Abstract
Multiple changes are influencing work, workplaces and workers in the US including shifts in the main types of work and the rise of the ‘gig’ economy. Work and workplace changes have coincided with a decline in unions and associated advocacy for improved safety and health conditions. Risk assessment has been the primary method to inform occupational and environmental health policy and management for many types of hazards. Although often focused on one hazard at a time, risk assessment frameworks and methods have advanced toward cumulative risk assessment recognizing that exposure to a single chemical or non-chemical stressor rarely occurs in isolation. We explore how applying cumulative risk approaches may change the roles of workers and employers as they pursue improved health and safety and elucidate some of the challenges and opportunities that might arise. Application of cumulative risk assessment should result in better understanding of complex exposures and health risks with the potential to inform more effective controls and improved safety and health risk management overall. Roles and responsibilities of both employers and workers are anticipated to change with potential for a greater burden of responsibility on workers to address risk factors both inside and outside the workplace that affect health at work. A range of policies, guidance and training have helped develop cumulative risk assessment for the environmental health field and similar approaches are available to foster the practice in occupational safety and health.
Keywords: Cumulative risk, Employer, Occupational safety and health, Risk assessment Worker
1. Introduction
There are many changes influencing work, workplaces and workers in the US. Broad changes in the economy have caused shifts in the main types of work from manufacturing to services (Pew Research Center, 2016; World Economic Forum, 2016). Other industries, such as construction and healthcare, remain important but demographics, tools, processes, materials and the way work is organized is changing and will likely continue to change (World Economic Forum, 2016). These changes include non-standard employment relationships such as increases in use of independent contractors and transient workers (Katz and Kreiger, 2016) and more work happening outside of traditional workplaces. Temporary and contract work can offer flexibility of work hours and the chance to develop a variety of skills, both potentially desirable attributes for some workers. However, such arrangements usually have a negative impact on protections provided on the job including safety training, personal protective equipment, and availability of benefits such as health insurance coverage or paid leave (Boden et al., 2016). Greater rates of injury and illness outcomes have been observed in workers in non-standard work arrangements (Virtanen et al., 2005; Benavides et al., 2006; Smith et al., 2010; Asfaw et al., 2012). Technological advances are also dramatically changing the nature of work, leading to the elimination of some jobs and the creation of others. Some technologies permit the same level of production with fewer workers or allow for the use of less skilled labor, while other technologies require workers to learn new skills if they wish to continue employment (World Economic Forum, 2016). Work and workplace changes have coincided with a decline in unions and associated advocacy for improved safety and health conditions (Boden et al., 2016).
Workforce demographics have also changed over recent decades with increased diversity with regard to age, gender, race and ethnicity (Boden et al., 2016; Lerman and Schmidt, 2017). Other trends in personal health such as wearable technology (e.g., activity monitors and other health-related sensors), genetic profiling and adoption of electronic health records can introduce new types of data and data analysis into prevention, health promotion and health care efforts. These trends present challenges and opportunities for occupational health and safety professionals that may be addressed in part through the incorporation of risk assessment principles and risk management practices, including those developed under the National Institute for Occupational Safety and Health (NIOSH) Total Worker Health Program®.
1.1. Cumulative risk assessment
Risk assessment has been the primary method to inform occupational and environmental health decision making for many types of hazards (chemical, physical, microbial, radiological, ergonomic, etc.) (NRC, 1983, 2009). Risk-based decision making includes three phases: problem formulation and scoping; planning and conduct of risk assessment; and risk management (NRC, 2009). The core risk assessment process includes: hazard identification; dose-response assessment; exposure assessment; and risk characterization (NRC, 1983, 2009). The resulting characterization of exposures and risks is designed to be used to develop interventions or policies to reduce exposure and risk (i.e., risk management). This paper adopts a broad concept of risk assessment encompassing a variety of activities to identify hazards affecting worker health and safety. The complexity and scope of a risk assessment will vary greatly depending on the hazards present, the work process, the industry, and the size of the business; risk management interventions will similarly vary. The risk assessment process (and subsequent management activities) can be used in many contexts, e.g., at a particular workplace or for a certain type of worker across different workplaces. A risk assessment may be focused on particular hazards or stressors (stressor-based) or may address a health problem for a group of workers such as those with hearing loss or respiratory disease (an effects-based assessment) (Menzie et al., 2007).
The risk assessment process was developed (and is still typically applied) to address one hazard at a time. However, the risk assessment field has begun to develop frameworks and methods for understanding cumulative risk, defined by US Environmental Protection Agency (EPA) as “the combined risks from aggregate exposures to multiple agents or stressors” (US EPA, 2003). The cumulative risk definition has two aspects: first, the concept of aggregate exposure meaning that all sources and pathways of exposure are identified for a particular hazard or agent; and second, that real-life exposures are not limited to single hazards and that multiple hazards and types of stressors are present and should be evaluated. Methods and applications of cumulative risk assessment (CRA) are still developing. US EPA and the Agency for Toxic Substances and Disease Registry have incorporated aspects of CRA into a number of different contexts with emphasis on aggregate exposure assessments in some cases and attention to multiple chemicals (mixtures) in others, see Table 1. Moving beyond chemical mixtures to develop assessments of multiple stressors (chemical and non-chemical) remains challenging (Fox et al., 2017; NRC, 2009). Approaches to these more complex assessments include the need for screening steps to simplify analysis, qualitative methods, and semi-quantitative scores or indices to combine disparate types of data (US EPA, 2007; Moretto et al., 2017).
Table 1.
Selected programs applying cumulative risk assessment concepts.
| Concepts | Programs | References |
|---|---|---|
| Aggregate exposure | Pesticide exposures from food, water, and home uses are evaluated by the US EPA Office of Pesticide Programs | US EPA (2002) |
| When a drinking water standard is established the Office of Water also evaluates exposures to the agent of interest from air, food, etc., as well as water to understand the relative source contribution. |
US EPA (2017) | |
| Chemical mixtures | Mixtures of air toxics are evaluated for various non-cancer outcomes, such as respiratory, neurological, endocrine, kidney, etc., and cancer health effects in the National Air Toxics Assessment. |
US EPA (2015) |
| Joint toxicity/interaction | Under its mandate to support Superfund, ATSDR developed methods to evaluate joint toxicity and interaction of chemical mixtures. | ATSDR (2004) |
To date, CRA has been primarily applied to understand exposures in the ambient and social environments to evaluate ecological or general population health (Fox et al., 2017). Efforts are underway to recognize cumulative exposures and advance the practice of CRA for worker health and safety. For example, Schulte et al. (2012) presented several “combinatorial models” of personal risk factors and occupational hazards (multiple hazards or stressors); and Lentz et al. (2015) described how an aggregate exposure concept such as the relative source contribution could result in advances in the development of occupational exposure limits. Dotson et al. (2017) described CRA as part of an innovative risk assessment approach for OSH that will inform risk management activities, such as the Total Worker Health® (TWH) program discussed below (see Table 2).
