Abstract
We used marginal structural models to evaluate associations of social support with antepartum depression in late pregnancy, if everyone had had high social support both before pregnancy and during early pregnancy, compared with having low social support at one of the 2 time points or low social support at both time points. In 2012–2014, pregnant Peruvian women (n = 3,336) were recruited into a prospective cohort study (at a mean gestational age of 9 weeks). A follow-up interview (n = 2,279) was conducted (at 26–28 weeks of gestation). Number of available support providers and satisfaction with social support were measured using Sarason Social Support Questionnaire–6. Depression was measured using the Edinburgh Postnatal Depression Scale. Low number of support providers at both time points was associated with increased risk of depression (odds ratio = 1.62, 95% confidence interval: 1.12, 2.34). The association for low satisfaction at both time points was marginally significant (odds ratio = 1.41, 95% confidence interval: 0.99, 1.99). Depression risk was not significantly higher for women who reported high social support at one of the 2 time points. Our study reinforces the importance of assessing social support before and during pregnancy and underscores the need for future interventions targeted at increasing the number of support providers to prevent antepartum depression.
Keywords: antepartum depression, marginal structural models, prenatal interventions, social support
Depression is common among women of childbearing age (1) and remains one of the most serious mental health problems faced by women (2). The prevalence of antepartum depression ranges from 10% to 41% in low- and middle-income countries (3, 4). Antepartum depression is associated with many adverse obstetrical outcomes and neonatal outcomes (5); it also places women at high risk for postpartum depression (6).
Although the risk factors for antepartum depression are well-documented, few studies have investigated protective factors. Social support, defined as any process whereby social relationships promote health and well-being (7), is hypothesized to act as a buffer against depression in stressful circumstances or major life transition such as pregnancy (8, 9). The relationship between social support and depression is complex (10, 11). On the one hand, greater social support decreases the risk for depression and depression relapse, and improves treatment outcomes, whereas deficits in social support increase the risk of depression and relapse (10–12). On the other hand, depression may cause strains on interpersonal relationships and negatively affect social support (10, 13). Depressed individuals tend to withdraw from social support, perceive the social support more negatively, and underestimate the level of existing support, which may lead them to receive and perceive low social support (10, 14, 15). Besides, such a negative effect of depression on social support can, in turn, undermine the long-term treatment of depression and increase the risk of relapse (11). Previous studies have shown that low social support was a risk factor for depression during pregnancy and after giving birth and have shown potential benefits of interventions targeted at increasing social support (2, 16–18). However, the majority of prior studies on the association of social support with depression have been cross-sectional, and the causal relationship remains unclear (16, 18–21). Limited longitudinal research has been carried out (2, 22–24), and most such studies have measured social support only once. Understanding the impact of social support at different time points may have important implications for the prevention and treatment of antepartum depression (22). No study has yet adequately addressed the methodological challenge of the complex, bidirectional relationship between social support and depression. Furthermore, there is relatively little research concerning how social support affects antepartum depression (16, 23) compared with postpartum depression (2, 21, 22, 25–27).
Using data from a prospective cohort study with repeated measures for social support and depression during pregnancy, we applied marginal structural models (MSMs) to assess the time-varying associations of low social support (prior to pregnancy and in early pregnancy) with antepartum depression in late pregnancy. We chose to use MSMs given that depression at early pregnancy was a confounder of the causal association of social support in early pregnancy on antepartum depression in late pregnancy and was affected by social support prior to pregnancy. By fitting MSMs, such temporal ordering was assumed to disentangle the bidirectional relationship between social support and depression. In addition, MSMs can help inform the design of prenatal interventions for clinical practice (28). We aimed to provide the magnitude of the association of social support at 2 different time points on depression at late pregnancy.
