Abstract
Introduction
Hypertension is one of the main risk factors of cardiovascular diseases. The first aim of the study was to evaluate the prevalence, awareness and treatment of hypertension as well as treatment effectiveness (blood pressure < 140/90 mm Hg) in a representative sample of the Polish population over the age of 19, examined in the WOBASZ II program. The second aim was to assess the changes in these parameters between 2003–2005 (WOBASZ study) and 2013–2014 in adults aged 20–74.
Material and methods
Sampling was performed in three stages, stratified according to voivodeship (province), type of commune, and gender. Finally, the study included 6163 persons (3406 women and 2757 men) examined in the years 2013–2014 (aged ≥ 19 years). For comparison the data from 14 755 persons (7783 women and 6452 men aged 20–74 years) examined in the years 2003–2005 were used.
Results
In the years 2013–2014, the age-standardized prevalence of hypertension, awareness, treatment and control was 42.7%, 59.3%, 46.1%, and 23% respectively. In the last decade an increase in the prevalence of hypertension (relative ratio (RR) 1.12; 95% confidence interval (CI): 1.07–1.18), treatment (RR = 1.26; 95% CI: 1.17–1.36) and control (RR = 2.16; 95% CI: 1.9-12.45) was found. In contrast, the awareness decreased nonsignificantly (RR = 0.98; 95% CI: 0.92–1.05).
Conclusions
The prevalence of hypertension in Poland is high, and increased by about 12% in 10 years. Although the number of treated patients and blood pressure control improved nearly twofold over the last decade, this is still below expectations. Efforts to improve the diagnosis and effective treatment of hypertension in Poland should still be intensified.
Keywords: health examination surveys, clinical epidemiology, prevalence of hypertension, awareness of hypertension, treatment of hypertension, control of hypertension
Introduction
All over the world, hypertension is the main modifiable risk factor for all cardiovascular disease, including coronary artery disease, stroke, heart failure, peripheral artery disease, and renal failure [1]. According to the WHO, an elevated blood pressure (BP) is the leading risk factor of death in the world [2]. According to American epidemiological studies, hypertension is responsible for up to 40.6% of cardiovascular mortality, while smoking is responsible for 13.2%, poor diet for 11.9%, insufficient physical activity for 8.8%, and elevated plasma glucose for 8.8% [3]. It is estimated that mortality due to cardiovascular diseases and stroke caused by elevated pressure is doubled with an increase in systolic BP (SBP) of 20 mm Hg and diastolic pressure of 10 mm Hg. It was demonstrated in meta-analyses of Hebert and MacMahon including randomized clinical trials concerning pharmacological treatment of patients with mild to moderate hypertension that even a slight decrease in mean diastolic BP (DBP) of 3–6 mm Hg resulted in a significant reduction in stroke incidence by 40–42% and cardiovascular events by 16–25% [4]. The study conducted by Farley demonstrated that about a 10% improvement in diagnosis and treatment of hypertension prevented 14,000 deaths a year in a population of adult Americans aged 25–75. For comparison, a 10% improvement in diagnosis and treatment of elevated low-density lipoprotein (LDL) cholesterol level, or an implementation of aspirin treatment in patients with high risk of cardiovascular mortality prevented 8,000 deaths [5].
In Poland, the share of cardiovascular diseases (CVDs) as a cause of mortality has been gradually decreasing since 1991. In 1991, CVDs were the cause of 47.7% of deaths (42.8% in men and 53.3% in women) [6]. In 2014, 169 735 people died due to CVDs (441.1/100 000). They were responsible for 45.8% of all deaths of Poles (40.9% in men and 51.1% in women) [7]. The age-standardized factor of mortality due to CVDs decreased by 27% in men and 30% in women in the years 1991–2013 [6]. A meta-analysis conducted by Kearney, which included studies on adults from 30 countries, demonstrated that the prevalence of hypertension in adults in the world in 2000 was 26.4% (972 million people), and it is estimated to grow by 2025 to 29.2% (1650 million patients) [8]. Based on the results of the NATPOL 2011 study, an increase in the number of hypertensive patients aged 18–79 to about 14 million is predicted in Poland by the year 2035 (after taking account of the Central Statistical Office (CSO) demographic forecast and directions of changes in the prevalence of risk factors in the period 2002 to 2011 (the aim of the Polish nationwide NATPOL 2011 study was assessment of prevalence and control of selected risk factors of CVD including hypertension)) [6]. Knowledge of the prevalence, detection and efficiency of hypertension treatment at the population level is extremely important for planning the strategy to reduce cardiovascular diseases incidence and health protection expenditures. The largest Polish epidemiological study evaluating the health status of Poles is the WOBASZ study (Multi-center National Population Health Examination Survey), whose first edition was conducted in 2003–2005, and the second in 2013–2014.
The first aim of the study was to evaluate the prevalence, awareness and treatment of hypertension as well as treatment effectiveness (BP < 140/90 mm Hg) in a representative sample of the Polish population over the age of 19 years, examined in the WOBASZ II program.
The second aim was to assess changes in these parameters in 2003–2005 and 2013–2014 in adults aged 20–74.
Material and methods
The methodology (study protocol, training materials, a set of questionnaires and instructions concerning every element of the study) was prepared using the combined experience of the POL-MONICA project (Polish part of the WHO MONICA Project), first edition of WOBASZ and guidelines of the European Health Examination Survey (EHES) [9, 10]. The WOBASZ II program was accepted by the Field Bioethics Committee of the Institute of Cardiology in Warsaw. Finally, the WOBASZ study included 14 755 people (7783 women and 6972 men) and the WOBASZ II study included only 6163 patients (3406 women and 2757 men; initially it was intended to examine 15 120 people), due to the participation rate that was 76.9% and 45.5% respectively. WOBASZ II included the same municipalities as the first edition, but the randomized sample of individual participants was independent. Sampling had three stages, stratified according to voivodeships (provinces), type of communes, and gender. A detailed description of the study methodology is provided in a separate paper [6, 10, 11].