Table 2.
CRA can inform risk management under the TWH® program.
Sources: Dotson et al. (2017), NIOSH (2015), NRC (1983, 2009) and US EPA (1997, 2003).
|
Cumulative risk assessment
Scoping and problem formulation Hazard identification Dose-response assessment Exposure assessment Risk characterization |
 |
Risk management via Total Worker
Health® "Policies, programs, and practices that integrate protection from work-related safety and health hazards with promotion of injury and illness prevention efforts to advance worker well-being." |
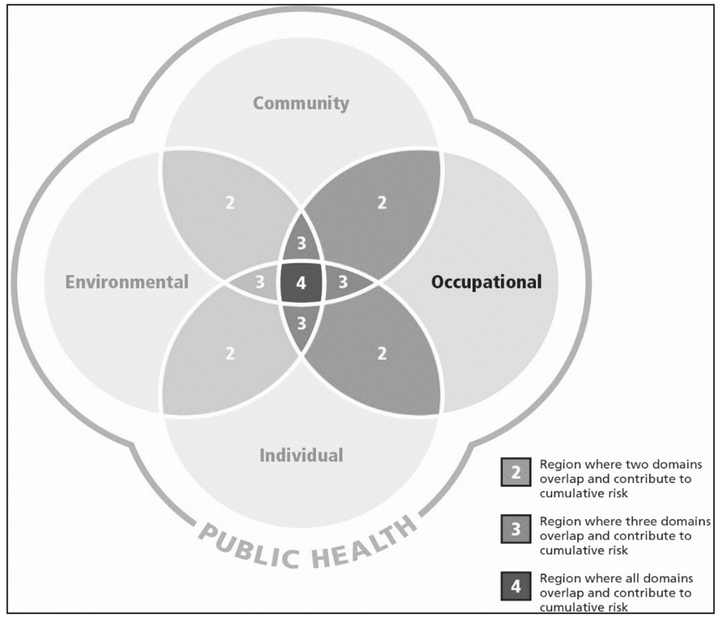
The US EPA definition of cumulative risk parallels the conceptual model of the multiple determinants of health (Fox et al., 2002). Evans and Stoddart (1990) presented a version of this model illustrating that health and well-being are functions of an individual's genetic endowment and behavior as well as their social and physical environments (including workplaces), disease status and access to health care (often employer-based). Assessing risks to health of a population under this model requires attention to these multiple influences. Fig. 1 helps illustrate the concepts embodied by CRA. Even when focused on the health of workers in the occupational domain, as illustrated in the figure, there is the potential for the influence of multiple stressors originating from sources across multiple domains including at the individual level (behavior, genetic), the community level, and the ambient environment.
Fig. 1.
Multiple domains of public health influence occupational health.
A health and safety assessment conducted under this type of comprehensive framework has the potential to inform new risk management approaches, exposure reduction strategies, and prevention activities addressing multiple stressors in multiple domains. Anticipating that such assessments will be conducted in occupational settings, the purpose of this paper is to: 1) explore how CRA approaches may change the roles of workers and employers as they assess and manage health and safety while navigating work and workplace trends; 2) identify barriers and benefits to adoption of the CRA approach among workers; and 3) identify the challenges and opportunities that might arise for employers with adoption of a CRA approach. To begin, current roles of workers and employers in OSH practice are described. We then introduce several cumulative risk case examples designed to describe a range of potential cumulative exposure and health risk issues. Finally, we explore how application of cumulative risk assessment approaches could change existing health and safety roles, practices and concerns of workers and employers.
2. Part I: what are the current roles, motivations, and concerns?
Occupational safety and health statutes identify the roles and responsibilities employers have in protecting workers. In the OSH Act (P.L. 91-596), Congress explained that its purpose is “to provide for the general welfare, to assure so far as possible every working man and woman in the Nation safe and healthful working conditions and to preserve our human resources”. The OSH Act recognizes that both employers and employees have “separate but dependent” roles in improving occupational health and safety. The employer role has two parts: to provide a safe workplace; and to comply with standards promulgated under the OSH Act. The employee role is to comply with rules, regulations, and orders under the OSH Act that relate to his/her actions. Title I of the Americans with Disabilities Act (ADA) (42 USC 42 U.S.C. § 12101 and amendments P.L. 110-325) prevents discrimination in the workplace and constrains an employer's ability to obtain disability information and medical examinations; it also requires employers to implement reasonable accommodations such that a disabled individual can perform essential job functions and generally ‘enjoy equal employment opportunities’. The various responsibilities and practices that have been established to realize the purposes of the OSH Act and ADA are introduced below for employers and for workers. This section also includes discussion of employer and worker concerns related to their respective roles.
2.1. Employer roles and concerns in occupational safety and health management
Broad variability exists in the perspective of the employer when it comes to occupational safety and health, depending on factors such as the size of the company, the type of work being done, and the hazards present in the workplace. Broad variability also exists in the utilization of risk assessment to prevent workplace injuries and diseases. According to OSHA, employers have a responsibility to provide a workplace free from serious recognized hazards and comply with standards, rules and regulations issued under the OSH Act as well as examine workplace conditions to make sure they conform to applicable OSHA standards (OSHA, 2017b). A critical element of any effective safety and health program is a proactive, ongoing process to identify and assess hazards in the workplace that could lead to injury, illness, or incidents (OSHA, 2017a). In other words, risk assessment is necessary for workplace injury and disease prevention. Government agencies utilize risk assessments to inform policy decisions, and from an occupational standpoint, develop exposure limits for chemicals, radiological agents, noise, and other potential hazards. In similar fashion, many employers utilize risk assessments for identifying, prioritizing, and controlling hazards in the workplace. Risk assessment is an important tool for the development of appropriate controls to address occupational risk factors. American National Standards Institute (ANSI, 2012) states, “Risk assessments have been an integral part of the practice of safety for many years. Risk assessment outcomes can be used to understand the relative levels of risk in the workplace and the importance of identifying strategies to reduce risk”. Modern incident causation models reflect the ideas of multiple causes, multi-linear interactions of causes and effects, and multiple opportunities for control (ANSI, 2012). Although, there is wide variability in the application of risk assessments in the workplace as well as their complexity, there are risk assessment tools available to help all enterprises better protect employees (e.g., OSHA, 2017a).
Cumulative risk assessment (CRA) will be a valuable tool for employers in carrying out core safety functions. An early step in the development of an effective occupational safety and health program is the identification and assessment of risks in the workplace (OSHA, 2017a). Risk identification typically involves a mixture of past experiences, historical data, and multiple information sources including incident histories at similar firms. These past incidents are rarely the outcome of a single root cause. Popular root cause analysis techniques consider the overlapping contributions of multiple factors, including human errors, mechanical failures, procedural shortcomings, and management system failures (Rooney and Vanden Heuvel, 2004). Each of these potential causes of unwanted incidents can be influenced by factors from occupational, personal, community, and environmental domains.
