 3.2 (1.3) | -0.3 (-0.4, -0.1)* | 0.0 (-0.5, 0.5) | -0.8 (-1.3, -0.3)* | -0.7 (-1.1, -0.2)* |
| 6 to 52 wk | -0.3 (-0.4, -0.2)* | -0.3 (-0.6, 0.1) | -0.9 (-1.3, -0.6)* | -0.9 (-1.2, -0.5)* | ||||||
| Anchors: “Extremely doubtful” (1); “Doubtful” (2); “A little doubtful” (3); “Unsure” (4); | ||||||||||
| Confidence care is working (1–7 scale)‡ | “A little certain” (5); “Certain” (6); “Extremely certain” (7). | |||||||||
| 6 wk | 5.1 (1.7) | 4.8 (1.8) | 3.8 (2.0) | 4.7 (1.6) | 5.8 (1.0) | 5.4 (1.6) | 0.6 (0.4, 0.8)* | 0.9 (0.3, 1.4)* | 2.0 (1.4, 2.6)* | 1.6 (1.0, 2.2)* |
| 12 wk | 5.0 (1.7) | 4.7 (1.6) | 3.8 (1.8) | 4.7 (1.4) | 5.6 (1.2) | 5.3 (1.7) | 0.5 (0.3, 0.7)* | 0.7 (0.1, 1.2)* | 1.8 (1.2, 2.3)* | 1.3 (0.8, 1.9)* |
| 24 wk | 4.7 (1.6) | 4.7 (1.7) | 4.0 (1.8) | 4.4 (1.6) | 5.3 (1.4) | 5.2 (1.5) | 0.4 (0.2, 0.6)* | 0.2 (-0.4, 0.7) | 1.3 (0.7, 1.9)* | 1.0 (0.4, 1.5)* |
| 39 wk | 4.8 (1.6) | 4.6 (1.7) | 3.8 (2.0) | 4.6 (1.4) | 5.2 (1.4) | 5.1 (1.6) | 0.4 (0.2, 0.6)* | 0.6 (0.1, 1.2)* | 1.3 (0.8, 1.9)* | 1.1 (0.5, 1.6)* |
| 52 wk | 4.6 (1.7) | 4.6 (1.7) | 3.6 (1.9) | 4.3 (1.6) | 5.2 (1.4) | 5.1 (1.6) | 0.5 (0.3, 0.7)* | 0.6 (-0.0, 1.1) | 1.6 (1.0, 2.1)* | 1.3 (0.7, 1.9)* |
| 6 to 52 wk | 0.5 (0.3, 0.6)* | 0.6 (0.1, 1.1)* | 1.6 (1.1, 2.1)* | 1.3 (0.7, 1.8)* | ||||||
| Anchors: “Extremely dissatisfied” (1); “Dissatisfied” (2); “Somewhat dissatisfied” (3); | ||||||||||
| Satisfaction with care (1–6 scale)‡ | “Some what satisfied”(4); “Satisfied” (5); “Extremely satisfied” (6). | |||||||||
| 6 wk | 4.9 (1.2) | 5.0 (1.1) | 4.3 (1.4) | 4.7 (1.2) | 5.4 (0.7) | 5.3 (1.0) | 0.3 (0.2, 0.5)* | 0.4 (0.0, 0.8)* | 1.1 (0.7, 1.5)* | 0.9 (0.6, 1.3)* |
| 12 wk | 4.8 (1.3) | 4.9 (1.1) | 4.2 (1.4) | 4.8 (1.2) | 5.4 (0.7) | 5.2 (1.0) | 0.3 (0.2, 0.5)* | 0.5 (0.1, 0.9)* | 1.1 (0.7, 1.5)* | 0.9 (0.5, 1.3)* |
| 24 wk | 4.7 (1.3) | 4.9 (1.1) | 4.2 (1.4) | 4.7 (1.2) | 5.3 (0.8) | 5.2 (0.9) | 0.4 (0.2, 0.5)* | 0.5 (0.1, 0.9)* | 1.1 (0.7, 1.6)* | 1.0 (0.5, 1.4)* |
| 39 wk | 4.7 (1.3) | 4.8 (1.2) | 4.1 (1.5) | 4.5 (1.2) | 5.2 (0.8) | 5.0 (1.1) | 0.3 (0.2, 0.4)* | 0.3 (-0.1, 0.8) | 1.1 (0.6, 1.5)* | 0.7 (0.3, 1.2)* |
