Case
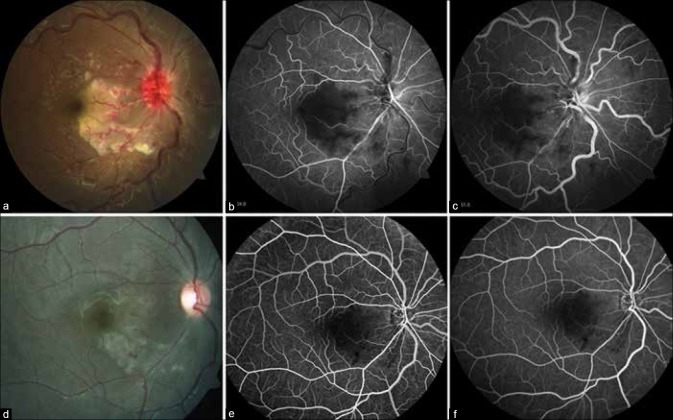
A 15-year-old female presented with diminution of vision in the right eye following high-grade fever for 18 days which was associated with skin rashes, severe myalgia, and arthralgia [Fig. 1]. She was extensively investigated for the cause of her febrile illness, which included a negative serology for dengue and chikungunya. Best-corrected visual acuity (BCVA) was 20/200 in the right eye and 20/20 in the left eye. Slit-lamp examination of the right eye revealed a quiet anterior chamber and anterior vitreous. Fundus examination of the right eye showed a circumscribed area of retinal whitening, abutting the fovea nasally and inferonasally with optic disc edema, marked venous tortuosity, few intraretinal hemorrhages, and cotton wool spots [Fig. 2a]. Fluorescein angiography showed early and late hypofluorescence due to hypoperfusion of retinal arterioles and capillary non-perfusion corresponding to the area of retinal whitening along with late disc staining [Fig. 2b and c]. Extensive laboratory workup under the guidance of a multidisciplinary approach revealed positive anti-nuclear antibodies with Hep-2 immunofluorescence, positive anti-double-stranded DNA antibody, and negative anti-B2 glycoprotein 1 antibody. A diagnosis of systemic lupus erythromatosus (SLE) was made by rheumatologist and she was started on oral prednisolone 1 mg/kg/day and hydroxychloroquine 200 mg once a day. At 4 weeks, the BCVA improved to 20/40 in the right eye. The disc edema resolved, and hemorrhages and retinal whitening reduced along with narrowing of the arterioles [Fig. 2d–f].
Figure 1.

(a and b) Hyperpigmented maculopapular rash on the face and palm of the patient
Figure 2.
(a) Color fundus photograph of right eye shows a circumscribed area of retinal whitening abutting fovea with hyperemic and edematous optic disc, marked venous tortuosity along with retinal hemorrhages, and cotton wool spots. Fluorescein angiogram of the right eye showing widespread arteriolar occlusion and capillary non-perfusion persisting in (b) early and (c) late phases. (d) At 3 weeks, disc edema resolved, hemorrhages and retinal whitening reduced along with narrowing of the arterioles, with improved perfusion of the arterioles and capillary plexus (e and f)
Discussion
SLE is an autoimmune, multisystem disease of unknown etiology which may affect the eye in up to a third of patients.[1] Purtscher-like retinopathy (PLR) is relatively rare but has been reported in patients with SLE. PLR is classically characterized by cotton-wool spots, few to moderate number of retinal hemorrhages, optic disc edema, and Purtscher flecken. Purtscher flecken is an area of inner retinal whitening with a clear demarcating line between the affected retina and contiguous normal retinal vessels. Although the majority of the cases have been described in previously diagnosed patients with SLE,[2] there are reports of PLR presenting as initial manifestation of SLE.[3]
Conclusion
It is of paramount importance for the ophthalmologists to be aware of this dreaded sight-threatening condition of SLE. Ocular involvement with multiple cotton wool spots, retinal hemorrhages, and retinal whitening with macular edema following a febrile illness with severe myalgia may lead to a misdiagnosis of viral retinitis, if a thorough systemic examination and laboratory investigations under multidisciplinary approach are not carried out.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Stafford-Brady FJ, Urowitz MB, Gladman DD, Easterbrook M. Lupus retinopathy. Patterns, associations, and prognosis. Arthritis Rheum. 1988;31:1105–10. doi: 10.1002/art.1780310904. [DOI] [PubMed] [Google Scholar]
- 2.Wu C, Dai R, Dong F, Wang Q. Purtscher-like retinopathy in systemic lupus erythematosus. Am J Ophthalmol. 2014;158:1335–41.e1. doi: 10.1016/j.ajo.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Alahmadi RM, Hashim RT, Almogairin SM, Abu AM. Purtscher-like retinopathy as a first presentation of systematic lupus erythematosus. Ann Saudi Med. 2016;36:85–8. doi: 10.5144/0256-4947.2016.85. [DOI] [PMC free article] [PubMed] [Google Scholar]