The CRA approach can benefit employers in prioritizing risks in the workplace by allowing consideration of multiple risk factors including personal and community risk factors along with occupational, providing a more holistic evaluation of risks impacting the workforce. For example, if the risk assessment only took into consideration the occupational risk factors for the development of heart disease, then these risks may be considered low and not significant enough to warrant interventions. However, if the risk assessment took into account personal, community, environmental, and occupational risk factors for heart disease, then the risk may be much higher in the prioritization phase warranting the implementation of interventions to reduce the risk in the workplace. CRA provides a framework for the assessment of multiple risk factors coming from multiple domains; the results of which will enable employers to develop more effective controls for the workplace.
The OSHA standards present the minimum compliance required of employers to achieve the purpose of the law. However, given that the costs of worker injuries and illnesses affect both productivity as well as healthcare costs (e.g., Finkelstein et al., 2005, 2010; Meraya and Sambamoorthi, 2016), many employers invest time and money to strive for an injury-free and healthy workforce, going beyond what is required for compliance. Not all employers will recognize the benefit of utilizing a CRA approach for occupational safety and health programs, but the employers that work to achieve a strong safety culture and to minimize injuries and illnesses to the extent possible are more likely to see the value in CRA approaches.
It should be noted that occupational disease doesn't always impact the financial success of a business because it may not surface during employment or it may not be recognized as occupational in origin. Furthermore, the traditional mature manufacturing employer is not as prevalent in today's economy as it once was in the U.S. As more and more American workers are obtaining temporary positions and working as independent contractors, the situation can be very different from that previously described. Independent contractors often are not offered health insurance benefits, paid leave time, or have a workplace with an OSH program. These workers are more likely to change work settings often and experience much more variability in work tasks as they go from job to job. Without the services of an OSH program, they are not likely to reap worker benefits from hazard identification and control efforts (Howard, 2017).
2.1.1. Health and well-being policies, programs and practices
Employers are increasingly addressing the health and safety needs of workers on and off the job, with many recognizing that a healthier workforce costs companies less through lower healthcare costs (Berry et al., 2010). Loss of workers to injury or illness, whether work related or not, impacts productivity, employee turnover, re-training costs, and business continuity. Addressing health and safety broadly, i.e. utilizing CRA to consider multiple domains of risks and developing controls to reduce those risks, has the potential to account for non-occupational risks in conjunction with occupational risks, allowing for more effective risk management. Interventions to reduce safety and health risks could include: comprehensive occupational safety and health programs; health benefits such as affordable healthcare coverage, paid sick leave and disability plans; worker-centered policies around flexibility in work schedules and healthier supervisory practices; and the provision of employee assistance programs (EAP).
Traditional worker health and disease prevention programs, including workplace health promotion programs in the workplace, have grown in number and popularity over the past several decades. According to a national survey conducted by Rand Health, approximately half of U.S. employers offer wellness promotion initiatives; however, it should be noted that small businesses with fewer than 50 employees were not included in the survey (Rand, 2013). These programs often include health screenings as well as interventions to reduce health risks such as employee benefits like gym memberships, smoking cessation programs, weight loss programs and incentives for participation (Rand, 2013). Some reviews have shown that, when properly executed with the appropriate goals and worker protections in place, well-being programs can achieve both health benefits for workers and financial benefits for their company (Goetzel et al., 2014, 2016). These types of programs typically require health screenings for employees which may include body mass index, cholesterol, and blood pressure for example. For example, employees considered at risk for cardiovascular disease or stroke may be offered programs to help manage their risk factors. Some may even be required to participate in wellness activities in order to receive lower insurance costs. Critics of these programs cite the failures of these programs to address the underlying risks to health related to the nature of the work itself, risks related to loss of privacy, and penalties for non-participation that make the programs no longer feel voluntary, to include cost-shifting of healthcare costs to vulnerable workers (Lax, 2016).
More recently, the Total Worker Health® program at NIOSH has promoted a more integrated approach to worker safety and health, on and off the job. NIOSH defines Total Worker Health (TWH) as policies, programs, and practices that integrate protection from work-related safety and health hazards with promotion of injury and illness prevention efforts to advance worker well-being. The TWH concept fosters a broad, organizational level focus, integrating multiple efforts to advance the health of workers, from the traditional control of workplace hazards and exposures, to addressing work organization, compensation and benefits, work-life management, organizational culture and leadership, and the community and built environment (NIOSH, 2015).
2.2. Worker role and concerns in occupational safety and health management
2.2.1. Training
Although the employer is responsible for providing workplace training (typically implemented by the OSH professionals), participating in the training and applying the training to work tasks is also part of the worker role in OSH. A systematic review by Robson et al. (2010), found that workplace training was effective in increasing worker knowledge of hazards and in development and practice of health protective behaviors, such as use of personal protective equipment (PPE). The authors have had similar experience with effective use of engineering controls, such as local exhaust ventilation, following training (Weinstein et al., 2016). As discussed further below, applying CRA approaches to assess workplace safety and health issues will likely lead to new management strategies such as trainings that address risk factors across multiple domains (Fig. 1 above). Participatory approaches that engage workers in the development and during the implementation of both CRA and training activities are likely to have a positive impact on the outcome.
2.2.2. Health exams, medical information and privacy concerns
The degree to which workers may be required to provide and/or voluntarily disclose health and medical information to the employer in the interest of maintaining a safe workplace varies and can be a source of controversy. Such inquiries or exams are generally conducted to ensure that the worker is capable to perform work tasks without risk to their own or others' safety sometimes defined as “fitness for work” (Serra et al., 2007). For example, one of the most common Occupational Safety and Health Administration (OSHA) standards for which a medical evaluation is required is the Respiratory Protection Standard (29 CFR 1910.134) which requires workers be evaluated for their ability to wear a respirator. In this standard, the medical criteria are simply whether the worker is fit or unfit to wear a respirator.
The ADA (and other laws specific to certain occupational groups, e.g., workers exposed to hazardous substances) place limits and requirements on employee medical exams and disability-related inquiries. Under the ADA, such inquiries and medical exams are prohibited prior to an offer of employment but may occur after a job offer is made but before work begins as well as after the employment begins (U.S. EEOC, 2000). The context and circumstances for exchange of health-related information can vary and may include transfer of information from a private physician (with permission of worker/patient per the Health Insurance Portability and Accountability Act [HIPAA] of 1996 [P.L. 104-191]), or a visit to an occupational health clinic at the workplace, or through a voluntary workplace employee assistance or health promotion program. There are several types of health- and safety-related tests related to “fitness for work” that are not considered medical examinations per the ADA including: tests for use of illicit drugs; physical agility or fitness tests; and psychological tests (U.S. EEOC, 2000). Medical information obtained through examination, inquiry or disclosed voluntarily is considered a confidential medical record which can be shared only under limited circumstances. Acquisition and use of genetic information that may be related to health risk including an individual's genetic tests and family history is also regulated and may not be used to discriminate for employment purposes (the Genetic Information Nondiscrimination Act [GINA] of 2008, P.L. 110-233; U.S. EEOC, 2017). For successful adoption and implementation of a cumulative risk assessment approach, ensuring worker privacy protections and safeguards to prevent discrimination based upon medical or genetic factors will be paramount.