METHODS
Participants
Participants in this study were women who received prenatal care at the Instituto Nacional Materno Perinatal and enrolled in the Pregnancy Outcomes, Maternal and Infant Cohort Study. The Pregnancy Outcomes, Maternal and Infant Cohort is a longitudinal study designed to examine social and behavioral maternal risk factors of pregnancy outcomes in Lima, Peru. Eligible participants were pregnant women who were 18–49 years of age and whose offspring were <16 weeks of gestational age at the first prenatal care visit. Participants were interviewed during the first prenatal care visit (interview 1, mean gestational age of 9 weeks) and a follow-up visit (interview 2) during 26–28 weeks of gestational age. Each participant was interviewed, in a private setting, by trained research personnel using a structured questionnaire. All participants provided written informed consent prior to the interview. The institutional review boards of the Instituto Nacional Materno Perinatal, Lima, Peru, and the Harvard T.H. Chan School of Public Health, Office of Human Research Administration, Boston, Massachusetts, approved all procedures used in this study.
The study population for the present analysis is derived from participants who enrolled in the Pregnancy Outcomes, Maternal and Infant Cohort Study between February 2012 and July 2014. During this period, 3,372 participants agreed to participate and completed the initial structured interview (interview 1), 81% of the eligible women approached. At interview 1, 36 participants were excluded because of missing information concerning social support and depression, leaving 3,336 women. Follow-up in-person interviews (interview 2) of 2,292 participants were conducted. Participants who attended interview 1 but not interview 2 (n = 1,044) were considered to be “censored.” At interview 2, 13 women were excluded due to missing information concerning social support and depression, leaving 2,279 women.
Measures
During the interview 1, participants reported baseline information regarding maternal sociodemographic and lifestyle characteristics, medical and reproductive histories, and experiences of childhood abuse (29) and intimate partner violence (30) before pregnancy. In addition, social support prior (31, 32) to the active pregnancy (any time before pregnancy) and antepartum depression (33) 7 days prior to interview 1 were measured. During the interview 2, social support since becoming pregnant/during early pregnancy and antepartum depression 7 days prior to interview 2 were measured.
Social support consisted of 2 distinct aspects (satisfaction with social support and number of available support providers); it was measured using a Spanish-language version of the 6-item Sarason Social Support Questionnaire–6 (SSQ-6) (31, 32). Participants were asked to indicate how satisfied they were with the overall support received and rate their satisfaction on a Likert scale from 1 (very unsatisfied) to 6 (very satisfied) in the following 6 situations: 1) is dependable when you need help; 2) helps you feel relaxed when you are under pressure; 3) takes care of you regardless of the circumstances; 4) cheers you up when you are feeling down; 5) consoles you when you are upset; and 6) accepts you unconditionally, including both your good and bad points. The Social Support Questionnaire Satisfaction Scale (SSQS) was scored by summing the ratings, ranging from 6 to 36. The Social Support Questionnaire Number Scale (SSQN), the total number of available support providers that participants can count on for help or support in the aforementioned 6 situations, was also calculated. The total SSQN score ranges from 0 to 54. To be compatible with previous studies using the SSQ-6 (32, 34–38), we defined low satisfaction with social support as an SSQS of ≤33 for interview 1 and an SSQS of ≤32 for interview 2 using the median split. The low number of support providers was defined as the SSQN of ≤8 for both interviews 1 and 2. In our population, the SSQ-6 was a reliable measure, with a Cronbach’s α of 0.81.
Depression 7 days prior to each interview was measured using the Spanish-language version of the Edinburgh Postnatal Depression Scale (EPDS). The EPDS is a widely used, 10-item screening scale for antepartum and postpartum depression (33). Women were asked to rate how they felt in the previous 7 days. Individual items are totaled to give an overall score ranging from 0 to 30. Prior validation studies suggest a cutoff score of ≥10 for possible depressive disorder (33, 39). The Spanish-language version of the EPDS has been shown to be a reliable and valid scale for antepartum depression screening among Peruvian pregnant women (4).