| 52 wk | 4.7 (1.3) | 4.8 (1.2) | 4.1 (1.5) | 4.6 (1.1) | 5.2 (0.8) | 5.1 (1.1) | 0.3 (0.2, 0.5)* | 0.4 (0.0, 0.8)* | 1.1 (0.7, 1.5)* | 0.9 (0.5, 1.3)* |
| 6 to 52 wk | 0.3 (0.2, 0.5)* | 0.4 (0.0, 0.8)* | 1.1 (0.8, 1.5)* | 0.9 (0.5, 1.3)* | ||||||
| Would seek same therapy in the future (1-5 scale)‡ | Anchors: “Strongly disagree” (1); “Strongly agree” (5). | |||||||||
| 6 wk | 3.7 (1.4) | 3.5 (1.3) | 2.6 (1.6) | 3.5 (1.2) | 4.2 (1.0) | 4.1 (1.1) | 0.5 (0.3, 0.6)* | 0.9 (0.5, 1.4)* | 1.6 (1.1, 2.0)* | 1.4 (1.0, 1.9)* |
| 12 wk | 3.7 (1.5) | 3.6 (1.3) | 2.6 (1.5) | 3.7 (1.3) | 4.3 (1.0) | 4.1 (1.2) | 0.5 (0.3, 0.6)* | 1.0 (0.5, 1.4)* | 1.7 (1.3, 2.2)* | 1.3 (0.9, 1.8)* |
| 24 wk | 3.7 (1.4) | 3.5 (1.4) | 2.7 (1.4) | 3.4 (1.4) | 4.2 (1.0) | 4.1 (1.2) | 0.5 (0.3, 0.6)* | 0.6 (0.2, 1.1)* | 1.5 (1.1, 2.0)* | 1.3 (0.9, 1.8)* |
| 39 wk | 3.7 (1.4) | 3.5 (1.4) | 2.6 (1.5) | 3.6 (1.4) | 4.2 (1.0) | 4.1 (1.2) | 0.5 (0.3, 0.6)* | 0.9 (0.4, 1.3)* | 1.6 (1.1, 2.0)* | 1.3 (0.9, 1.8)* |
| 52 wk | 3.7 (1.5) | 3.5 (1.4) | 2.5 (1.6) | 3.5 (1.3) | 4.2 (1.1) | 4.0 (1.2) | 0.5 (0.4, 0.7)* | 0.9 (0.5, 1.4)* | 1.7 (1.3, 2.2)* | 1.5 (1.0, 1.9)* |
| 6 to 52 wk | 0.5 (0.3, 0.6)* | 0.9 (0.4, 1.3)* | 1.6 (1.2, 2.0)* | 1.4 (0.9, 1.8)* | ||||||
| Days with non-CGH headaches (last 4 wk)† | ||||||||||
| 0 wk | 2.3 (2.7) | 2.3 (3.0) | 2.3 (3.1) | 2.4 (3.0) | 2.3 (2.4) | 2.2 (3.1) | ||||
| 6 wk | 2.2 (3.0 | 1.9 (2.8) | 2.4 (2.9) | 2.3 (3.1) | 1.7 (2.5) | 2.0 (3.7) | -0.1 (-0.5, 0.2) | -0.2 (-1.2, 0.9) | -0.5 (-1.6, 0.6) | -0.4 (-1.4, 0.6) |
| 12 wk | 2.1 (3.6) | 1.8 (2.8) | 1.8 (3.0) | 2.3 (2.9) | 1.6 (2.1) | 2.1 (4.5) | 0.1 (-0.2, 0.5) | 0.5 (-0.6, 1.6) | 0.1 (-1.0, 1.2) | 0.6 (-0.5, 1.7) |
| 24 wk | 2.3 (3.6) | 1.9 (3.4) | 1.6 (2.7) | 2.4 (3.0) | 2.3 (3.3) | 1.8 (4.5) | -0.0 (-0.4, 0.4) | 0.5 (-0.7, 1.7) | 0.7 (-0.5, 1.9) | -0.1 (-1.3, 1.1) |
| 39 wk | 1.9 (2.8) | 1.9 (3.5) | 1.6 (1.9) | 2.3 (4.0) | 1.7 (2.4) | 1.9 (3.7) | -0.0 (-0.4, 0.4) | 0.4 (-0.7, 1.6) | 0.2 (-0.9, 1.3) | 0.1 (-1.1, 1.2) |
| 52 wk | 2.1 (3.5) | 1.7 (3.5) | 1.4 (1.8) | 2.0 (3.3) | 1.5 (2.7) | 2.5 (5.1) | 0.2 (-0.2, 0.6) | 0.3 (-0.9, 1.5) | 0.2 (-1.0, 1.4) | 0.8 (-0.4, 2.0) |
| 6 to 52 wk | 0.0 (-0.3, 0.4) | 0.3 (-0.5, 1.1) | 0.1 (-0.7, 1.0) | 0.2 (-0.9, 1.3) | ||||||