2.2.3. Worker role in risk assessment at work and beyond the workplace
Strong worker participation is a key to effective risk assessment and management for workplace safety and health. Workers will benefit from hazard mitigation and often know most about the potential hazards of their job tasks and environment (hazard identification). Detailed guidelines for worker participation are available from OSHA (2017a). Participation is not limited to reporting hazards and illness but should extend through all aspects of the program including planning and set-up, operation, evaluation and program improvement.
In contrast to the OSH professional, who receives specialized training (e.g., core functions described above), the worker is primarily focused on their particular job and its tasks. Having the structure of core safety functions may facilitate the adoption of CRA for OSH professionals but in-turn raises the challenge of changing the worker role. Outlined below are examples of how personal, and community factors can influence a worker's health at work. Implementing a CRA approach to health at work potentially expands the scope of the worker role to modifying or controlling aspects of their personal, home and community environments.
Workers' understanding of the connection between work, environmental and personal characteristics and behaviors is essential in optimizing the CRA approach. For example, personal behaviors like regular exercise promotes general fitness and can reduce pain (for example, Gordon and Bloxham, 2016) and may improve work performance or lower injury risk. Smoking and alcohol use are risk factors for many chronic diseases and may interact with occupational risk factors to increase risk for disease development (Schulte et al., 2012); alcohol and drug misuse affect work through lower productivity (Gmel and Rehm, 2003; National Council on Alcoholism and Drug Dependence, 2015). Employers must be mindful of the measures they employ when promoting healthy behaviors outside of the workplace and that they are respecting the privacy of their employees. To promote healthy behaviors, employers may establish workplace programs such as tobacco cessation programs, drug-free workplace policies, voluntary EAPs, and health and well-being programs, as noted above. But in the CRA approach, it will be critical that initiatives promoting exercise, healthy lifestyle and fitness should not be used as a replacement for engineering out occupational hazards or for minimizing such hazards. For example, a morning stretching program will not be adequate in preventing musculoskeletal disorders in working conditions where equipment is poorly designed from an ergonomic point of view or work demands are excessive.
Aspects of a worker's family, community and social environment (at home and at work) can have both beneficial and harmful influences on health. For example, various stressors including financial hardship and interpersonal difficulties with family, friends or co-workers have been shown to increase levels of inflammatory markers associated with cardiovascular disease (Sturgeon et al., 2016). Community activities, such as religious attendance can buffer the effects of financial hardship (Bradshaw and Ellison, 2010). Social groups may model healthy or unhealthy behaviors as well as provide various types of social support, such as providing emotional support, problem solving, financial aid, or help with practical tasks (Thoits, 2011). These influences on health occur through complex social and cultural mechanisms often outside an individual's control. A CRA may identify community and social factors that can positively impact the health for particular worker populations or communities.
2.3. Part I summary
We have reviewed the important legal bases of OSH programs and presented both employer and worker roles and concerns in developing and implementing such programs. The next section presents several practical OSH problems that exemplify various aspects of cumulative risk including combinations of exposures occurring in multiple domains. Analysis and consideration of these examples helps reveal how the application of CRA may change the current roles and concerns of employers and workers engaged in OSH programs. Understanding these changes brings to light a number of implications, both in terms of challenges and opportunities of introducing CRA into OSH programs that are further explored in Part III.
3. Part II: cumulative risk examples
The following examples are drawn from published literature and the authors' own work experiences, representing a variety of occupations and workplaces. Because CRA is not routinely practiced in the OSH field there are no formal “OSH CRAs” to highlight. These examples feature commonplace cumulative work exposures and help to illustrate how CRA concepts can be applied to develop a risk management approach. These examples are by no means exhaustive of circumstances where a CRA approach could be applied.
3.1. Example 1: work tasks and obesity increase risk of carpal tunnel syndrome (CTS)
3.1.1. Importance
Among nonfatal occupational injuries, CTS is the third ranked in median number of days lost from work (25 days) (Bureau of Labor Statistics, 2017).
3.1.2. Populations of interest
Workers in manufacturing, healthcare, agriculture.
3.1.3. Potential stressors/hazards/interactions
Job tasks with high hand activity and forceful exertion; worker obesity.
3.1.4. Exposure patterns
Burt et al. (2011) found that a high frequency of exertion resulted in tripling of the odds for CTS among the obese, while obesity resulted in doubling the odds for CTS among those with at least 15 exertions per minute.
3.1.5. CRA considerations/approach
The combination of a high frequency of exertion using the hands at work and obesity increases the odds for CTS more than either of those risk factors alone. Considering Fig. 1 and drawing on the Burt et al. (2011) study, the exposures of concern originate in three domains, forceful exertion and high hand activity from work, and the individual and social/community aspects of obesity (Pachucki and Goodman, 2015).
3.1.6. Potential interventions
In this situation, a ‘cumulative risk’ management approach to reduce the risk of CTS should address both the forceful exertion risk factor as well as obesity across all relevant domains of exposure. Individual, social and workplace factors can contribute to obesity. Reducing obesity can include workplace changes that mitigate major job stressors, decrease the demands of the work itself, promote worker autonomy and flexibility, and address hours of work and wages. Additionally, well-being initiatives such as support for adequate break and meal-times, access to facilities for physical activity and time to utilize them, and education for employees on healthy meal choices and preparation. Policies targeting work organization, worker autonomy and wellbeing combined with addressing the nature of the work with the appropriate ergonomic controls can reduce the risk for CTS.
3.2. Example 2: shift work, community and environmental exposures increase risk for heart disease
3.2.1. Importance
Heart disease has been the most common cause of death in the United States for many years (CDC, 2016).
3.2.2. Population of interest
Shift workers in many sectors, e.g., healthcare, security, manufacturing.
3.2.3. Potential stressors/hazards/interactions
Multiple stressors contribute to heart disease risk.
3.2.4. Exposure patterns
Shift work contributes to job strain and physiological changes that increase heart disease risk (Puttonen et al., 2010); neighborhood deprivation, psychological stress, and air pollution also increase heart disease risk (Koulova and Frishman, 2014; Steptoe and Kivimaki, 2012; Sundquist et al., 2004); smoking, exercise and abnormal blood lipids are examples of well-recognized individual-level risk factors for heart disease (Yusuf et al., 2004). Workers on afternoon and night shifts have, on average, less education and lower wages than day-shift workers indicating lower socio-economic status and suggesting potential for exposure to community and environmental stressors (Enchautegui, 2013; Saenz, 2008).