Blood pressure measurements were performed according to the recommendations of PTNT 2015 (Polish Society of Hypertension) [12] consistent with the recommendations of the ESC/ESH 2013 (European Society of Cardiology/European Society of Hypertension) [13].
Pressure measurements took place during a single visit, and were performed using the automatic device AND UA-631 (in the WOBASZ study the automatic device OMRON M-51 was used [10]), approved by the AAMI (Association for the Advancement of Medical Instrumentation). Arm circumference was measured before pressure measurement, in order to select an appropriate width of the cuff. The measurement was performed three times at two-minute intervals on the right upper arm in a sitting position after 5 min of rest (in the WOBASZ study the BP measurement protocol was identical [10]). An average value from the second and third measurement were accepted for an evaluation of BP value in the examined patient. In cases where three BP measurements were not performed, a single measurement or an average of two measurements was taken into account.
The following definitions were accepted according to the recommendations of the World Hypertension League Expert Committee [14]:
Hypertension is defined as presence of SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg or use of BP-lowering medication (regular for last 2 weeks).
-
Awareness of hypertension is defined as the proportion of patients with hypertension who report either having been diagnosed with hypertension by a health professional or who report taking medication for high BP to hypertensive patients (affirmative response to the questions: “Have you ever been told by a doctor that you had hypertension, also called high blood pressure?” and “Have you ever taken medicine prescribed because of high blood pressure?”
Treatment of hypertension is defined as the proportion of patients with hypertension who report taking medication for high BP to hypertensive patients (affirmative response to the questions: “Have you taken this medicines regularly during the last 2 weeks?”).
Controlled hypertension is defined as the proportion of patients with hypertension who both report taking medication for high BP and have SBP < 140 mm Hg and DBP < 90 mm Hg to hypertensive patients.
We are aware that ESH BP categories can be applied only to an untreated population. The described stages of hypertension concerned the whole population, including those treated. However, the same methodology of presentation of results was adopted in a previous publication on the WOBASZ study. Thanks to that we obtained results we could compare and could evaluate changes in the prevalence of raised blood pressure in the Polish population.
The patients were qualified for the group with optimal pressure, according to the recommendations of PTNT 2015 and ESC/ESH 2013 [12, 13], when SBP < 120 mm Hg and DBP < 80 mm Hg, with normal BP when SBP was 120–129 mm Hg and/or DBP 80–84 mm Hg, and high normal pressure when SBP was 130–139 mm Hg and/or DBP 85–89 mm Hg. First degree hypertension was diagnosed when SBP was 140–159 mm Hg and/or 90–99 mm Hg, second degree when SBP was 160–179 mm Hg and/or DBP 100–109 mm Hg, third degree when SBP was ≥ 180 mm Hg and/or DBP ≥ 110 mm Hg.
Statistical analysis
All data obtained during the study were recorded in individual questionnaires. Then they were transferred to the database created in Excel Office 2013. Parameters such as pressure values were described using the arithmetic mean and standard deviation. Crude prevalence of hypertension, awareness, frequency of treatment, and BP control (as defined above) were described as percentages, with the 95% confidence interval (95% CI), for the following age ranges: 19–49, 50–59, 60–69, 70–79 and above 80. Age-standardized prevalence rates were calculated with the direct method using weights assessed for the population of Poland at the end of 2013 [11]. In assessment of compatibility of the distribution of the WOBASZ II population and CSO population (population of Poland by sex and age as of December 31, 2013, according to CSO data), the Wilcoxon signed rank and sign test were compared (p = 0.766 and p = 0.902 respectively). Obtained results are a proof of good matching of the WOBASZ group to the standard CSO population.
The compatibility with a normal distribution was examined using the Lilliefors test. Parametric tests were used for parameters consistent with a normal distribution; otherwise non-parametric tests were used. The t-test for unmatched pairs or Mann-Whitney test was used to compare mean values between the tests and between the groups of men and women. Frequencies of analyzed features were compared using the χ2 test. To compare data from the WOBASZ II study with those from the first edition WOBASZ study, which included adults aged 20 to 74 years, we used restricted data from the WOBASZ II study for people aged 20 to 74 years. The rate ratio (RR) with 95% CI was calculated by dividing the standardized frequency of the above-listed parameter in order to evaluate the changes in the prevalence of optimal, normal, high-normal pressure, grade I, II and III hypertension, prevalence of hypertension, awareness, treatment and control of hypertension between WOBASZ and WOBASZ II studies. An RR value lower than 1.0 indicated a decreased, and above 1.0 an increased prevalence.
Spearman correlation was used to assess the relationship between prevalence of hypertension and participation rate in 16 voivodships. Statistical hypotheses were verified at a significance level of p < 0.05. The calculations were performed using the statistical package Statistica PL (data analysis software system) StatSoft, Inc. (2016) version 12.
