Abstract
Background:
Vascular access is an important part of many patient care management plans, but has unwanted risks. A working group led by the Infection Prevention Society (IPS) produced a Vessel Health and Preservation (VHP) Framework. Based on current evidence, a framework was developed for frontline staff to assess and select the best vascular access device to meet the individual patient’s needs and to preserve veins for future use.
Methods:
Using the Outcome Logic Model, we conducted an evaluation of the short- and medium-term outcomes with regards to the impact and success of the VHP Framework.
Results:
This evaluation found that many respondents were aware of the framework and were using it in a range of different ways. Participants saw the framework as being most beneficial to help decisions on device choice and peripheral vein assessment. However, the framework has not fully reached its intended audience.
Discussion:
Many positive outcomes were reported as a result of using the VHP Framework including improving clinical practice as it relates to the VHP elements. However, further work is required to find the tools to extend the reach of the framework and assist healthcare teams to be able to fully implement it within their clinical settings.
Keywords: Vascular access, Vessel Health and Preservation, patient safety, competence, healthcare-associated infections, infection prevention
Introduction
Reliable and safe vascular access is an integral part of today’s healthcare; with vascular access devices being utilised for a vast variety of therapies (Hallam et al., 2016; Jackson et al., 2013; Maki et al., 2006). Vascular access and therapy can potentially save lives; however, its utilisation also has the potential to lead to a wide range of complications, some of which can be life-threatening (Loveday et al., 2014). Vascular access devices are now considered to be the single most important cause of healthcare-associated blood stream infections (Hadaway, 2012; Moureau et al., 2012).
Inexperience and poor decision-making has been identified as an issue that can lead frontline staff automatically opting for a peripheral vascular catheter (PVC) when intravenous therapy is required rather than considering which is the most appropriate and safest device for their patient (Hallam et al., 2016; Jackson et al., 2013). The concept of Vessel Health and Preservation (VHP) originated in the US with the ground-breaking work of Moureau et al. (2012). They recognised the need for the development of a programme which incorporated evidence-based practices, focusing on the timely, intentional and proactive selection of the right vascular access device to improve patient care, safety and outcomes.
Development of the VHP Framework
Evidence-based guidance on preventing complications resulting from the use of vascular access device (VAD) usage has long been available (Loveday et al., 2014). However, in the UK, there was an absence of simple-to-use tools which focused on the preservation of vessel health as well as preventing the most recognised complications. A focus on preserving the health of vessels has distinct advantages over a traditional infection prevention approach. An infection prevention approach focuses on aseptic technique to reduce the infection risks when inserting a peripheral cannula. However, a VHP approach includes, in addition to infection prevention, an assessment of the patient’s vessels, predicted cannula usage (duration and drugs) so that the cannula and vein selected results in the least possible vessel harm, secondary complications and unnecessary pain/inconvenience for the patient.
With the development of a VHP tool in the US (Moureau et al., 2012), the Infection Prevention Society’s (IPS) Intravenous (IV) Special Interest Group decided to explore the tool for suitable adaption and adoption in the UK. A small group was set up and a UK VHP framework developed (Hallam et al., 2016). As the prevention of IV complications covers various specialties and professional societies, there was, and continues to be, full engagement with the Royal College of Nursing and the National Infusion and Vascular Access Society (NIVAS) in this work. The UK VHP Framework provides practitioners with a decision-making tool to ensure the most appropriate vein and vascular access device are used to prevent all VAD complications and maintain the health of patients’ vessels. Having developed the UK VHP Framework, there was a clear need to evaluate the extent to which the UK VHP Framework was known to and used by practitioners.
Aim
The aims of this evaluation study were to consider how the information about the VHP Framework was disseminated, who it has reached, if it is being used and how it is being used. In order to address the aims, the following research questions were developed:
Has the VHP Framework been disseminated and communicated to the appropriate individuals and teams?
Is the VHP Framework being promoted to frontline clinical healthcare workers by infection prevention and control teams and IV teams?
Is the VHP Framework being used in practice?
How is the VHP Framework being used in practice?
What are the barriers and challenges when using the VHP Framework in practice?
Methodology
The Outcome Logic Model (OLM) was selected for this study (W.K. Kellogg Foundation, 2004). This is a widely used model which enables the evaluation of the effectiveness and efficiency of planned programmes or frameworks by providing a roadmap or pathway for measuring the right outcomes at the right time (Burnett et al., 2014; Hayes et al., 2011). Additionally, the OLM helps to systematically determine what elements or aspects of a programme or framework are achieving what they intended or which ones are not (Armstrong and Barison, 2006). Thus, it helps guides and focus future work and leads to improved planning and management. The OLM comprises three major components: inputs (the resources consumed by the programme); outputs (what did we do [activities] and who did we reach [participants] and outcomes [what are the results of the programme], which are developed in the context of the program’s assumptions and external factors (Frechtling, 2007; Mederiros et al., 2005).