3.2.5. CRA considerations/approach
Stressors originating across all domains of Fig. 1 have been associated with heart disease risk. In studies focused on myocardial infarction, population attributable risks (PAR) have been derived for job strain and other stressors, e.g., Yusuf et al. (2004) calculated PARs of 32.5% for psychosocial factors (depression, locus of control, perceived stress and life events) and 13.7% for lack of daily consumption of fruits and vegetables; Kivimaki et al. (2012) calculated a PAR of 3.4% for job strain. There is a large literature on cardiovascular disease morbidity and mortality and ambient air pollution (Du et al., 2016). A multi-faceted cumulative risk management effort addressing occupational and non-occupational domains could be developed to reduce and prevent heart disease.
3.2.6. Potential interventions
A broad range of community, environmental and occupational risk factors have been associated with the development and progression of heart disease and related outcomes. However, heart disease risk management is typically focused on the individual, e.g., the National Heart, Lung and Blood Institute (NHLBI) webpage on coronary heart disease (NHLBI, 2018). In contrast, a risk management approach rooted in a CRA would look across all domains of exposure to identify opportunities and partners in reducing exposure and risk. For example, there are resources available to guide employers in developing shift schedules to reduce and manage related job strain and negative consequences (Burgess, 2007; Rosa and Colligan, 1997). In some settings, corporate social responsibility frameworks have been used to address community problems. Workers may participate in the employer corporate social responsibility program or may be active as individuals in community development in other ways. Similarly, environmental management frameworks such as ISO 14001 can be implemented by employers to understand and reduce environmental impacts of the organization (American Society for Quality, 2017).
3.3. Part II summary
Practical examples introduced the potential of CRA as a framework to comprehensively characterize multiple influences on worker health and safety. As a new and developing approach, its application and subsequent risk management activities suggest expanding roles for both employers and workers.
4. Part III: discussion of the challenges and opportunities of CRA
Application of CRA should result in better understanding of complex exposures, health risks and related modifying factors, with the possibility of attributing risk across multiple domains. Addressing exposures in this comprehensive manner should lead to the development of more effective workplace controls and improved safety and health risk management overall.
Table 3 summarizes important implications of CRA for employers and workers. Both employers and workers would face some increased responsibilities, challenges and also potential benefits. The implementation of CRA also has potential to reduce liability for employers in cases where the majority of risk factors are found to be outside the workplace. CRA may place a greater burden on workers, as responsibilities may shift to controlling risks outside the workplace and more health evaluations may also be necessary as risk factors become better understood. Cautions should be taken to ensure that these additional burdens do not outweigh the potential benefits that might accrue to workers through the CRA approach.
Table 3.
Implications of cumulative risk assessment on employers and workers.
| Implications of CRA | Employer | Worker |
|---|---|---|
| Increased liability or responsibility |
Engagement in controlling risks both inside and outside the workplace even when workplace risk alone is small, e.g., providing education to workers on strategies to manage risks outside the workplace |
Greater importance of managing risks in home, social environment, and community Need to participate in more complex health assessments or fitness for work evaluations and potential threats to privacy Greater burden on workers to demonstrate impact of occupational exposure contribution to disease burden |
| Reduced liability or responsibility |
More accurate assessments may reduce employer liability where a majority of risk factors lie outside the workplace |
|
| Other challenges | Managing desirability of certain jobs or workplaces Addressing risks outside of work without impinging on privacy of workers |
Increased potential for discrimination due to personal, genetic or behavioral risk factors Increased employer intervention into personal life |
| Other benefits | More comprehensive assessment framework/tools | Better understanding of risk to inform personal health decisions; improved health and well-being |
4.1. Moving forward
Several approaches have been used in the development of CRA methods to date. Agencies have supported the development of guidance and expert panel reports as well as research funding opportunities (US EPA 2003, 2009; NRC, 2008). Scientists have offered professional trainings (e.g., Society for Risk Analysis, 2016, 2017). The Food Quality Protection Act of 1996 (P.L. 104-170) mandated that US EPA apply cumulative risk concepts including aggregate exposure and chemical mixtures assessment in evaluations of pesticides with a common mechanism of action. Resources required for each approach will vary but development of CRA for OSH could occur through passage of laws, organizational policies, trainings, guidance or other mechanisms.
Some resources exist that can guide an OSH CRA. With OSH in mind, Schulte et al. (2012), Williams et al. (2012), and Lentz et al. (2015) present introductory examples, lists of potential exposures or stressors and a case study, respectively. Other authors have proposed general approaches for CRA that feature phased or tiered analyses, although these are written with an environmental health rather than OSH focus. Menzie et al. (2007) outline approaches (including specific types of data analyses and tools) addressing two potential motivations for a CRA: (1) concern about a health effect or an effects-based assessment; or (2) concern over multiple stressors or a stressor-based assessment. Moretto et al. (2017) presents a step-wise framework for CRA with a focus on evaluating and incorporating non-chemical stressors.
A CRA will typically include consideration of community and environmental risk factors so OSH practitioners will need community and environmental data that they are not accustomed to accessing. Flexible, scalable tools will be needed to accommodate varied workplaces and resource levels. Training (of OSH professionals) on both methodology and data sources will be required for successful implementation in the workplace, e.g., OSH professionals will need to be able to assess and explain how occupational and non-occupational risk factors contribute to health outcomes of concern and then be able to guide workers on mitigating both types of risk factors. Safety professionals will also benefit from guidance regarding employee privacy laws including requirements under ADA, GINA, and HIPAA, specifically addressing legal requirements surrounding the acquisition of employee health data.
In order for CRA to truly be a useful tool for occupational health and safety professionals in the workplace several needs must be addressed. Practitioners in this field will need to fully understand and be convinced that the benefits offered by this approach outweigh the cost and complexity. While this paper presented examples highlighting the application of CRA in the workplace, more research is needed to explore and quantify costs and benefits of implementing CRA in workplace assessments. Given the increased data needs, potentially more complex risk assessment methods, and training requirements for implementing CRA in the workplace, incentives should be identified for both workers and employers to fully embrace this approach to risk assessment.
The needs and challenges outlined here will be important to inform CRA development going forward. A sustained effort will be needed to continue the development of the underlying science and to implement CRA within OSH fields. A phased approach to program development might include research funding for pilot studies assessing information needs, costs, and benefits from employer, OSH professional, and worker perspectives. Results from the pilot research can inform: 1) methods development; 2) education campaigns to raise awareness of cumulative risk approaches; 3) trainings to disseminate data and methods; 4) policy development to provide incentives as needed for CRA program implementation; and 5) advanced research.