Results
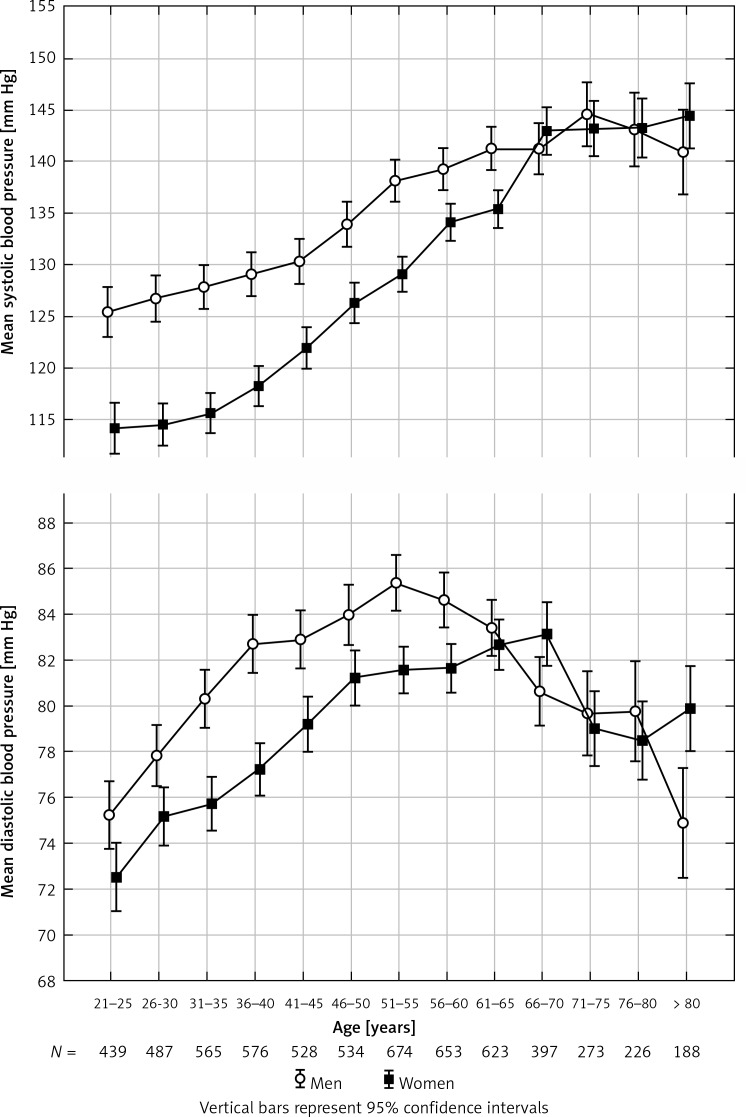
Three pressure measurements in accordance with the established protocol were performed in 98.35% of the patients. In 99.72%, the pressure measurements were conducted in a sitting position. In 33.3% of cases the arm circumference was equal to or greater than 32 cm, and pressure measurement was made using the cuff bigger (size L: 33–45 cm) than the standard one (size M: 22–32 cm), and in 0.8% of the patients the arm circumference was below 22 cm. Blood pressure distribution demonstrated an increase in SBP with an age up to about 75 years in both men and women. Then a further increase in SBP is observed in women over 75 years of age, and its decrease in men over 75 years of age. Distribution of DBP was slightly different – its growth, plateau and decrease with age were noted in men, while the situation in women was similar, with one difference – an increase in DBP was observed from about 75 years of age. Mean SBP values for women were significantly lower than for men in all analyzed 5-year age ranges up to 65 years of age. Similarly, average values of DBP for women were significantly lower than for men in all analyzed 5-year age ranges up to 60 years of age (Figure 1).
Figure 1.
Mean systolic and diastolic blood pressure by age group in WOBASZ II study
Optimal pressure was observed significantly more frequently in women than in men in the whole examined population (34.2% vs. 17.6%; p < 0.00001). High normal pressure and first degree hypertension were observed significantly more often in men than in women in the whole examined group (respectively 26.0% vs. 17.5%; p = 0.0001 and 22.3% vs. 15.9%; p < 0.0001). No significant differences were demonstrated in the prevalence of normal, second and third degree hypertension between men and women. Percentage distributions of optimal, normal and high normal SBP and DBP, as well as first, second and third degree hypertension, are presented in Table I.
Table I.
Crude and age-standardized prevalence of optimal blood pressure, normal and high normal blood pressure in Polish population aged 19–99
| Parameter | Age [years] | P-value* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 19–49 (n = 3114) | 50–59 (n = 1314) | 60–69 (n = 1105) | 70–79 (n = 507) | ≥ 80 (n = 223) | 19–99 | ||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | Age standarization | 95% CI | ||
| Optimal blood pressure: | < 0.0001 | ||||||||||||
| Total | 37.0 | 34.2–39.8 | 18.9 | 14.1–23.8 | 13.3 | 7.8–18.8 | 11.8 | 3.7–20.0 | 10.3 | 0.0–22.7 | 27.1 | 25.8–28.4 | |
| Men | 21.8 | 17.2–26.4 | 11.5 | 3.7–19.3 | 11.2 | 2.9–19.4 | 11.7 | 0.0–24.3 | 14.6 | 0.0–34.6 | 17.6 | 16.0–19.2 | |
| Women | 50.1 | 46.7–53.5 | 24.6 | 18.3–30.8 | 15.1 | 7.7–22.4 | 11.9 | 1.2–22.7 | 7.8 | 0.0–23.7 | 34.2 | 32.2–36.2 | |
| Normal blood pressure: | 0.6266 | ||||||||||||
| Total | 26.3 | 23.2–29.3 | 21.6 | 16.8–26.4 | 17.8 | 12.5–23.2 | 12.6 | 4.5–20.8 | 22.4 | 10.9–34.0 | 23.0 | 21.8–24.2 | |
| Men | 28.0 | 23.6–32.5 | 19.1 | 11.7–26.5 | 17.8 | 9.8–25.7 | 10.3 | 0.00–23.0 | 20.7 | 1.5–40.0 | 23.6 | 21.8–25.5 | |
| Women | 24.8 | 20.5–29.0 | 23.5 | 17.2–29.8 | 17.9 | 10.7–25.1 | 14.3 | 3.7–24.9 | 23.4 | 9.0–37.9 | 22.5 | 20.8–24.1 | |
| High normal blood pressure: | < 0.0001 | ||||||||||||
| Total | 18.4 | 15.2–21.6 | 19.3 | 14.5–24.2 | 19.4 | 14.1–24.7 | 19.5 | 11.7–27.3 | 15.2 | 3.2–27.3 | 18.6 | 17.5–19.7 | |
| Men | 25.0 | 20.5–29.6 | 20.2 | 12.8–27.5 | 17.2 | 9.2–25.1 | 19.6 | 7.6–31.6 | 12.2 | 0.0–32.5 | 22.3 | 20.5–24.1 | |
| Women | 12.7 | 18.7 | 21.2 | 19.5 | 17.0 | 15.9 | 14.6–17.2 | ||||||
| Grade I hypertension: | 0.0002 | ||||||||||||
| Total | 14.3 | 11.0–17.6 | 27.2 | 22.6–31.9 | 31.7 | 26.8–36.5 | 34.1 | 27.1–41.2 | 26 | 14.2–36.9 | 21.2 | 20.1–22.3 | |
| Men | 19.6 | 14.9–24.3 | 35.2 | 28.6–41.9 | 34 | 27.2–41.4 | 38.8 | 28.3–49.3 | 29 | 11.1–47.5 | 26.0 | 24.1–27.9 | |
| Women | 9.6 | 5.0–14.3 | 21.2 | 14.9–27.6 | 29 | 22.8–36.2 | 30.7 | 21.2–40.2 | 23 | 9.0–37.9 | 17.5 | 16.1–18.9 | |