| Days with neck pain (last 4 wk)† | ||||||||||
| 0 wk | 18.8 (7.2) | 17.9 (7.8) | 19.2 (7.6) | 18.8 (7.2) | 18.2 (8.0) | 17.1 (7.3) | ||||
| 6 wk | 14.1 (9.0) | 14.0 (8.7) | 16.8 (9.0) | 14.7 (8.4) | 12.3 (8.4) | 12.3 (9.0) | -1.7 (-2.5, -0.9)* | -2.0 (-4.5, 0.6) | -4.8 (-7.4, -2.2)* | -4.7 (-7.3, -2.1)* |
| 12 wk | 13.2 (9.0) | 11.7 (9.1) | 15.2 (9.6) | 13.5 (8.6) | 12.2 (8.8) | 8.7 (8.1) | -2.0 (-2.9, -1.2)* | -1.4 (-4.1, 1.3) | -3.4 (-6.1, -0.7)* | -6.2 (-8.9, -3.4)* |
| 24 wk | 13.3 (9.6) | 12.2 (9.4) | 13.4 (9.4) | 14.4 (9.6) | 12.6 (9.8) | 10.4 (9.0) | -1.4 (-2.3, -0.4)* | 0.7 (-2.2, 3.6) | -2.1 (-5.0, 0.8) | -3.7 (-6.6, -0.7)* |
| 39 wk | 12.1 (9.3) | 11.1 (9.3) | 12.9 (10.1) | 12.4 (9.5) | 11.1 (8.8) | 10.0 (8.8) | -1.0 (-2.0, -0.1)* | -0.3 (-3.2, 2.6) | -2.0 (-4.9, 1.0) | -2.9 (-5.8, 0.1) |
| 52 wk | 12.0 (9.9) | 11.3 (9.3) | 13.1 (9.6) | 12.3 (9.9) | 11.2 (9.7) | 10.1 (9.2) | -1.1 (-2.0, -0.1)* | -0.4 (-3.3, 2.6) | -2.2 (-5.2, 0.8) | -2.9 (-5.9, 0.0) |
| 6 to 52 wk | -1.4 (-2.2, -0.7)* | -0.7 (-2.9, 1.6) | -2.9 (-5.2, -0.6)* | -4.1 (-6.4, -1.8)* | ||||||
| Average neck pain intensity in last 4 wk (0–10 scale)† | Anchors: “No pain” (0); “As bad as pain could be” (10). | |||||||||
| 0 wk | 4.6 (1.5) | 4.6 (1.5) | 4.5 (1.5) | 4.5 (1.4) | 4.5 (1.5) | 4.8 (1.5) | ||||
| 6 wk | 3.5 (1.6) | 3.9 (1.8) | 4.1 (1.7) | 3.9 (1.4) | 3.2 (1.8) | 3.7 (1.8) | -0.2 (-0.4, -0.1)* | -0.3 (-0.9, 0.2) | -0.8 (-1.3, -0.2)* | -0.7 (-1.2, -0.1)* |
| 12 wk | 3.7 (1.7) | 3.6 (1.8) | 4.0 (1.8) | 3.7 (1.4) | 3.4 (1.8) | 3.5 (1.9) | -0.2 (-0.4, -0.1)* | -0.3 (-0.9, 0.2) | -0.6 (-1.2, -0.1)* | -0.7 (-1.2, -0.1)* |
| 24 wk | 3.7 (1.9) | 3.8 (1.8) | 3.9 (1.7) | 3.9 (1.9) | 3.6 (1.9) | 3.7 (2.0) | -0.2 (-0.3, 0.0) | -0.1 (-0.7, 0.5) | -0.5 (-1.1, 0.1) | -0.4 (-1.0, 0.2) |
| 39 wk | 3.8 (1.9) | 3.7 (1.9) | 3.9 (1.8) | 4.0 (1.9) | 3.5 (2.0) | 3.6 (1.9) | -0.2 (-0.4, 0.0) | 0.1 (-0.5, 0.6) | -0.4 (-1.0, 0.1) | -0.4 (-1.0, 0.2) |
| 52 wk | 3.6 (2.1) | 3.5 (1.8) | 3.8 (1.9) | 3.5 (1.8) | 3.2 (2.0) | 3.7 (2.1) | -0.1 (-0.3, 0.1) | -0.3 (-0.9, 0.3) | -0.7 (-1.3, -0.1)* | -0.3 (-0.9, 0.3) |
| 6 to 52 wk | -0.2 (-0.3, -0.1)* | -0.2 (-0.6, 0.2) | -0.6 (-1.0, -0.2)* | -0.5 (-0.9, -0.1)* | ||||||