The Total Worker Health® (TWH) program at NIOSH represents a successful model for program development that could be used in developing CRA approaches. TWH policies, program and practices seek to integrate workplace interventions that protect workers' safety and health with activities that advance their overall well-being (NIOSH, 2015). For example, the TWH concept promotes research into how new patterns of employment, and emerging types of work restructuring, affect overall worker health, safety and well-being. This perspective recognizes that new patterns of work organization and nonstandard employment arrangements, and their link to illness and injury, are an important occupational exposure that needs investigation. At the same time, NIOSH recognizes that non-occupational exposures and occupational exposures can act together to produce worker illness and injury (NIOSH, 2015); a concept embodied in CRA. The development and application of CRA as an OSH approach would complement and help better inform TWH interventions (Dotson et al., 2017). Maintaining worker health and workplace safety in the context of a dynamic economy requires flexibility and adoption of new tools and approaches, such as CRA.
Acknowledgements
This work was supported in part by a National Institute for Occupational Safety and Health Interagency Personnel Agreement with author Fox (15IPA1518041).
References
- Agency for Toxic Substances and Disease Registry, 2004. Guidance manual for the assessment of joint toxic action of chemical mixtures. https://www.atsdr.cdc.gov/interactionprofiles/ipga.html, Accessed date: 30 October 2017. [Google Scholar]
- American National Standards Institute, 2012. American National Standard for Occupational Health and Safety Management Systems, Appendix F: Risk Assessment. American National Standards Institute, New York, NY. [Google Scholar]
- American Society for Quality, 2017. What is the ISO 14000 standards series? http://asq.org/learn-about-quality/iso-14000/, Accessed date: 7 July 2017. [Google Scholar]
- Americans with Disabilities Act (42 USC 42 U.S.C. § 12101 and amendments P.L. 110– 325) https://www.ada.gov/pubs/ada.htm, Accessed date: 31 October 2017. [Google Scholar]
- Asfaw A, Pana-Cryan R, Rosa R, 2012. Paid sick leave and nonfatal occupational injuries. Am. J. Public Health 102 (9), e59–e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benavides FG, Benach J, Muntaner C, Delclos GL, Catot N, Amable M, 2006. Associations between temporary employment and occupational injury: what are the mechanisms? Occup. Environ. Med 63 (6), 416–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry LL, Mirabito AM, Baun WB, 2010. What's the hard return on employee wellness programs? In: Harvard Business Review,. https://hbr.org/2010/12/whats-the-hard-return-on-employee-wellness-programs, Accessed date: 11 July 2017. [PubMed] [Google Scholar]
- Boden LI, Spieler EA, Wagner GR, 2016. The changing structure of work: implications for workplace health and safety in the US. https://www.dol.gov/asp/evaluation/completed-studies/Future_of_work_the_implications_for_workplace_ health_and_safety.pdf, Accessed date: 21 June 2017. [Google Scholar]
- Bradshaw M, Ellison CG, 2010. Financial hardship and psychological distress: exploring the buffering effects of religion. Soc. Sci. Med. 71 (1), 196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics, 2017. 2016 survey of occupational injuries and illnesses charts package. https://www.bls.gov/iif/osch0060.pdf, Accessed date: 18 January 2018. [Google Scholar]
- Burgess PA, 2007. Optimal shift duration and sequence: recommended approach for short-term emergency response activations for public health and emergency management. Am. J. Public Health 97 (Suppl. 1), S88–S92. http://dx.doi.org/10.2105/AJPH. 2005.078782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt S, Crombie K, Jin Y, Wurzelbacher S, Ramsey J, Deddens J, 2011. Workplace and individual risk factors for carpal tunnel syndrome. Occup. Environ. Med. 68 (12), 928–933. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2016. Health, United States, 2016 - individual charts and tables. Age-adjusted death rates for selected causes of death, by sex, race, and Hispanic origin: United States, selected years 1950–2015. https://www.cdc.gov/nchs/data/hus/2016/017.pdf, Accessed date: 26 January 2018. [Google Scholar]
- Dotson S, Chosewood LC, Middendorf P, 2017. Integrating NIOSH Efforts to Protect Workers: Linking Exposome, Cumulative Risk Assessment, and Total Worker Health®. Society for Risk Analysis Annual Conferencehttp://birenheide.com/sra/2017AM/program/singlesession.php3?sessid=P&order=122#122, Accessed date: 22 January 2018. [Google Scholar]
- Du Y, Xu X, Chu M, Guo Y, Wang J, 2016. Air particulate matter and cardiovascular disease: the epidemiological, biomedical and clinical evidence. J. Thorac. Dis 8 (1), E8–E19. 10.3978/j.issn.2072-1439.2015.11.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enchautegui ME, 2013. Nonstandard work schedules and the well-being of low-income families. http://www.urban.org/sites/default/files/publication/32696/412877-Nonstandard-Work-Schedules-and-the-Well-being-of-Low-Income-Families.PDF, Accessed date: January 2020. [Google Scholar]
- Evans RG, Stoddart GL, 1990. Producing health, consuming health care. Soc. Sci. Med. 31, 1347–1363. [DOI] [PubMed] [Google Scholar]
- Finkelstein E, Fiebelkorn IC, Wang G, 2005. The costs of obesity among full-time employees. Am. J. Health Promot. 20 (1), 45–51. [DOI] [PubMed] [Google Scholar]
- Finkelstein E, DiBonaventura M, Burgess SM, Hale BC, 2010. The costs of obesity in the workplace. J. Occup. Environ. Med 52 (10), 971–976. http://dx.doi.org/10. 1097/JOM.0b013e3181f274d2. [DOI] [PubMed] [Google Scholar]
- Food Quality Protection Act of 1996, P.L. 104–170 https://www.epa.gov/laws-regulations/summary-food-quality-protection-act, Accessed date: 26 October 2017. [Google Scholar]