| Grade II hypertension: | 0.7634 | ||||||||||||
| Total | 3.6 | 0.0–7.1 | 9.7 | 4.6–14.9 | 14.1 | 8.7–19.6 | 15.8 | 7.8–23.8 | 21 | 8.9–32.3 | 8.0 | 7.3–8.7 | |
| Men | 4.8 | 0.0–9.9 | 10.6 | 2.8–18.4 | 16 | 7.5–23.6 | 13.1 | 0.6–25.6 | 17 | 0.0–36.8 | 8.3 | 7.2–9.3 | |
| Women | 2.5 | 0.0–7.3 | 9.1 | 2.2–15.9 | 13 | 5.5–20.4 | 17.7 | 7.4–28.1 | 23 | 8.2–37.2 | 7.9 | 6.9–8.9 | |
| Grade III hypertension: | 0.7954 | ||||||||||||
| Total | 0.5 | 0.0–4.1 | 3.1 | 0.0–8.4 | 3.7 | 0.0–9.5 | 6.1 | 0.0–14.5 | 5.8 | 0.0–18.5 | 2.1 | 1.8–2.5 | |
| Men | 0.7 | 0.0–5.9 | 3.4 | 0.0–11.5 | 4.0 | 0.0–12.6 | 6.5 | 0.0–19.5 | 6.1 | 0.0–27.1 | 2.2 | 1.7–2.7 | |
| Women | 0.4 | 0.0–5.2 | 2.9 | 0.0–10.0 | 3.5 | 0.0–11.3 | 5.8 | 0.0–16.9 | 5.7 | 0.0–21.7 | 2.1 | 1.6–2.6 | |
Men vs. women.
After age standardization, the prevalence of hypertension was 42.7% in the entire population of the WOBASZ study, and was highest in the age group 70–79. Having in mind the entire analyzed age range, hypertension was significantly more often noted in men than in women (46.2% vs. 40.4%; p < 0.00001). The greatest awareness of the disease was observed in patients after 50 years of age. This was significantly higher in women than in men in all age groups (63.2% vs. 55.3%; p = 0.00005). Pharmacological therapy was the most commonly implemented in older age – after 60 years of age. In the entire population of the WOBASZ II study, women were treated significantly more often than men (52.1% vs. 40.2%; p < 0.00001). Good BP control was obtained in 23% in the whole examined group, and in 51.9% with respect to treated patients. Pressure normalization was achieved in a higher percentage in women than in men (27.3% vs. 19.0%; p = 0.0091). The worst pressure control was observed in men and women aged 19–49. The prevalence, awareness, and percentage of treated patients, including those treated effectively, are presented in Table II.
Table II.
Crude and age-standardized prevalence of hypertension, awareness, treatment and control in WOBASZ II population aged 19–99
| Parameter | Age [years] | P-value* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 19–49 (n = 3114) | 50–59 (n = 1314) | 60–69 (n = 1105) | 70–79 (n = 507) | ≥ 80 (n = 223) | 19–99 | ||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | Age standardized | 95% CI | ||
| Prevalence: | 0.002 | ||||||||||||
| Total | 22.1 | 18.9–25.2 | 56.8 | 53.2–60.3 | 71.5 | 68.3–74.6 | 80.3 | 76.4–84.1 | 78.0 | 71.9–84.2 | 42.7 | 41.1–44.3 | |
| Men | 29.6 | 25.2–34.0 | 64.1 | 59.1–69.0 | 72.3 | 67.6–76.9 | 78.0 | 71.8–84.3 | 73.2 | 62.0–84.4 | 46.2 | 43.7–48.7 | |
| Women | 15.6 | 11.2–20.1 | 51.3 | 46.3–56.3 | 70.9 | 66.6–75.2 | 81.9 | 77.0–86.8 | 80.9 | 73.6–88.1 | 40.4 | 38.2–42.6 | |
| Awareness: | 0.0425 | ||||||||||||
| Total | 45.8 | 40.2–51.4 | 70.5 | 66.6–74.4 | 77.5 | 74.2–80.8 | 80.8 | 76.6–85.1 | 82.2 | 75.9–88.5 | 59.3 | 56.0–62.6 | |
| Men | 45.3 | 38.1–52.4 | 67.1 | 61.2–73.0 | 71.0 | 65.4–76.5 | 71.3 | 63.1–79.4 | 71.7 | 58.2–85.1 | 55.3 | 50.9–59.7 | |
| Women | 46.6 | 37.6–55.6 | 73.7 | 68.6–78.8 | 82.9 | 79.0–86.9 | 87.5 | 83.0–92.0 | 87.7 | 81.3–94.2 | 63.2 | 58.1–68.2 | |
| Treatment: | < 0.0001 | ||||||||||||
| Total | 30.2 | 23.8–36.5 | 58.2 | 53.5–62.8 | 67.0 | 63.0–71.0 | 73.2 | 68.2–78.2 | 76.4 | 69.2–83.6 | 46.1 | 43.3–48.9 | |
| Men | 28.6 | 20.4–36.7 | 53.6 | 46.6–60.6 | 57.2 | 50.4–63.9 | 61.1 | 51.6–70.5 | 63.3 | 48.0–78.7 | 40.2 | 36.6–43.8 | |
| Women | 32.8 | 22.7–42.9 | 62.5 | 56.4–68.6 | 75.2 | 70.5–79.9 | 81.7 | 76.2–87.1 | 83.3 | 75.8–90.8 | 52.1 | 47.7–56.5 | |
| Controlled: | 0.133 | ||||||||||||
| Total | 17.0 | 10.0–23.9 | 29.4 | 23.3–35.4 | 30.8 | 25.0–36.6 | 30.2 | 22.1–38.3 | 33 | 21.2–45.5 | 23.0 | 21.0–25.0 | |
| Men | 15.0 | 6.1–23.9 | 23.2 | 14.2–32.3 | 25 | 16.5–34.3 | 28.3 | 6.9–49.8 | 28 | 6.9–49.8 | 19.0 | 16.5–21.6 | |
| Women | 20.2 | 9.1–31.2 | 35.2 | 27.1–43.2 | 35 | 27.7–42.9 | 33.8 | 23.5–44.0 | 36 | 21.3–50.7 | 27.3 | 24.0–30.6 | |
Men vs. women.