Models and estimations
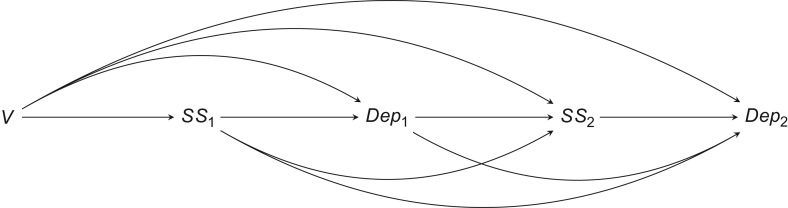
MSMs can be used to estimate the causal association of a time-dependent exposure in the presence of time-dependent covariates that are simultaneously confounders and intermediate variables from observational data (40, 41). We fitted 2 sets of MSMs for the 2 distinct aspects of social support (2, 32): low satisfaction with social support and a low number of available support providers. We used the MSMs to account for the potential confounding and intermediary role of depression in early pregnancy (Figure 1): Social support prior to pregnancy (SS1), measured at interview 1, might be associated with depression at interview 1 (Dep1), which might, in turn, affect both social support since becoming pregnant (SS2) and depression at interview 2 (Dep2) both measured at interview 2.
Figure 1.
Directed acyclic graph for the association of low social support with antepartum depression at interview 2, Pregnancy Outcomes, Maternal and Infant Cohort Study, Peru, 2012–2014. V represented the time-independent baseline covariates (maternal age, education, race/ethnicity, married/living with partner, difficulty in accessing basic foods, planned pregnancy, parity, childhood abuse, and intimate partner violence prior to pregnancy). if women received low social support prior to index pregnancy, otherwise 0; if women received low social support since becoming pregnant, otherwise 0; if women were depressed at interview 1, otherwise 0; and if women were depressed at interview 2, otherwise 0. represented as both confounder and intermediate variable in relation to .
The models that predicted the expected outcome took the form:
where was antepartum depression at interview 2 for a woman that would have resulted under the hypothetical joint interventions to set social support at interview 1 and interview 2, possibly contrary to fact, to SS1 and SS2, respectively. We evaluated associations of social support with antepartum depression, if all had had high social support at both interviews 1 and 2, compared with having low social support at one of the 2 time points or low social support at both time points. V denoted the baseline covariates including maternal age, education, race/ethnicity, marital status, difficulty in accessing basic foods, planned pregnancy, parity, childhood abuse, and intimate partner violence prior to pregnancy.
Inverse probability weights
MSMs can appropriately control for time-varying confounding and loss to follow-up through inverse-probability-of-treatment and inverse-probability-of-censoring weights and give valid estimates (40, 41).
Inverse-probability-of-treatment weights
We used a stabilized version of inverse-probability-of-treatment weights:
given the smaller variance (40, 41), where V represented the aforementioned time-independent baseline covariates, and L1 included both depression at interview 1 and baseline covariates V. Further details on the distribution of both stabilized and unstabilized weights are available in the Web Table 1 (available at https://academic.oup.com/aje).
Inverse-probability-of-censoring weights
To adjust for right censoring at interview 2 due to loss to follow-up, we used a similar procedure to estimate the stabilized inverse-probability-of-censoring weights (SWC), where
We defined the censoring indicator as if a woman was lost to follow-up at interview 2 and otherwise. We assumed that censoring at interview 2 was random, with the probability of attending interview 2 depending on prior social support, baseline covariates, and depression at interview 1. Further details on the characteristics of women who were lost to follow-up are available in the Web Table 2.
The censoring weights were multiplied by the treatment weights to create a final stabilized weight for each woman.
When fitting MSMs using inverse-probability weights, we made the following 4 assumptions (42): conditional exchangeability (28, 41, 43), positivity, correct specification of models used to estimate weights, and consistency. In addition, we performed a sensitivity analysis for unmeasured confounding to assess the extent to which unmeasured residual confounding would explain away the observed associations (44, 45). Without imposing any assumptions on the unmeasured confounders, we calculated the E-value as a representation of the minimum strength of association that an unmeasured confounder would need to have with the exposure and outcome to nullify an observed exposure-outcome association (OR) (44–46). The formula for the E-value is: for common outcomes. We assessed model misspecification based on the distribution of stabilized weights (42).
