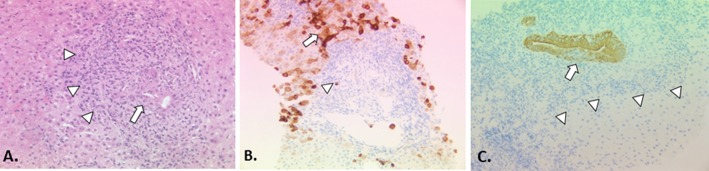
Figure 2.
The histopathology of PBC classical staging systems for PBC divide the histological injury of PBC into four stages: florid duct lesions and portal inflammation without interface activity (stage 1), interface hepatitis, ductular proliferation and periportal fibrosis (stage 2), bridging necrosis or bridging fibrosis (stage 3), and cirrhosis (stage 4).93 These systems are easy to apply and are quite reproducible. However, their practical utility is limited because of the uneven distribution of diagnostic histological lesions of PBC and different disease stages co-existing at any time.93 Furthermore, they incorporate features such as inflammation, which are more appropriately regarded as a manifestation of disease activity (histological ‘grade’) rather than disease progression (histological ‘stage’). A more recent scoring system described by Nakanuma and colleagues sums up individual scores for fibrosis, bile duct loss and severity of chronic cholestasis based on copper-associated protein deposition to assess disease stage and provides a separate system for grading necroinflammatory activity based on cholangitic and hepatitic features.100 Similar to the classical staging systems, the Nakanuma staging system correlates well with clinical and laboratory features. Subsequent studies have suggested that the Nakanuma system is more useful than previously described staging systems in predicting adverse outcomes in patients with PBC101 102 and may also be helpful in predicting treatment responses.79 Another recently described histological scoring system for PBC based on prognostically significant lesions (ie, fibrosis, bile duct loss and lymphocytic interface hepatitis) showed better interobserver agreement and correlation with biochemical abnormalities than traditional scoring systems, but predictive value for adverse outcomes could not be assessed.103 Problems with sampling variability apply to all of the histological staging systems that have been described for patients with PBC, which limits the utility of liver biopsy to assess disease severity in routine clinical practice, but they may still have a role in the context of clinical trials where liver biopsies have been used for risk stratification and as a surrogate marker of treatment outcomes. (A) Early PBC is characterised mainly by portal lesions and mild necroinflammatory changes in the acini. Portal tracts may show cholangiocentric granulomatous inflammation composed of lymphocytes, occasionally numerous plasmacytes, and polymorphs including eosinophils. Lymphoid follicles with germinal centres may form. The lymphoid inflammatory infiltrate extends to the biliary epithelium (cholangitis) (arrow), disrupting the basement membrane sometimes leading to bile duct destruction (florid duct lesion). Granulomas, ranging from small collections of histiocytes to easily discerned non-caseating epithelioid granulomas, may be present in portal tracts near damaged bile ducts and less often in the acini. In the progressive lesion of PBC, lymphocytic interface hepatitis may predominate blurring the portal tract boundary and extending into the acinus (arrowheads). Ductular proliferation at the portal-parenchymal interface may be prominent with associated stromal oedema and neutrophilic inflammation. Parenchymal necroinflammatory activity and hepatocellular injury are usually mild. Small and large cell change and hepatocellular regeneration may be seen (H&E, x20). (B) Keratin 7 immunostaining highlights loss of bile ducts (arrowhead indicates a keratin 7-positive bile duct epithelial remnant) leading to chronic cholestasis with features of feathery degeneration, Mallory-Denk bodies, copper-associated protein deposition in periportal/periseptal hepatocytes (cholate stasis), cholestatic rosettes and biliary metaplasia of hepatocytes (arrow) (keratin 7 immunostain, DAB chromagen, x10). (C) Loss of canals of Hering in acinar zone 1 (arrowheads) detected by keratin 19 immunostaining has recently been proposed as an early feature of PBC in the absence of the classic destructive biliary lesions.104 Focal intraepithelial inflammation (cholangitis) is noted in the K19-positive interlobular bile duct (arrow) (keratin 19 immunostain, DAB chromagen, x20).