| EuroQol “Health State Today” (0–100 visual analog scale)‡ | Anchors: “worst imaginable health state” (0); “best imaginable health state” (100). | |||||||||
| 0 wk | 74.4 (13.7) | 76.7 (13.2) | 74.9 (13.7) | 76.3 (11.3) | 76.1 (13.9) | 74.8 (15.0) | ||||
| 12 wk | 77.1 (11.4) | 80.6 (12.1) | 78.2 (11.2) | 77.8 (14.0) | 81.5 (9.4) | 78.4 (12.1) | 1 (-1, 2) | -2 (-6, 2) | 2 (-3, 6) | 1 (-4, 5) |
| 24 wk | 77.7 (12.4) | 80.8 (11.7) | 78.5 (12.3) | 81.3 (10.5) | 80.2 (11.0) | 77.6 (14.3) | 0 (-1, 2) | 2 (-2, 7) | 2 (-3, 6) | 0 (-4, 5) |
| 39 wk | 77.0 (12.9) | 81.3 (11.3) | 76.7 (13.3) | 79.9 (10.1) | 81.0 (12.2) | 79.8 (12.9) | 1 (-0, 3) | 2 (-2, 7) | 3 (-2, 7) | 3 (-1, 8) |
| 52 wk | 77.1 (13.7) | 81.2 (12.8) | 76.1 (15.6) | 79.5 (12.3) | 81.2 (13.1) | 80.2 (12.2) | 1 (-0, 3) | 2 (-3, 7) | 4 (-1, 9) | 4 (-1, 9) |
| 6 to 52 wk | 1 (-0, 2) | 1 (-3, 5) | 2 (-2, 6) | 2 (-2, 6) | ||||||
| Days taking medication for CGH (last 4 wk)† | ||||||||||
| 0 wk | 6.3 (4.9) | 6.3 (4.6) | 5.6 (4.5) | 5.9 (4.0) | 6.6 (5.4) | 7.0 (4.8) | ||||
| 6 wk | 4.6 (4.1) | 4.4 (4.6) | 4.8 (4.9) | 4.5 (4.0) | 4.5 (4.4) | 4.3 (4.2) | -0.3 (-0.7, 0.2) | -0.3 (-1.8, 1.2) | -0.6 (-2.2, 0.9) | -0.7 (-2.3, 0.8) |
| 12 wk | 4.1 (5.0) | 4.0 (4.0) | 4.2 (4.0) | 4.2 (4.6) | 4.1 (5.3) | 3.7 (3.9) | -0.3 (-0.8, 0.2) | -0.1 (-1.6, 1.5) | -0.6 (-2.1, 1.0) | -0.9 (-2.5, 0.7) |
| 24 wk | 4.4 (4.8) | 3.6 (3.6) | 4.1 (3.4) | 3.9 (4.3) | 3.8 (4.6) | 4.0 (4.3) | -0.2 (-0.7, 0.3) | -0.4 (-2.0, 1.1) | -1.0 (-2.5, 0.5) | -0.5 (-2.1, 1.0) |
| 39 wk | 3.6 (4.5) | 3.7 (4.2) | 3.0 (3.2) | 3.8 (3.9) | 3.8 (5.2) | 4.0 (4.8) | 0.0 (-0.5, 0.5) | 0.3 (-1.3, 1.9) | 0.1 (-1.6, 1.7) | 0.1 (-1.5, 1.7) |
| 52 wk | 3.8 (4.6) | 4.1 (4.4) | 3.9 (3.8) | 4.5 (4.7) | 3.9 (5.4) | 3.5 (3.9) | -0.3 (-0.8, 0.2) | 0.2 (-1.4, 1.8) | -0.4 (-2.1, 1.2) | -0.8 (-2.5, 0.8) |
| 6 to 52 wk | -0.2 (-0.6, 0.2) | -0.1 (-1.3, 1.2) | -0.5 (-1.9, 0.9) | -0.6 (-1.8, 0.7) | ||||||
SD, standard deviation; CI, confidence interval; UWS, University of Western States; NWHSU, Northwestern Health Sciences University; SMT, spinal manipulation; CGH, cervicogenic headache; VAS, visual analog scale.