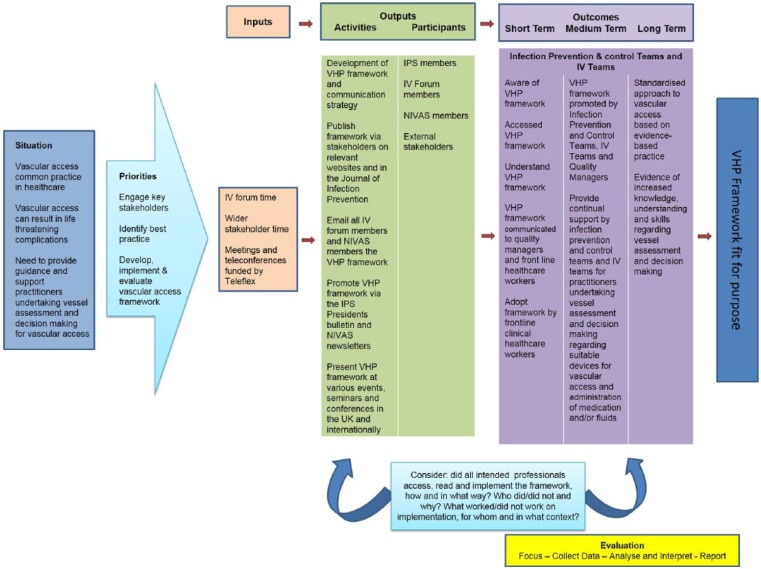
The VHP Framework was published and communicated to a range of practitioners, teams and wider stakeholders early in 2016. Evaluating the short-term outcomes at this time using the OLM enabled us to systematically consider all elements of the planning and implementation stages of the framework and thus guide and help focus our next programme of work. Figure 1 presents a visual representation of the three major components in relation to this study.
Figure 1.
The Outcome Logic Model for evaluation of the Vessel Health and Preservation Framework.
Figure 1 illustrates the OLM populated with each component of the VHP Framework from the initial development to the long-term outcomes. In order to evaluate the short-term outcomes, the generation, analysis and interpretation of appropriate data are required.
Inputs
Inputs are the investments made in order to effectively develop the VHP Framework. This included time dedicated by the IPS IV forum and wider stakeholder engagement from individuals such as vascular access specialists, anaesthetists, pharmacists, NIVAS and RCN members. Funding was provided by Teleflex to allow regular meetings and teleconferences.
Outputs
Outputs within the OLM consist of activities which were undertaken following the completion of the VHP Framework and the participants who were the target audience reached by the framework. Setting out these activities and related participants allows the visualisation of links between the situation and the outcomes of the framework.
Outcomes
Evaluation indications and questions were set to determine the outcomes of the framework and an evaluation plan identified indicators relevant to the short-, medium- and long-term outcomes. This initial evaluation focused mainly on the short-term outcomes, with possibly some impact on the medium-term outcomes. In order to effectively understand these outcomes, data needed to be generated and analysed. These findings would then be used to inform further development and improvements of the framework (Kazi, 2003).
Research design
Methods
This evaluation study adopted a quantitative approach, using a survey questionnaire to generate numerical data (Creswell, 2014). An electronic questionnaire was created using SurveyMonkey™ and available to complete online. It was established that this was the most appropriate systematic method to generate a significant amount of data from a relatively large and diverse population (Nulty, 2008). For the purpose of this study, both closed and open-ended questions were used to ensure the evaluation questions were answered fully (Table 1). The development of the questionnaire was informed by the literature and the evaluation aims and questions. The questionnaire was piloted with practitioners, managers and academics and refined before distribution. All data generated from the questionnaire were included in the analysis.
Table 1.