Among people included in WOBASZ and WOBASZ II studies, mean SBP decreased (mean ± standard deviation) from 137.6 ±18.9 mm Hg to 132.7 ±17.7 mm Hg in men (p < 0.00001), and from 129.7 ±22.1 mm Hg to 125.0 ±18.8 mm Hg in women (p < 0.00001), while mean DBP decreased from 83.9 ±11.8 mm Hg to 81.3 ±10.6 mm Hg and 81.3 ±12.0 mm Hg to 78.7 ±10.6 mm Hg, respectively (p < 0.00001).
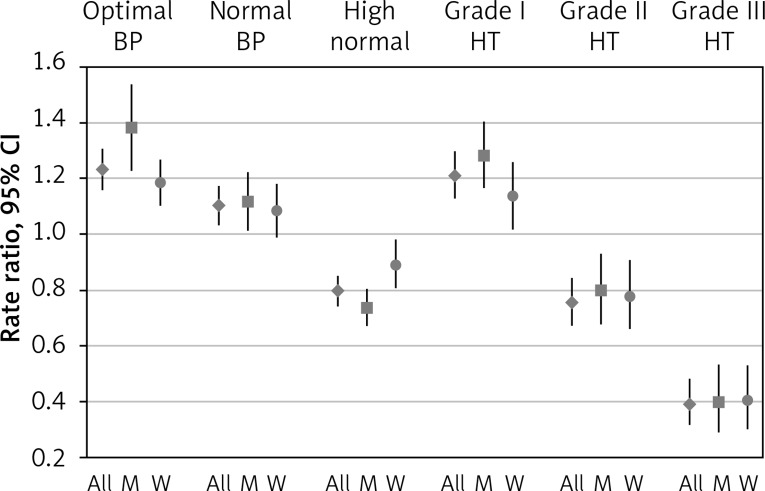
Changes in the prevalence of BP classes, i.e. optimal, normal, high normal BP, and grades I–III hypertension, in a subsample age restricted to 20–74 years are presented as rate ratios in Figure 2.
Figure 2.
Changes in prevalence of BP classes, i.e. optimal, normal, high normal BP, grade I–III hypertension in a subsample age restricted to 20–74 years in WOBASZ studies
All – all population, M – men, W – women.
During the last decade, both in men and in women, there was a significantly increased percentage of persons with optimal and normal BP and first degree hypertension and a decreased percentage of persons with high normal BP and second and third degree hypertension.
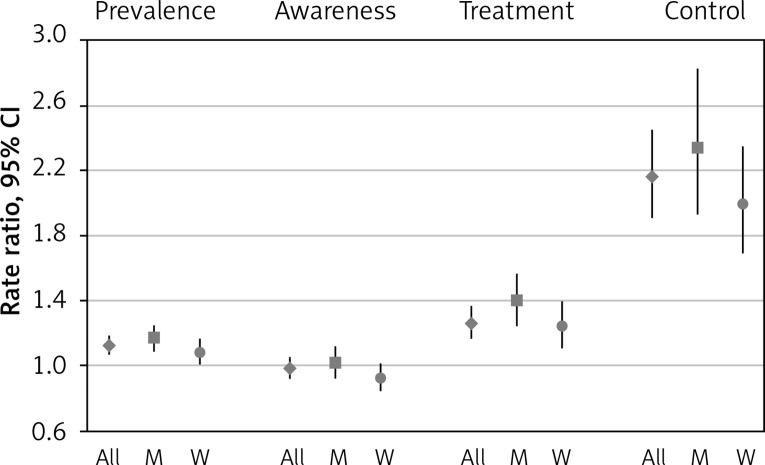
Changes in the prevalence of hypertension, awareness, treatment and control of BP in a subsample age restricted to 20–74 years are presented as rate ratios in Figure 3.
Figure 3.
Changes in the prevalence of hypertension, awareness, treatment and control of BP in a subsample age restricted to 20–74 years in WOBASZ studies
All – all population, M – men, W – women.
After standardization for age and sex, the prevalence of hypertension among people included in WOBASZ and WOBASZ II studies increased from 34.7% to 39% (RR = 1.12; 95% CI: 1.07–1.8); in men from 38.1% to 44.3% (RR 1.16; 95%CI: 1.09–1.25), in women from 32.3% to 35% (RR = 1.08; 95% CI: 1.01–1.16). Hypertension awareness decreased from 55% to 54.2% (RR = 0.98; 95% CI: 0.92–1.05); in men it increased from 51.6% to 52.3% (RR = 1.01; 95% CI: 0.92–1.11) and in women decreased from 59.2% to 54.7% (RR = 0.92; 95% CI: 0.84–1.01). Comparing WOBASZ studies, an improvement was observed – the number of treated patients increased from 32% to 40.5% (RR = 1.26; 95% CI: 1.17–1.36); in men it increased from 26.9% to 37.5% (RR = 1.39; 95% CI: 1.24–1.57) and in women from 38.2% to 42.9% (RR = 1.24; 95% CI: 1.11–1.40). Also BP control improved twofold – it increased from 9.6% to 20.7% (RR = 2.16; 95% CI: 1.91–2.45); in men it increased from 7.6% to 17.5% (RR = 2.34; 95% CI: 1.93–2.82) and in women from 12.0% to 23.8% (RR = 1.99; 95% CI: 1.69–2.35).