Unadjusted means are from original data without imputation; slopes and mean differences are computed from imputed data and adjusted for baseline covariates. Longitudinal profiles using generalized estimating equations are indicated by lines labeled “6 to 52” weeks.
p<.05.
Lower scores are favorable; negative signs of slopes and risk differences favor higher doses of manipulation.
Higher scores are favorable; positive signs of slopes and risk differences favor higher doses of manipulation.
There were less than 2.5 days in the prior 4 weeks reported for non-cervicogenic headaches in any group for any follow-up, so slopes and dose-group differences were trivial. The patterns of improvement in group comparisons for days with neck pain and neck pain intensity were similar to that for CGH. There were no meaningful differences between groups in the EuroQol health state visual analogue scale and in medication use for CGH.
Adverse events
There were no treatment-related severe or serious adverse events reportable to the institutional review boards during the treatment or follow-up phases of the study. All adverse events were reviewed by the independent data and safety monitoring board for severity and relatedness to study intervention. Ten severe adverse events occurred during the treatment phase, all of which were unrelated or unlikely related to study intervention. These included two cases that could be attributable to the natural history of CGH or other headache: a week-long headache and muscle tension that led to couch rest or loss of social activity. The remaining cases were due to unrelated conditions (e.g., accident or visceral disease). During the follow-up phase, there were 11 unrelated serious events and 53 severe events unrelated or unlikely related to study care. Mild or moderate adverse events related to treatment (e.g. neck soreness/pain/stiffness, transient upper extremity pain/tingling, increased headache intensity, nausea, dizziness) were reported by approximately 40% of participants receiving SMT (similar proportions across doses) and approximately 20% of participants in the light-massage control group. The number of mild to moderate adverse events were approximately three times higher in the SMT groups compared to the control; all were short-term and transitory.
Discussion
This was the second full-scale dose-response study of SMT to be conducted for any condition, the previous one for low back pain [21]. Our study had several notable findings. The primary outcome, CGH days, showed that 18 visits to a chiropractor for SMT produced the best relief in terms of dose-response gradient and advantage over the control. This finding was consistent over time from the end of treatment through the one-year follow-up. The responder analysis supported the advantage for 18 visits, particularly at the 12 and 24-week primary endpoints, where the number needed to treat for at least minimal clinically important improvement [42] was a respectable 3 to 4 patients [44]. Importantly, the results suggest about two-thirds of patients receiving 18 SMT treatments can expect minimal clinical important improvement and over half can expect to achieve at least 50% improvement in CGH days. Also noteworthy is that the results of care were robust and similar across study groups in Oregon and Minnesota, despite the sociodemographic differences between sites.
Consideration must be given to the accumulation of benefit increasing care from 0 SMT to 18 SMT visits. At the higher end, up to half of improvement in CGH days was attributable to the intervention compared to the control. Another consideration was the absence of a significant plateau in the dose-response curves over the range of SMT visits to inform selection of an optimal dose for use in future studies or clinical practice. Practical issues including cost, time, and inconvenience to the patient also make it difficult to recommend study of a greater number of visits. The impact of cost-effectiveness on the selection of optimal dose will be addressed in a separate publication.
Most secondary outcomes evaluating CGH and care for CGH (e.g., disability, perceived pain change, global improvement, confidence in care, satisfaction, and willingness to seek the same treatment) were supportive of the findings for the primary outcomes, showing statistically significant linear dose-response gradients at most time points. Although 18 SMT visits generally showed the best outcomes, there was some evidence of saturation effects starting at 12 SMT visits for some variables. Notable exceptions to the trends in the primary outcome were seen for pain intensity and medication use. It seems that SMT may decrease the frequency of CGH without affecting the intensity of CGH headache in a meaningful way. This stands in juxtaposition to previous trials [15,45] and our pilot study showing an effect on pain for higher dose [17]. A likely explanation was our use of headache diaries to evaluate headache pain intensity on a daily basis rather than questionnaire recall as in previous studies. This is supported by the fact that recall of average CGH pain intensity from the questionnaires in the current study (used as back-up for missing diaries) showed statistically significant dose-response at all follow-ups. Medication use was fairly consistent across groups, unaffected by SMT relative to the control.
Surprisingly, neck pain intensity did not show meaningful improvement compared to the control, in contrast to findings from recent systematic reviews [46,47]. It is possible that participants could not distinguish neck pain from headache pain in the occipital region. Alternatively, there may be some distinguishing characteristics of neck-pain generators in CGH patients that do not respond as well to SMT.