Evaluation questionnaire.
| 1. Are you a member (tick all that apply) a. IPS b. IPS IV Forum c. NIVAS d. RCN |
| 2. Are you aware of the existence of the UK Vessel Health and Preservation (VHP) Framework? a. If yes, where did you hear about the VHP Framework? |
| 3. If you have seen the VHP Framework did you find it easy to understand? a. If no, what was difficult? |
| 4. Are you using part or all of the VHP Framework in practice? a. If not, why? |
| 5. What did you perceive to be the impact and benefit of using the part or the entire VHP Framework prior to use? |
| 6. In what context are you using the VHP Framework a. As a whole framework to improve vascular access b. In part(s) to improve i. Vascular device choice ii. Peripheral vein assessment iii. Knowledge of drug suitability iv. Daily evaluation of vascular device c. Assessing IV team and service needs d. Business case development e. For education and training programmes f. Other (specify) |
| 7. If you are using the whole VHP Framework or just using sections? a. Which part(s) are you using and why? |
| 8. What benefits have you seen since using the VHP Framework? |
Sample
The study population were members of IPS (including the IPS IV forum), NIVAS and RCN as these were the main individuals targeted in dissemination of information about the VHP framework. All individuals were identified through the IPS and NIVAS databases and were contacted by email. Further potential participants were also identified through attendance of presentations on the VHP framework at events and conferences. A SurveyMonkey link, an explanation of the study and a participant information leaflet were provided in the email. Participants were given four weeks to complete the survey and reminders were given regularly via email and social media. Participants who were using the framework were also invited to express interest in a second phase of the study and provide their name and contact details. This second phase used a qualitative approach to explore the impact of the VHP Framework. All individuals who completed the questionnaire were entered into a prize draw to win £50 (each for five people).
Ethical considerations
The evaluation proposal was approved by the IPS Board. Ethical approval was not necessary as the nature of this proposed study was an evaluation. A full explanation of the study was provided to all participants on receiving the online survey monkey questionnaire. Completion of the questionnaire served as consent. All electronic data were kept on a password-protected computer and laptop, which was kept in a locked office and was only accessible by the evaluation team. No individual is identifiable from written reports of this study.
Data analysis
Data were analysed using SPSS statistical software using descriptive statistics.
Results
The initial email invitation was sent out to 2354 individuals. A total of 270 questionnaires were submitted via the online tool, corresponding to a response rate of 12%. As survey participants were not required to answer all questions, responses to individual survey items varied widely, with a low number of responses for some questions.
Most of the respondents were members of the IPS (73%; 182/270) and/or the RCN (66%; 163/270). Two-thirds of respondents were aware of the VHP Framework (64%, n = 170/265). Multiple routes were cited as sources of information about the VHP Framework, most frequently conferences 33% (n = 57/175) or professional body communication lists 32% (n = 56/175). Others included study days or training courses 13% (n = 23/175), colleagues 12% (n = 21/175), scientific journal 5% (n = 8/165) and the Internet 3% (n = 5/175).
With the exception of 7% of respondents (n = 12/164), the VHP framework was considered easy to understand. For the 12 who indicated difficulty understanding the VHP framework, areas of difficulty included an unclear poster format 50% (n = 6/12), too complex 33% (n = 4/12) and too lengthy 17% (n = 2/12). Notably, nearly half the respondents indicated that they were not using the VHP Framework at the time of the survey (49%, n = 78/159). Only 10% (n = 16/159) indicated that they were actively using all of the VHP Framework. Only 32 respondents provided information on the extent to which they were using the VHP Framework in clinical practice. A number of respondents indicated that the framework was used either as a training (22%, n = 7/32) or as a reference tool (13%, n = 4/32) (Figure 2).
Figure 2.
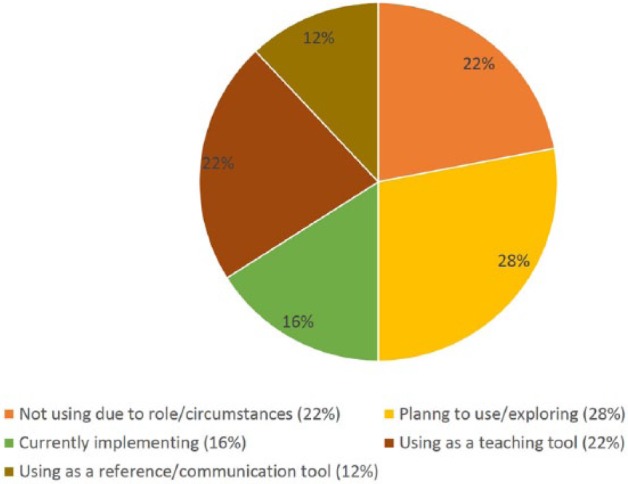
To what extent are you using the VHP Framework in practice?
In terms of perceptions before actual use of the VHP Framework, respondents predominantly expected the framework to improve clinician knowledge/decision-making and clinical practice (Figure 3).
Figure 3.