Discussion
The average values of SBP and DBP (analyzed in the whole population – in patients with and without diagnosed hypertension) over the last 10 years in Poland decreased during the decade between 2003/2005 (WOBASZ) [15] and 2013/2014 (WOBASZ II). We relate this to an increase in the number of patients with implemented effective antihypertensive therapy, and an increase in the number of patients with improved BP control. Less likely, the shift to a more favorable distribution of BP could be related to life style modification. Other findings of the WOBASZ II study suggest that both diet and physical activity changed to less favorable patterns, which was reflected in unfavorable changes in blood lipids and prevalence of obesity [16–19]. These data are part of a global trend in which a decrease in both SBP and DBP was observed in recent years. Between 1980 and 2008, age-standardized average SBP was reduced from 130.5 mm Hg to 128.1 mm Hg in men, which gives a decrease of 0.8 mm Hg per decade, and from 127.2 mm Hg to 124.4 mm Hg in women, which means a decrease of about 1.0 mm Hg per decade [20].
Only 27.1% of the patients aged 19–99 years had optimal BP. This percentage was significantly higher for women than for men (34.2% vs. 17.6%; p < 0.00001). For comparison, in the English population aged 20–79 years the corresponding figures were 34.2%, for the US population 50.3%, and for the Canadian population 66.1% [21].
In the present study, repeated BP measurement (three times) took place in one visit. According to current recommendations of ESH/ESC 2013 [13] and PTNT 2015 [12], the diagnosis of hypertension is based on at least two pressure measurements during two separate visits. The implementation of these recommendations to epidemiological studies is difficult. Taking the measurements at only one visit leads to higher average values of BP and to an overestimation of hypertension prevalence in the examined population, and an underestimation of awareness of this disease and effectiveness of treatment. The differences in methodology concerning hypertension diagnosis cause a problem in interpretation and comparison of the epidemiological situation in different countries. A meta-analysis of Kearney et al. [8], evaluating hypertension prevalence in 40 countries, included studies with different numbers of visits and BP measurements – both based on one visit (e.g. Spanish, English, German, Greek, Italian, studies) and on two visits (American, Canadian studies). It was the basis of hypertension prevalence estimation in the world in 2000 at a level of about 26.4% (95% CI: 26.0–26.8%). The study conducted in 2001–2003 by Figueiredo on the Portuguese population aged above 45 demonstrated the prevalence of hypertension at the level of 63.4%, 60.2%, 56.3% (p < 0.001), for the measurements based on the first visit, the second visit, and the average of the first and second visit, respectively. According to the authors of this study, pressure measurement at only one visit resulted in an overestimation of hypertension prevalence of 12.6% [22].
Prevalence of hypertension in the HYDY study conducted in 2007 on the Yemeni population aged 15–69, estimated based on measurements from a single visit, was 17.3% and was 35% higher than that calculated on the basis of the measurements from two different visits, which was 11.3% [23]. In the Polish NATPOL PLUS study from 2002, hypertension diagnosis was based on the measurements performed in the homes of the respondents during three separate visits. The prevalence of hypertension according to the number of visits was 36.4%, 31.3% and 29.4% for 1, 2 and 3 visits, respectively [6, 24].
Taking into account the results of the Portuguese study, the closest to Polish socio-economic and epidemiological conditions, as well as the results of the NATPOL PLUS study, we recognize that our results may be higher by about 15%. Attention should be paid to the high prevalence of hypertension in the WOBASZ II population – up 42.7%, significantly different from that observed in other developed countries (Table III). Similar results were observed in Bosnia and Herzegovina as well as in Greece.
Table III.
Hypertension prevalence in selected countries
| Study | Country | Year | Population [years] | No. of measurements | No. of visits | Prevalence of hypertension (%) | ||
|---|---|---|---|---|---|---|---|---|
| Overall | Men | Women | ||||||
| NHANES | USA | 2007–2010 | 20–79 | 3 (mean 2 and 3) | 1 | 29.1 | 29.4 | 28.8 |
| The Canadian Health Measures Survey | Canada | 2007–2009 | 20–79 | 6 (mean 2–6) | 2 | 19.5 | 19.7 | 19.3 |
| Health Survey for England | England | 2011 | ≥ 16 | 3 (mean 2 and 3) | 1 | 30 | 32 | 28 |
| PatenT 2 | Turkey | 2012 | > 18 | 3 | 1 | 30.3 | 28.4 | 32.3 |
| DEGS1 | Germany | 2008–2011 | 18–79 | 3 (mean 2 and 3) | 1 | 32 | 33.4 | 30 |
| Pilav et al. | Bosnia and Herzegovina | 2012 | > 18 | 3 (mean 2 and 3) | 1 | 42 | 43.9 | 37.5 |
| EPIC | Greece | 2004 | 20–86 | 2 | 1 | 44.4 | 45.2 | 43.8 |
Epidemiological data from around the world are divergent – depending on the region of residence, hypertension occurs with varying frequency in men and women (Table III).
According to the WHO report of 2015 [25], higher prevalence of hypertension in men than in women was found in countries with a socio-economic profile (i.e. Central and Eastern Europe countries) similar to the Polish population, e.g.: 35.2% and 24.3% in Lithuania, 34.6% and 23.1% in Hungary, 33.2% and 21% in the Czech Republic, for men and women, respectively. The situation is similar in Western Europe; in 2010, in the population aged over 20, hypertension occurred more frequently in women than in men: 23.3% vs. 20.7% in the UK, 20.0% vs. 14.8% in Spain, 22.3% vs. 17.6% in Italy, 25.1% vs. 22.9% in Germany [26]. Women suffer from hypertension more frequently than men in some African countries, e.g. in 32.0% and 27.7% in Lesotho for women and men, respectively [25]. In 2015, global age-standardized prevalence of raised blood pressure was 24.1 in men and 20.1% in women [27].