Interpretation of the findings from a dose-response randomized trial on SMT requires perspective on several key issues [21]. This was a fastidious randomized trial designed to isolate the unique effects of SMT. We controlled number of visits, time with the participant, effects of hands-on treatment, patient-provider interaction, and intervention credibility with 18 carefully structured visits. Hence, the potential contributions of the doctor-patient interaction and other contextual effects, identified in a previous dose-response study [29], were eliminated from the estimates of the dose-response gradients and group comparisons. Other therapies used by chiropractors were also excluded from the treatment regimen [23].
It is recognized that the light massage is technically not a true control but a comparison treatment. Hence, the magnitude of SMT efficacy is likely somewhat underestimated. A true sham was not used because blinding was not feasible in a study where half of the participants received both treatment and control interventions. We also were trying to avoid the potential negative effects of disappointment in being randomized to a sham (e.g., nocebo effects or loss to follow-up).
In clinical practice, care may be stopped at the discretion of the clinician based on degree of improvement. Stoppage protocols could not be implemented in our trial because they could have interfered with determination of the effects of the full dosage assigned. It is also unknown if stoppage of care is beneficial or detrimental to patient progress.
It is also unclear what constitutes a clinically important difference between groups for the primary outcome. A 50% improvement is a common demarcation for substantial individual improvement [48,49], in our case about 8 CGH per month. However, a threshold for improvement in the individual patient cannot serve as a benchmark for clinical importance of the incremental improvement of treatment compared to a control or other intervention; other study characteristics need to be taken into consideration. [49]. For this study, improvement was durable, compliance with care was high, and secondary outcomes were generally supportive of the primary findings. Safety was acceptable with no serious treatment-related adverse events. The frequency of mild to moderate transient adverse events associated with SMT (reported by approximately 40% of participants) was similar to what has been reported in the literature [50,51].
The study had several notable strengths. Electronic diaries ensured data collection in real time without distortion of recall. Attention to standardization of protocols may have contributed to the similarity of outcomes across sites. The agreement of sensitivity and primary analyses gives confidence in the findings for the primary outcome, the similarity of outcomes across sites, and the viability of a linear dose-response relationship between CGH days and the number of SMT visits. Limitations, discussed above, included the absence of a dose-response plateau to identify the optimal SMT dose, limited generalizability of findings from a fastidious trial to practice, absence of a true sham or no-treatment control, and no accepted standard for a clinically important dose-response gradient across study groups.
Conclusion
There was a linear dose-response relationship between SMT visits and days with CGH, that was durable to 52 weeks following start of care. For the highest and most effective dose of 18 SMT visits, CGH days were reduced by about half, and about 3 more days per month than for the light-massage control.
Acknowledgments
This study was funded by the National Center for Complementary and Integrative Health (NCCIH), National Institutes of Health (R01 AT006330). The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the official views of NCCIH. We wish to thank the clinicians and study staff who contributed to the design and implementation of this study.
Footnotes
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stovner LJ, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193–210. doi: 10.1111/j.1468-2982.2007.01288.x. [DOI] [PubMed] [Google Scholar]
- 2.Atlas of headache disorders and resources in the world 2011. A collaborative project of World Health Organization and Lifting The Burden. Geneva: WHO; 2011. [Google Scholar]
- 3.Solomon GD, Cady RK, Klapper JA, Ryan RE., Jr Standards of care for treating headache in primary care practice National Headache Foundation. Cleve Clin J Med. 1997;64:373–83. doi: 10.3949/ccjm.64.7.373. [DOI] [PubMed] [Google Scholar]
- 4.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders, 2nd edition. Cephalalgia. 2004;24(1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 5.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 6.Nilsson N. The prevalence of cervicogenic headache in a random population sample of 20-59 year olds. Spine. 1995;20:1884–8. doi: 10.1097/00007632-199509000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Sjaastad O, Fredriksson TA. Cervicogenic headache: criteria, classification and epidemiology. Clin Exp Rheumatol. 2000;18(2 Suppl 19):S3–S6. [PubMed] [Google Scholar]