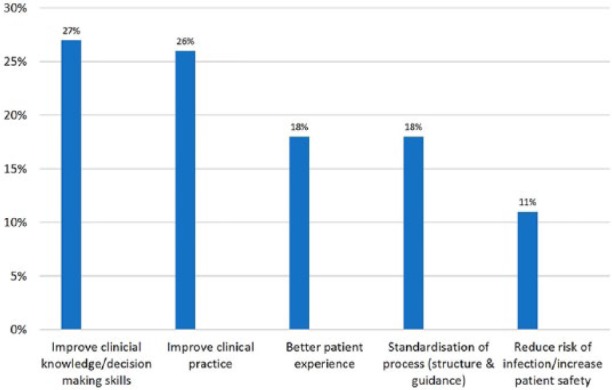
What did you perceive to be the impact and benefit of using part or the entire VHP Framework before use?
Moreover, 64% (n = 38/59) of respondents indicated that they used the framework to improve vascular access, 47% (n = 28/59) to assess the IV team and service needs, 32% (n = 19/59) for business case development and 78% (n = 46/59) for education and training programmes. Most respondents indicated that they used the framework to help them choose a vascular device (86%, n = 49/57) and perform a peripheral vein assessment (81%, n = 46/57). Four respondents indicated additional contexts where the framework was used in their practice, including promotion of quality and safety work, reduction in number of requests for blood samples and reduction of infection rates from multiple cannulation.
The part of the VHP Framework most frequently used by survey respondents was ‘vein assessment’ (24%, n = 16/68), followed by ‘device selection’ (16%, n = 11/68) and ‘right line decision tool’ (15%, n = 10/68) (Figure 4).
Figure 4.
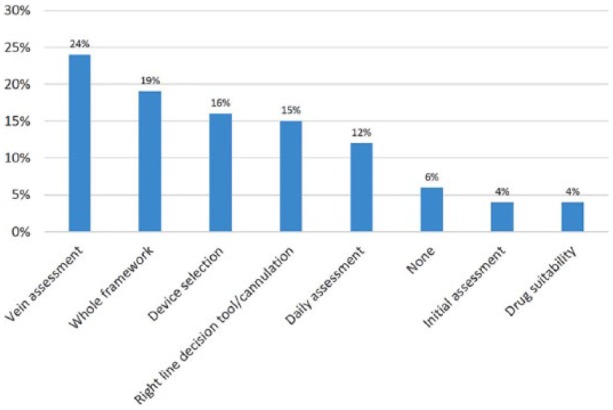
Which part(s) of the VHP Framework are you using and why?
When benefits from actual use of the VHP Framework were considered, 61 responses to this question were received. The majority of respondents indicated that the framework improved their clinical practice (23%, 14/61) and/or increased their knowledge and confidence in decision-making (23%, 14/61). Up to 35% (25/61) of respondents could not find a benefit, most frequently because they felt unable to comment due to the short period between implementation of the framework and participation in the survey (Figure 5).
Figure 5.
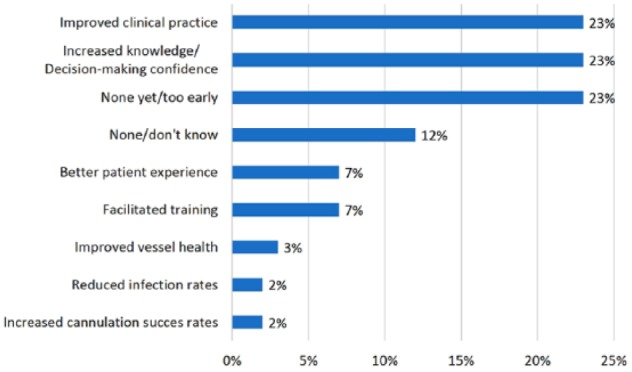
What benefits have you seen since using the VHP Framework?
Of those who chose to not use the VHP Framework in practice, 34% (n = 24/71) indicated that either cannulation was not part of their clinical role or they themselves did not have a clinical role (16%, n = 11/71). A sizable 35% (n = 25/71) indicated that they were exploring the possibility of future implementation of the framework.
Discussion
Vascular access and the administration of intravenous drugs and fluids plays a key role in the care and management of many patients (Gabriel, 2013). The development and implementation of the VHP Framework aimed to support practitioners undertaking vessel assessment and their decision-making in relation to suitable devices for vascular access in addition to the administration of medication and/or fluids.
This evaluation study allowed us to understand if the communication strategy was effective in enabling the VHP Framework to reach the anticipated audience. Understanding whether the VHP Framework reached who it was intended for and knowing if they are using it and how they are using it will help the future plans for the framework. Our findings demonstrated that while two-thirds of respondents were aware of the framework, only half the respondents were, at the time of the survey, actually using the framework. This suggests that further work is required to find the tools to assist healthcare teams to be able to implement the framework within their hospitals.