- Fox MA, Groopman JD, Burke TA, 2002. Evaluating cumulative risk assessment for environmental justice: a community case study. Environ. Health Perspect 110 (Suppl. 2), 203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox MA, Brewer LE, Martin L, 2017. An overview of literature topics related to current concepts, methods, tools, and applications for cumulative risk assessment (2007–2016). Int. J. Environ. Res. Public Health 14 (4), 389 http://www.mdpi.com/1660–4601/14/4/389/pdf Accessed date: 30 October 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genetic Information Nondiscrimination Act of 2008, P.L. 110-233 https://www.eeoc.gov/laws/statutes/gina.cfm, Accessed date: 26 October 2017. [Google Scholar]
- Gmel G, Rehm J, 2003. Harmful alcohol use. http://pubs.niaaa.nih.gov/publications/arh27-1/52–62.htm Accessed date: 26 October 2017. [Google Scholar]
- Goetzel RZ, Henke RM, Tabrizi M, Pelletier KR, Loeppke R, Ballard DW, Grossmeier J, Anderson DR, Yach D, Kelly RK, McCalister T, Serxner S, Selecky C, Shallenberger LG, Fries JF, Baase C, Isaac F, Crighton KA, Wald P, Exum E, Shurney D, Metz RD, 2014. Do workplace health promotion (well-ness) programs work? J. Occup. Environ. Med 56 (9), 927–934. 10.1097/JOM.0000000000000276. [DOI] [PubMed] [Google Scholar]
- Goetzel RZ, Fabius R, Fabius D, Roemer EC, Thornton N, Kelly RK, Pelletier KR, 2016. The stock performance of C. Everett Koop award winners compared with the Standard & Poor’s 500 Index. J. Occup. Environ. Med 58 (1), 9–15. http://dx.doi. org/10.1097/JOM.0000000000000632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon R, Bloxham S, 2016. A systematic review of the effects of exercise and physical activity on non-specific chronic low back pain. Healthcare 4 (2), 22 http://dx.doi. org/10.3390/healthcare4020022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Insurance Portability and Accountability Act of 1996. P.L. 104–191 https://www.gpo.gov/fdsys/pkg/PLAW-104publ191/pdf/PLAW-104publ191.pdf, Accessed date: 26 October 2017. [Google Scholar]
- Howard J, 2017. Nonstandard work arrangements and worker health and safety. Am. J. Ind. Med. 60, 1–10. 10.1002/ajim.22669. [DOI] [PubMed] [Google Scholar]
- Katz LF, Kreiger AB, 2016. The rise and nature of alternative work arrangements in the United States, 1995–2015. http://scholar.harvard.edu/files/lkatz/files/katz_ krueger_cws_v3.pdf, Accessed date: 21 June 2017mixed. [Google Scholar]
- Kivimaki M, Nyberg ST, Batty GD, Fransson EI, Heikkila K, Alfredsson L, et al. , 2012. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet 380, 1491–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koulova A, Frishman WH, 2014. Air pollution exposure as a risk factor for cardio-vascular disease morbidity and mortality. Cardiol. Rev. 22 (1), 30–36. http://dx.doi. org/10.1097/CRD.0000000000000000. [DOI] [PubMed] [Google Scholar]
- Lax MB, 2016. 2016 the perils of integrating wellness and safety and health and the possibility of a worker-oriented alternative. New Solut. 26 (1), 11–39. http://dx.doi. org/10.1177/1048291116629489. [DOI] [PubMed] [Google Scholar]
- Lentz TJ, Dotson GS, Williams PRD, Maier A, Gadagbui B, Pandalai SP, et al. , 2015. Aggregate exposure and cumulative risk assessment: integrating occupational and non-occupational risk factors. J. Occup. Environ. Hyg. 12, S112–S126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerman RI, Schmidt SR, 2017. An Overview of Economic, Social, and Demographic Trends Affecting the US Labor Market. The Urban Institute, Washington, D.C. Available. https://www.dol.gov/oasam/programs/history/herman/reports/futurework/conference/trends/trendsi.htm, Accessed date: 23 June 2017. [Google Scholar]
- Menzie CA, MacDonell MM, Mumtaz M, 2007. A phased approach for assessing combined effects from multiple stressors. Environ. Health Perspect. 115 (5), 807–816. 10.1289/ehp9331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meraya AM, Sambamoorthi U, 2016. Chronic condition combinations and productivity loss among employed nonelderly adults (18 to 64 years). J. Occup. Environ. Med 58 (10), 974–978. 10.1097/JOM.0000000000000839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moretto A, Bachman A, Boobis A, Solomon KR, Pastoor TP, Wilks MF, Embry MR, 2017. A framework for cumulative risk assessment in the 21st century. Crit. Rev. Toxicol. 47 (2), 85–97. 10.1080/10408444.2016.1211618. [DOI] [PubMed] [Google Scholar]
- National Council on Alcoholism and Drug Dependence, 2015. Drugs and alcohol in the workplace. https ://www.ncadd. org/abo ut-addiction/addiction-update/drugs-and-alcohol-in-the-workplace, Accessed date: 30 October 2017. [Google Scholar]
- National Heart Lung and Blood Institute, 2018. Coronary heart disease. Available. https://www.nhlbi.nih.gov/health-topics/coronary-heart-disease, Accessed date: 12 January 2018. [Google Scholar]
- National Institute for Occupational Safety and Health (NIOSH), 2015. Total Worker Health®: advancing worker safety, health, and well-being. Frequently asked questions. https://www.cdc. gov/niosh/twh/pdfs/faq-for-total-worker-health_2015–03-01-trademark-amended-for-download.pdf, Accessed date: 26 October 2017. [Google Scholar]
- National Research Council (NRC), 1983. Risk Assessment in the Federal Government: Managing the Process. National Academies Press, Washington, DC: Available. http://www.nap.edu/catalog/366/risk-assessment-in-the-federal-government-managingthe-process, Accessed date: 29 January 2016. [Google Scholar]
- NRC, 2008. Phthalates and Cumulative Risk Assessment: The Tasks Ahead. National Academies Press, Washington, DC: Available. https://www.nap.edu/catalog/12528/phthalates-and-cumulative-risk-assessment-the-tasks-ahead, Accessed date: 26 October 2017. [PubMed] [Google Scholar]
- NRC, 2009. Science and Decisions: Advancing Risk Assessment. National Academies Press, Washington, DC: Available. http://www.nap.edu/catalog/12209/science-and-decisions-advancing-risk-assessment, Accessed date: 26 October 2017. [PubMed] [Google Scholar]
- Occupational Safety and Health Act, P.L. 91–596 https://www.osha.gov/pls/oshaweb/owasrch.search_form?p_doc_type=OSHACT&p_toc_level=0&p_keyvalue=OshAct_toc_by_sect.html, Accessed date: 3 October 2017.
- OSHA, 2017a. Recommended practices for safety and health programs. In: Hazard Identification and Assessment,. https://www.osha.gov/shpguidelines/hazard-Identification.html, Accessed date: 3 October 2017.
- OSHA, 2017b. Employer responsibilities. https://www.osha.gov/as/opa/worker/employer-responsibility.html, Accessed date: 25 January 2018.