- 8.Sjaastad O, Bakketeig LS. Prevalence of cervicogenic headache: Vaga study of headache epidemiology. Acta Neurol Scand. 2008;117:173–80. doi: 10.1111/j.1600-0404.2007.00962.x. [DOI] [PubMed] [Google Scholar]
- 9.Haldeman S, Dagenais S. Cervicogenic headaches: a critical review. Spine J. 2001;1:31–46. doi: 10.1016/s1529-9430(01)00024-9. [DOI] [PubMed] [Google Scholar]
- 10.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008:1–23. [PubMed] [Google Scholar]
- 11.Eisenberg DM, Kessler RC, Van Rompay M, et al. Perceptions about complementary therapies relative to conventional therapies among adults who use both: results from a national survey. Ann Intern Med. 2001;135:344–51. doi: 10.7326/0003-4819-135-5-200109040-00011. [DOI] [PubMed] [Google Scholar]
- 12.Wells RE, Bertisch SM, Buettner C, Phillips RS, McCarthy EP. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. 2011;51:1087–97. doi: 10.1111/j.1526-4610.2011.01917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bronfort G, Haas M, Evans R, Leiniger B, Triano J. Effectiveness of manual therapies: The UK evidence report. Chiropr Osteopat. 2010;18:3. doi: 10.1186/1746-1340-18-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bryans R, Descarreaux M, Duranleau M, et al. Evidence-based guidelines for the chiropractic treatment of adults with headache. J Manipulative Physiol Ther. 2011;34:274–89. doi: 10.1016/j.jmpt.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Clar C, Tsertsvadze A, Court R, et al. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropr Man Therap. 2014;22:12. doi: 10.1186/2045-709X-22-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varatharajan S, Ferguson B, Chrobak K, et al. Are non-invasive interventions effective for the management of headaches associated with neck pain? An update of the Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur Spine J. 2016;7:1971–99. doi: 10.1007/s00586-016-4376-9. [DOI] [PubMed] [Google Scholar]
- 17.Haas M, Spegman A, Peterson DH, Aickin M, Vavrek D. Dose-response and efficacy of spinal manipulation for chronic cervicogenic headache: a pilot randomized controlled trial. Spine J. 2010;10:117–28. doi: 10.1016/j.spinee.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haas M, Groupp E, Aickin M, et al. Dose-response for chiropractic care of chronic cervicogenic headache and associated neck pain: a randomized pilot study. J Manipulative Physiol Ther. 2004;27:547–53. doi: 10.1016/j.jmpt.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 19.Kaptchuk TJ. The placebo effect in alternative medicine: can the performance of a healing ritual have clinical significance? Ann Intern Med. 2002;136:817–25. doi: 10.7326/0003-4819-136-11-200206040-00011. [DOI] [PubMed] [Google Scholar]
- 20.Hanson L, Haas M, Bronfort G, et al. Dose-response of spinal manipulation for cervicogenic headache: study protocol for a randomized controlled trial. Chiropr Man Therap. 2016;24:23. doi: 10.1186/s12998-016-0105-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haas M, Vavrek D, Peterson D, Polissar NL, Neradilek MB. Dose-response and efficacy of spinal manipulation for care of chronic low back pain: a randomized controlled trial. Spine J. 2014;14:1106–16. doi: 10.1016/j.spinee.2013.07.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stigsby B, Taves DR. Rank-Minimization for balanced assignment of subjects in clinical trials. Contemp Clin Trials. 2010;31:147–50. doi: 10.1016/j.cct.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Gatterman MI, Panzer DM. Disorders of the cervical spine. In: Gatterman MI, editor. Chiropractic management of spine related disorders. Baltimore: Williams & Wilkins; 1990. pp. 205–55. [Google Scholar]
- 24.Vernon H. Spinal manipulation and headaches: an update. Top Clin Chiropr. 1995;2:34–47. [Google Scholar]
- 25.Souza TA. Differential diagnosis for the chiropractor: protocols and algorithms. Gaithersburg, MD: Aspen Publishers, Inc; 1998. pp. 383–402. [Google Scholar]
- 26.Jull G, Amiri M, Bullock-Saxton J, Darnell R, Lander C. Cervical musculoskeletal impairment in frequent intermittent headache Part 1: Subjects with single headaches. Cephalalgia. 2007;27:793–802. doi: 10.1111/j.1468-2982.2007.01345.x. [DOI] [PubMed] [Google Scholar]
- 27.Peterson DH, Bergmann TF. Chiropractic technique: principles and procedures. 2nd. St. Louis: Mosby; 2002. [Google Scholar]
- 28.Cherkin DC, Deyo RA, Sherman KJ, et al. Characteristics of licensed acupuncturists, chiropractors, massage therapists and naturopathic physicians. J Am Board Fam Pract. 2002;15:463–72. [PubMed] [Google Scholar]