The awareness, percentage of treated patients and blood pressure control have improved over the last decade, and in the WOBASZ II study in the whole population aged 19–99 years they were 59.3%, 46.1% and 23%, respectively. As a result, we approached the best countries in this range. The awareness of hypertension in the NHANES study in 2009–2012 in patients above 20 years of age was noted in about 82.7% of patients, and 76.5% of them were treated, including 54.1% who achieved good BP control [9]. The absolute leader in the care related to hypertension is Canada, where the greatest awareness of hypertension was reported (83.4%), the highest percentage of patients had antihypertensive treatment implemented (79.9%), and good BP control was achieved in the largest number of patients – up to 65.8% [21]. Such good results were not achieved in countries which, like Poland, reported a high prevalence of hypertension. In 2012, awareness of the disease in the population of Bosnia and Herzegovina was reported by 48.6% of respondents, 40.3% of men and 57.2% women. In this study, 35.5% of men and 54.2% of women were treated, but good pressure control was observed in only 9% of men and 22.2% of women [28].
It is not possible to compare easily Polish epidemiological studies, i.e. the NATPOL PLUS study of 2002 [6, 24], the WOBASZ study of 2005 [6, 15, 24], NATPOL 2011 [6, 24] and the WOBASZ II study. However, all these studies were carried out on a representative group of Polish citizens, but they included different age ranges of the examined population, 18–94, 20–74, 19–79 and 19–99, respectively. Therefore, in presenting the results of the WOBASZ II study, it was necessary to make additional calculations for the age 20–74, so that it was possible to compare both WOBASZ studies. Another difference in NATPOL and WOBASZ studies was the number of visits – the NATPOL PLUS study involved three visits (the results were described for 2 visits), NATPOL 2011 involved two visits, and the WOBASZ study involved one visit. The prevalence of hypertension has increased in Poland since 2002. In the NATPOL study, it increased from 30% to 32% between 2002 and 2011 [24]. This increase was higher in WOBASZ studies – from 34.7% to 39.0% in the whole population. An increase in the number of patients with hypertension between 2010 and 2025 is predicted in many Western European countries, and is expected to reach 9% in Germany, 17% in France and Italy, 18% in Britain and 22% in Spain [26].
The increase in hypertension diagnosis is observed both in NATPOL and WOBASZ studies. Awareness of the disease in the NATPOL study increased within a decade from 66% to 72% [24]. A different trend was observed in WOBASZ and WOBASZ II studies – awareness of the disease showed an insignificant decrease from 55.2% to 54.2%. The care of patients with hypertension in Poland shows continuous improvement. The number of patients with implemented treatment is increasing, and its control is improving. The effectiveness of hypertension treatment in NATPOL PLUS and NATPOL 2011 studies measured by the percentage of patients with SBP < 140 mm Hg and DBP < 90 mm Hg among all patients with hypertension increased over 10 years from 12% to 26% [24]. This could be the effect of growing attention to hypertension over the last decades both among professionals and the general public. The important signs were introduction of hypertensiology specialization in 2005 (now, there are 304 professionals in this field in Poland) [29] and very intensive training activities of the Polish Society of Hypertension, which in 2008 and 2011 issued guidelines for the diagnosis and treatment of hypertension, and organized a number of seminars and workshops addressed to general practitioners.
An important role was played by national projects that were introduced in Poland in 2003 as part of the National Program for Prevention and Treatment of Cardiovascular Diseases POLKARD (the Polish 400 Cities Project: screening and educational program for citizens of 400 small cities, Polkard-Media: education of general population using TV and radio, SMS: educational multimedia program for children in schools) [24].
Also public current expenditures on health care have increased in recent years. In 2004, they amounted to around 37 billion PLN (about $9.5 billion, $1 = 4 PLN), which accounted for 4.02% of GDP (gross domestic product), and in 2012 was 70.7 billion PLN (about $17.5 billion), which represented 4.43% of GDP [30].
One strength of the WOBASZ II study is the large group of examined people, n = 6170. After the WOBASZ study of 2005 (n = 14 769), it is the largest Polish epidemiological study concerning hypertension. For example, another study – the last edition of NATPOL of 2011 – involved only 2404 people. The main strength of the study would be that the examined group was a stratified random sample, which was representative for the Polish population aged over 19 years.
On the other hand, the study had a low participation rate, so selection bias towards overrepresentation of healthy people could be expected. Further, participation in WOBASZ II was lower than 10 years ago (45.5% vs. 70.5%; frequency among women was 10% higher than in men; it was also lower than in the NATPOL 2011 study, where it was 66.5%) [24]. It is similar to the rate observed in the 12 European countries participating in the EHES study (European Health Examination Survey Pilot Project) in 2009–2012, which ranged from 16% to 57% in men, and from 31% to 74% in women [31]. However, there was no significant correlation between the response rate in 16 voivodships and the prevalence of hypertension (r = 0.17; p = 0.516), awareness (r = 0.31; p = 0.2351), treatment (r = 0.15; p = 0.569), control (r = 0.27; p = 0.3108, optimal (r = 0.2; p = 0.4668), normal (r = 0.33; p = 0.207), and high normal BP (r = –0.12, p = 0.6485).
Another weakness of this study was that BP measurements were made only at one visit. This could have resulted in an overestimation of hypertension prevalence in Poland and led to underestimation of its control.
In conclusion, the prevalence of hypertension in Poland is high, and increased by about 12% within the decade between 2003/2005 and 2013/2014. Although the proportion of treated patients and in particular the proportion of patients reaching the treatment target increased over twofold, it is still lower than the average in Western Europe, USA or Canada. Efforts to improve the diagnosis and effective treatment of hypertension in Poland should be intensified, both in primary care and specialized treatment, especially in young people.
Acknowledgments
A complete list of members of the WOBASZ II Trial is available at: Kardiologia Polska 2016; 74, 7: 681-690.
On behalf of the Steering Committee of the WOBASZ Study, we address words of heartfelt thanks for the participation in the study to all of our co-workers from the research teams in six academic centers, nurses, doctors and analysts from local research centers in 16 provinces.