Although the greatest number of respondents were members of the IPS and RCN and the smaller number were NIVAS members, NIVAS has a significantly smaller membership due to its specialist area. Virtually all NIVAS members will be involved with vascular access compared to many of the IPS and RCN members who will not be involved with vascular access in their work role. It was clear that respondents see the framework as being the most beneficial to help decisions on device choice and peripheral vein assessment. They highlighted many positive outcomes since using the VHP Framework, including improving clinical practice as it relates to the VHP elements. For example, increasing their knowledge regarding vein assessment and device selection would, they felt, improve their decision-making and the confidence they have in their decision-making.
This survey has some limitations due to the low response rate in many of the individual questions. Overall, it has shown that the VHP framework has reached a range of healthcare staff through conferences and study days. However, the framework has yet to reach the entire desired audience and further communication and dissemination is required. Once this has been achieved, an additional evaluation may improve on the response rate. The survey failed to identify the barriers and challenges to using the VHP Framework, with many of the respondents stating they were not using the framework as it was not part of their role or they were not in a clinical role. Addressing this issue needs to be the next step of the VHP Framework journey. Nevertheless, a small number of respondents did state they were exploring the possibility of implementing the VHP Framework. It would therefore also be beneficial to identify methods and tools to help support individuals and teams with implementation.
Acknowledgments
We thank the participants for taking part in this evaluation, the Infection Prevention Society for funding this work, the IPS R&D committee for feedback during the survey development and Dr Greg Kotronoulas for analysing the data.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Peer review statement: Not commissioned; blind peer-reviewed.
References
- Armstrong EG, Barison SJ. (2006) Using an outcomes-logic-model approach to evaluate a faculty development program for medical educators. Academic Medicine 81: 483–488. [DOI] [PubMed] [Google Scholar]
- Burnett E, Curran E, Loveday HP, Kiernan M, Tannahill M. (2013) The outcome competency framework for practitioners in infection prevention and control: use of the outcome logic model for evaluation. Journal of Infection Prevention 15: 14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JW. (2014) Research Design Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Frechtling JA. (2007) Logic modeling methods in program evaluation. San Francisco, CA: Jossey-Bass. [Google Scholar]
- Gabriel J. (2013) Long term central venous device selection. Nursing Times 109: 12–15. [PubMed] [Google Scholar]
- Hadaway L. (2012) Short peripheral intravenous catheters and infections. Journal of Infusion Nursing 35: 230–240. [DOI] [PubMed] [Google Scholar]
- Hallam C, Weston V, Denton A, Hill S, Bodenham A, Dunn H, Jackson T. (2016) Development of the UK Vessel Health and Preservation (VHP) framework: a multi-organisational collaborative. Journal of Infection Prevention 17: 65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes H, Parchman ML, Howard R. (2011) A logic model framework for evaluation and planning in a primary care practice-based research network (PBRN). Journal of the American Board of Family Medicine 24: 576–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson T, Hallam C, Corner T, Hill S. (2013) Right line, right patient, right time: every choice matters. British Journal of Nursing 22: S26–28. [DOI] [PubMed] [Google Scholar]
- Kazi M. (2003) Realist evaluation for practice. British Journal of Social Work 33: 803–818. [Google Scholar]
- Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, Browne J, Prieto J, Wilcox M. (2014) Epic3: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals. Journal of Hospital Infection S86: S1–S70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maki G, Daniel M, Kluger M, Crnich CJ. (2006) The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clinic Proceedings 81: 1159–1171. [DOI] [PubMed] [Google Scholar]
- Medeiros LC, Butkus SN, Chipman H, Cox RH, Jones L, Little D. (2005) A logic model framework for community nutrition education. Journal of Nutrition Education and Behavior 37: 197–202. [DOI] [PubMed] [Google Scholar]
- Moureau NL, Trick N, Nifong T, Perry C, Kelley C, Leavett M, Gordan SM., Wallace J, Harvill M, Biggar C, Doll M, Papke L, Benton L, Phelan DA. (2012) Vessel health and preservation (Part 1): a new evidence-based approach to vascular access selection and management. Journal of Vascular Access 13: 351–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nulty DD. (2008) The adequacy of response rates to online and paper surveys: what can be done? Assessment & Evaluation in Higher Education 33 301–314. [Google Scholar]
- W.K. Kellogg Foundation. (2004) Using logic models to bring together planning, evaluation and action: logic model development guide. Battle Creek, MI: W.K. Kellogg Foundation. [Google Scholar]