- 29.Haas M, Vavrek D, Neradilek MB, Polissar N. A path analysis of the effects of the doctor-patient encounter and expectancy in an open-label randomized trial of spinal manipulation for the care of low back pain. BMC Complement Altern Med. 2014;14:16. doi: 10.1186/1472-6882-14-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nicholson GG, Clendaniel RA. Manual Techniques. In: Scully RM, Barnes MR, editors. Physical Therapy. Philadelphia: J.B. Lippincott Company; 1989. pp. 926–85. [Google Scholar]
- 31.Bendtsen L, Bigal ME, Cerbo R, et al. Guidelines for controlled trials of drugs in tension-type headache: second edition. Cephalalgia. 2010;30:1–16. doi: 10.1111/j.1468-2982.2009.01948.x. [DOI] [PubMed] [Google Scholar]
- 32.Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117–26. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 33.Kosinski M, Bayliss MS, Bjorner JB, et al. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res. 2003;12:963–74. doi: 10.1023/a:1026119331193. [DOI] [PubMed] [Google Scholar]
- 34.Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. 2005;43:203–20. doi: 10.1097/00005650-200503000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Luo N, Johnson JA, Shaw JW, Feeny D, Coons SJ. Self-reported health status of the general adult U.S population as assessed by the EQ-5D and Health Utilities Index. Med Care. 2005;43:1078–86. doi: 10.1097/01.mlr.0000182493.57090.c1. [DOI] [PubMed] [Google Scholar]
- 36.Fischer D, Stewart AL, Bloch DA, et al. Capturing the patient's view of change as a clinical outcome measure. JAMA. 1999;282:1157–62. doi: 10.1001/jama.282.12.1157. [DOI] [PubMed] [Google Scholar]
- 37.Version 1. Bloomington, MN: Quality Quest; 1989. User's manual: low back pain TyPE specification. [Google Scholar]
- 38.Wang SF, Teng CC, Lin KH. Measurement of cervical range of motion pattern during cyclic neck movement by an ultrasound-based motion system. Manual Ther. 2005;10:68–72. doi: 10.1016/j.math.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 39.Chesterton LS, Sim J, Wright CC, Foster NE. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin J Pain. 2007;23:760–6. doi: 10.1097/AJP.0b013e318154b6ae. [DOI] [PubMed] [Google Scholar]
- 40.Diggle PJ, Heagerty PJ, Liang KY, Zeger SL. Analysis of longitudinal data. 2nd. New York: Oxford University Press; 2013. [Google Scholar]
- 41.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011;45:3. [Google Scholar]
- 42.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine. 2008;33:90–4. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 43.Cheung YB. A modified least-squares regression approach to the estimation of risk difference. Am J Epidemiol. 2007;166:1337–44. doi: 10.1093/aje/kwm223. [DOI] [PubMed] [Google Scholar]
- 44.Froud R, Eldridge S, Lall R, Underwood M. Estimating the number needed to treat from continuous outcomes in randomised controlled trials: methodological challenges and worked example using data from the UK Back Pain Exercise and Manipulation (BEAM) trial. BMC Med Res Methodol. 2009;9:35. doi: 10.1186/1471-2288-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dunning JR, Butts R, Mourad F, et al. Upper cervical and upper thoracic manipulation versus mobilization and exercise in patients with cervicogenic headache: a multi-center randomized clinical trial. BMC Musculoskelet Disord. 2016;17:64. doi: 10.1186/s12891-016-0912-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gross A, Langevin P, Burnie SJ, et al. Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane Database Syst Rev. 2015;9:CD004249. doi: 10.1002/14651858.CD004249.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wong JJ, Shearer HM, Mior S, et al. Are manual therapies, passive physical modalities, or acupuncture effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders? an update of the bone and joint decade task force on neck pain and its associated disorders by the optima collaboration. Spine J. 2016;16:1598–630. doi: 10.1016/j.spinee.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 48.Fritz JM, Hebert J, Koppenhaver S, Parent E. Beyond minimally important change: defining a successful outcome of physical therapy for patients with low back pain. Spine. 2009;34:2803–9. doi: 10.1097/BRS.0b013e3181ae2bd4. [DOI] [PubMed] [Google Scholar]
- 49.Dworkin RH, Turk DC, McDermott MP, et al. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146:238–44. doi: 10.1016/j.pain.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 50.Carnes D, Mars TS, Mullinger B, Froud R, Underwood M. Adverse events and manual therapy: a systematic review. Man Ther. 2010;15:355–63. doi: 10.1016/j.math.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 51.Senstad O, Leboeuf-Yde C, Borchgrevink C. Frequency and characteristics of side effects of spinal manipulative therapy. Spine (Phila Pa 1976) 1997;22:435–40. doi: 10.1097/00007632-199702150-00017. [DOI] [PubMed] [Google Scholar]