Special thanks to Professor Jerzy Głuszek for valuable comments in the formation of the initial version of the manuscript and Stanisław Paradowski for help with statistical calculations.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–83. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study. 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarian D, Roger VL, et al. Executive summary: heart disease and stroke statistics – 2014 update: a report from the American Heart Association. Circulation. 2014;129:399–410. doi: 10.1161/01.cir.0000442015.53336.12. [DOI] [PubMed] [Google Scholar]
- 4.MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease. Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–74. doi: 10.1016/0140-6736(90)90878-9. [DOI] [PubMed] [Google Scholar]
- 5.Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the U.S. by improvements in use of clinical preventive services. Am J Prev Med. 2010;38:600–9. doi: 10.1016/j.amepre.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 6.Kopcia G, Jankowski P, Pająk A, Drygas W. Epidemiology and prevention of cardiovascular diseases. Krakow: Medycyna Praktyczna; 2015. [Google Scholar]
- 7.Central Statistical Office . Demographic Yearbook of Poland. Warsaw: 2016. [Google Scholar]
- 8.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 9.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics – 2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 10.Rywik S, Kupść W, Piotrowski W, et al. Multicenter national Polish population health status tests-WOBASZ project. Establishment of methods and logistics. J Kardiol Pol. 2005;63(6 Suppl. 4):S605–13. [PubMed] [Google Scholar]
- 11.Drygas W, Niklas AA, Piwońska A, et al. Multi-centre National Population Health Examination Survey (WOBASZ II study): assumptions, methods, and implementation. Kardiol Pol. 2016;74:681–90. doi: 10.5603/KP.a2015.0235. [DOI] [PubMed] [Google Scholar]
- 12.Tykarski A, Narkiewicz K, Gaciong Z, et al. 2015 guidelines for the management of hypertension. Recommendations of the Polish Society of Hypertension – short version. Kardiol Pol. 2015;73:676–700. doi: 10.5603/KP.2015.0157. [DOI] [PubMed] [Google Scholar]
- 13.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2013;31:1281–357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 14.Gee ME, Campbell N, Sarrafzadegan N, et al. Standards for the uniform reporting of hypertension in adults using population survey data: recommendations from the World Hypertension League Expert Committee. J Clin Hypertens (Greenwich) 2014;16:773–81. doi: 10.1111/jch.12387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tykarski A, Posadzy-Małaczyńska A, Wyrzykowski B, et al. Prevalence of hypertension and effectiveness of its treatment in adult residents of our country. Results of the WOBASZ program. Kardiol Pol. 2005;63(6 Suppl 4):S614–9. [PubMed] [Google Scholar]
- 16.Waśkiewicz A, Szcześniewska D, Szostak-Węgierek D, et al. Are dietary habits of the Polish population consistent with the recommendations for prevention of cardiovascular disease? – WOBASZ II Project. Kardiol Pol. 2016;74:969–77. doi: 10.5603/KP.a2016.0003. [DOI] [PubMed] [Google Scholar]
- 17.Kwaśniewska M, Pikala M, Bielecki W, et al. Ten-year changes in the prevalence and socio-demographic determinants of physical activity among Polish adults aged 20 to 74 years. Results of the National Multicenter Health Surveys WOBASZ (2003-2005) and WOBASZ II (2013-2014) PLoS One. 2016;11:e0156766. doi: 10.1371/journal.pone.0156766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pająk A, Szafraniec K, Polak M, et al. Changes in the prevalence, treatment, and control of hypercholesterolemia and other dyslipidemias over 10 years in Poland: the WOBASZ study. Pol Arch Med Wewn. 2016;126:642–52. doi: 10.20452/pamw.3464. [DOI] [PubMed] [Google Scholar]
- 19.Stepaniak U, Micek A, Waśkiewicz A, et al. Prevalence of general and abdominal obesity and overweight among adults in Poland. Results of WOBASZ II study (2013–2014) and comparison with WOBASZ study (2003–2005) Pol Arch Med Wewn. 2016;126:662–671. doi: 10.20452/pamw.3499. [DOI] [PubMed] [Google Scholar]
- 20.Danaei G, Finucane MM, Lin JK, et al. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Pressure). National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5,4 million participants. Lancet. 2011;377:568–77. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 21.Joffres M, Falaschetti E, Gillespie C, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013;3:e003423. doi: 10.1136/bmjopen-2013-003423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Figueiredo D, Azevedo A, Pereira M, de Barros H. Definition of hypertension: the impact of number of visits for blood pressure measurement. Rev Port Cardiol. 2009;28:775–83. [PubMed] [Google Scholar]
- 23.Modesti PA, Rapi S, Bamoshmoosh M, et al. Impact of one or two visits strategy on hypertension burden estimation in HYDY, a population-based cross-sectional study: implications for healthcare resource allocation decision making. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-001062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Więcek A, Januszewicz A, Szczepańska-Sadowska E, Prejbisz A. Hypertensiology. Krakow: Medycyna Praktyczna; 2011. [Google Scholar]
- 25.World health statistics 2015 WHO Library Cataloguing-in-Publication Data. 2015. Available: http://apps.who.int/iris/bitstream/10665/170250/1/9789240694439_eng.pdf?ua=1&ua=1 Accessed 15 July 2017.
- 26.Eichmann F, Potthoff P, Schmidt M. Burden of hypertension in selected EU countries: 2010-2025. Value Health. 2012;15:A383. [Google Scholar]
- 27.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pilav A, Doder V, Branković S. Awareness, treatment, and control of hypertension among adult population in the Federation of Bosnia and Herzegovina over the past decade. J Public Health Res. 2014;3:323. doi: 10.4081/jphr.2014.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centralny Rejestr lekarzy Naczelnej Izby Lekarskiej 2015. Available: http://nil.org.pl/__data/assets/pdf_file/0017/104138/Zestawienie-nr-04.pdf. Accessed 15 July 2017.
- 30.Health and health care in 2014 . Central Statistical Office of Poland. 2014. Available: http://stat.gov.pl/obszary-tematyczne/zdrowie/zdrowie/narodowy-rachunek-zdrowia-za-2012-rok,4,5.html. Accessed 15 July 2017. [Google Scholar]
- 31.Tolonen H, Ahonen S, Jentoft S, Kuulasmaa K, Heldal J, European Health Examination Pilot Project Differences in participation rates and lessons learned about recruitment of participants – the European Health Examination Survey Pilot Project. Scand J Public Health. 2015;43:212–9. doi: 10.1177/1403494814565692. [DOI] [PubMed] [Google Scholar]