- Pachucki MC, Goodman E, 2015. Social relationships and obesity: benefits of incorporating a lifecourse perspective. Curr. Obes. Rep. 4, 217–223. 10.1007/s13679-015-0145-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center, 2016. The state of American jobs. http://www.pewsocialtrends.org/2016/10/06/the-state-of-american-jobs/, Accessed date: 21 June 2017. [Google Scholar]
- Puttonen S, Härmä M, Hublin C, 2010. Shift work and cardiovascular disease – pathways from circadian stress to morbidity. Scand. J. Work Environ. Health 36 (2), 96–108. 10.5271/sjweh.2894. [DOI] [PubMed] [Google Scholar]
- Health Rand, 2013. Workplace Wellness Programs Study Final Report. Mattke S, Liu H, Caloyeras J, Huang C, Van Busum K, Khodyakov D, et al. , Santa Monica, CA. https://aspe.hhs.gov/system/files/pdf/76661/rpt_wellness.pdf, Accessed date: 25 January 2018. [PMC free article] [PubMed] [Google Scholar]
- Respiratory Protection Standard, 29 Code of Federal Regulations 1910.134. [Google Scholar]
- Robson L, Stephenson C, Schulte P, Amick B, Chan S, Bielecky A, et al. , 2010. A Systematic Review of the Effectiveness of Training & Education for the Protection of Workers 2010. Institute for Work & Health, Toronto (Cincinnati, OH: National Institute for Occupational Safety and Health. This publication can also be tracked as DHHS (NIOSH) Publication No. 2010–127). [Google Scholar]
- Rooney J, Vanden Heuvel L, 2004. Root cause analysis for beginners. Qual. Prog. 2004, 45–53. [Google Scholar]
- Rosa R, Colligan MJ, 1997. Plain Language About Shiftwork. Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Division of Biomedical and Behavioral Science, Education and Information Division, Cincinnati, Ohio (July 1997). [Google Scholar]
- Saenz R, 2008. A demographic profile of U.S. workers around the clock. http://www.prb.org/Publications/Articles/2008/workingaroundtheclock.aspx, Accessed date: 30 October 2017. [Google Scholar]
- Schulte PA, Pandalai S, Wulsin V, Chun H, 2012. Interaction of occupational and person risk factors in workforce health and safety. Am. J. Public Health 102 (3), 434–448. 10.2105/AJPH.2011.300249.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serra C, Cruz Rodriguez M, Delclos GL, Plana M, Gomez Lopez LI, Benavides FG, 2007. Criteria and methods used for the assessment of fitness for work: a systematic review. Occup. Environ. Med 64, 304–312. 10.1136/oem.2006.029397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CK, Silverstein BA, Bonauto DK, Adams D, Fan ZJ, 2010. Temporary workers in Washington state. Am. J. Ind. Med. 53, 135–145. [DOI] [PubMed] [Google Scholar]
- Society for Risk Analysis (SRA), 2016. Full day workshop: cumulative risk assessment: addressing combined environmental stressors. http://www.sra.org/sites/default/files/pdf/events/SRA%20Final%20Program%20-%20R6.pdf, Accessed date: 26 October 2017. [Google Scholar]
- SRA, 2017. Annual meeting 2017 final program.Full-day workshop. In: Cumulative Risk Assessment: Addressing Combined Environmental Stressors,. http://sra.org/sites/default/files/pdf/events/2017%20SRA%20Final%20Program%20-%20R6.pdf, Accessed date: 12 January 2018. [Google Scholar]
- Steptoe A, Kivimaki M, 2012. Stress and cardiovascular disease. Nat. Rev. Cardiol. 9, 360–370. http: //dx. doi. org/10.1038/nrcardio.2012.45. [DOI] [PubMed] [Google Scholar]
- Sturgeon JA, Arewaskiporn A, Okum MA, Davis MC, Ong AD, Zautra AJ, 2016. The psychosocial context of financial stress: implications for inflammation and psychological health. Psychosom. Med 78, 134–143. http://dx.doi.org/10.1097/PSY. 0000000000000276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundquist K, Malmström M, Johansson S-E, 2004. Neighbourhood deprivation and incidence of coronary heart disease: a multilevel study of 2.6 million women and men in Sweden. J. Epidemiol. Community Health 58, 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits PA, 2011. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 52 (2), 145–161. [DOI] [PubMed] [Google Scholar]
- U.S. EEOC, 2017. Laws enforced by the EEOC. https://www.eeoc.gov/laws/statutes/index.cfm, Accessed date: 26 October 2017. [Google Scholar]
- U.S. Environmental Protection Agency (EPA) Science Policy Council, 1997. Guidance on cumulative risk assessment.In: Part 1. Planning and Scoping,. https://www.epa.gov/risk/guidance-cumulative-risk-assessment-part-1-planning-and-scoping, Accessed date: 26 January 2018. [Google Scholar]
- U.S. EPA, 2003. Framework for Cumulative Risk Assessment. U.S. EPA, Office of Research and Development, National Center for Environmental Assessment, Washington Office, Washington, DC: (EPA/600/P-02/001F). https://www.epa.gov/risk/framework-cumulative-risk-assessment, Accessed date: 29 June 2017. [Google Scholar]
- U.S. EPA, 2007. Concepts, Methods and Data Sources for Cumulative Health Risk Assessment of Multiple Chemicals, Exposures and Effects: A Resource Document. U.S. Environmental Protection Agency, National Center for Environmental Assessment, Cincinnati, OH (EPA/600/R-06/013F). https://cfpub.epa.gov/ncea/risk/recordisplay.cfm?deid=190187, Accessed date: 31 October 2017. [Google Scholar]
- U.S. EPA, 2009. Understanding the role of nonchemical stressors and developing analytic methods for cumulative risk assessments. Available National Center for Environmental Research https://cfpub.epa.gov/ncer_abstracts/index.cfm/fuseaction/display.rfatext/rfa_id/515, Accessed date: 31 October 2017. [Google Scholar]
- U.S. EPA Office of Air Quality, Protection and Standards, 2015. EPA's 2011 national-scale air toxics assessment. Technical support document. https://www.epa.gov/sites/production/files/2015-12/documents/2011-nata-tsd.pdf, Accessed date: 26 October 2017. [Google Scholar]
- U.S. EPA Office of Pesticide Programs, 2002. Guidance on cumulative risk assessment of pesticide chemicals that have a common mechanism of toxicity. https://www.epa. gov/sites/production/files/2015-07/documents/guidance_on_common_mechanism. pdf, Accessed date: 26 October 2017.
- U.S. EPA Office of Water, 2017. How EPA regulates drinking water contaminants. https://www.epa.gov/dwregdev/how-epa-regulates-drinking-water-contaminants, Accessed date: 26 October 2017. [Google Scholar]
- U.S. Equal Employment Opportunity Commission (EEOC), 2000. Enforcement guidance: disability-related inquiries and medical examinations of employees under the Americans with Disabilities Act. https://www.eeoc.gov/policy/docs/guidance-inquiries.html, Accessed date: 26 October 2017.
- Virtanen M, Kivimaki M, Joensuu M, Virtanen P, Elovainio M, Vahtera J, 2005. Temporary employment and health: a review. Int. J. Epidemiol. 34, 610–622. [DOI] [PubMed] [Google Scholar]
- Weinstein M, Susi P, Goldberg M, 2016. The power of local action in occupational health: the adoption of local exhaust ventilation in the Chicago tuckpointing trade. Int. J. Occup. Environ. Health 22 (2), 142–150. 10.1080/10773525.2016.1187476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams PRD, Dotson GS, Maier A, 2012. Cumulative risk assessment (CRA): transforming the way we assess health risks. Environ. Sci. Technol 46 (20), 10868–10874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Economic Forum, 2016. The future of jobs employment, skills and workforce strategy for the fourth industrial revolution. In: The Future of Jobs and Skills: Executive Summary,. http://www3.weforum.org/docs/WEF_FOJ_Executive_Summary_Jobs.pdf, Accessed date: 21 June 2017. [Google Scholar]
- Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. , 2004. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364, 937–952. [DOI] [PubMed] [Google Scholar]