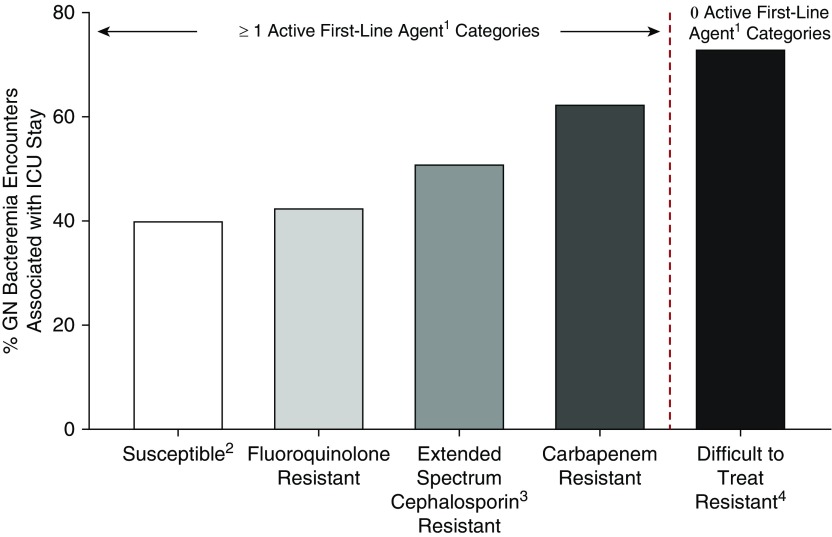
Figure 1.
Proportion of unique inpatient encounters with gram-negative bacteremia associated with an ICU stay across resistance phenotypes (29,474 unique inpatient encounters, 170 U.S. hospitals in Premier Healthcare Database, 2009–2013). The figure depicts the proportion of ICU stays associated with inpatients with bacteremia resulting from select taxa of gram-negative bacteria (Escherichia coli, Klebsiella pneumoniae, Enterobacter spp., Pseudomonas aeruginosa, and Acinetobacter baumannii) across various phenotypes of resistance. The association with ICU stay was greatest for encounters with gram-negative bacteremia displaying difficult-to-treat resistance (no active first-line agent categories) at 73%. Even among isolates with one or more active first-line category, the association with ICU stay increased with increasing spectrum of the antibiotic category to which the isolate is resistant (carbapenems > extended-spectrum cephalosporins > fluoroquinolones). Susceptible: 8,547/21,410; fluoroquinolone resistant: 1,845/4,342; extended spectrum cephalosporin resistant: 1,401/2,756; carbapenem resistant: 328/526; difficult-to-treat resistant: 321/440. 1First-line agents are carbapenems, other β-lactams, and fluoroquinolones. 2Without any of the four resistance phenotypes in the figure. 3Extended-spectrum cephalosporins include third- and fourth-generation cephalosporins (for P. aeruginosa, limited to antipseudomonal cephalosporins). 4For GN bloodstream isolates, “difficult-to-treat resistant” indicates intermediate susceptibility or resistance to all carbapenems, other β-lactams, and fluoroquinolones tested. The other resistance phenotypes shown are defined using U.S. Centers for Disease Control and Prevention 2015 surveillance definitions (17). GN = gram-negative. Data from Table 2 of Reference 4.