We conducted additional analyses to test the robustness of our results. We fitted multivariate logistic regression models for the associations of social support during early pregnancy on depression in late pregnancy, adjusting for baseline covariates, social support before pregnancy, and depression in early pregnancy. In addition, we modeled the SSQS and SSQN as continuous variables.
All statistical analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
Sociodemographic and reproductive characteristics are provided in Tables 1 and 2. At interview 1, compared with women reporting high satisfaction with social support, women reporting low satisfaction with social support were less likely to have more than 12 years of education, to report the active pregnancy as planned, and to be nulliparous; they also tended to have difficulties in accessing basic foods and to have experienced childhood abuse and intimate partner violence prior to pregnancy (Table 1). Compared with women who reported having a high number of support providers, women who reported having a low number of support providers were more likely to be 35 years or older, to have difficulties in accessing basic foods, and to have experienced childhood abuse and intimate partner violence prior to pregnancy; they were less likely to identify themselves as Mestizo, to have received more than 12 years of education, or to be nulliparous (Table 2). At interview 2, similar patterns of sociodemographic and reproductive characteristics were seen (Tables 1 and 2).
Table 1.
Characteristics of Women According to Social Support Status Measured by Social Support Satisfaction in the Pregnancy Outcomes, Maternal and Infant Cohort Study, Peru, 2012–2014
| Characteristic | Satisfaction With Social Support | |||||||||
| Before Pregnancya | Since Becoming Pregnantb | |||||||||
| High (n = 1,576) | Low (n = 1,760) | P Value | High (n = 1,058) | Low (n = 1,221) | P Value | |||||
| No. | % | No. | % | No. | % | No. | % | |||
| Maternal age, yearsc | 28.1 (6.2) | 28.3 (6.4) | 0.44 | 27.9 (6.1) | 28.4 (6.2) | 0.10 | ||||
| Maternal age group, years | 0.59 | 0.42 | ||||||||
| 18–19 | 86 | 5.5 | 86 | 4.9 | 52 | 4.9 | 58 | 4.8 | ||
| 20–29 | 879 | 55.8 | 980 | 55.7 | 607 | 57.4 | 665 | 54.5 | ||
| 30–34 | 339 | 21.5 | 363 | 20.6 | 228 | 21.6 | 272 | 22.3 | ||
| ≥35 | 272 | 17.3 | 331 | 18.8 | 171 | 16.2 | 226 | 18.5 | ||
| Education, years | <0.0001 | 0.0008 | ||||||||
| ≤6 | 60 | 3.8 | 85 | 4.8 | 35 | 3.3 | 59 | 4.8 | ||
| 7–12 | 765 | 48.5 | 1,051 | 59.7 | 531 | 50.2 | 684 | 56.0 | ||
| >12 | 746 | 47.3 | 620 | 35.2 | 489 | 46.2 | 474 | 38.8 | ||
| Mestizo ethnicity | 1,191 | 75.6 | 1,318 | 74.9 | 0.60 | 808 | 76.4 | 918 | 75.2 | 0.48 |
| Married/living with partner | 1,277 | 81.0 | 1,414 | 80.3 | 0.54 | 863 | 81.6 | 986 | 80.8 | 0.85 |
| Employed during pregnancy | 713 | 45.2 | 820 | 46.6 | 0.43 | 474 | 44.8 | 569 | 46.6 | 0.38 |
| Access to basic foods | 0.002 | 0.004 | ||||||||
| Hard | 739 | 46.9 | 919 | 52.2 | 490 | 46.3 | 639 | 52.3 | ||
| Not very hard | 836 | 53.0 | 840 | 47.7 | 568 | 53.7 | 582 | 47.7 | ||
| Planned pregnancy | 707 | 44.9 | 689 | 39.1 | 0.001 | 478 | 45.2 | 482 | 39.5 | 0.006 |
| Nulliparous | 804 | 51.0 | 826 | 46.9 | 0.02 | 548 | 51.8 | 583 | 47.7 | 0.05 |
| Gestational age at interview 1, weeksc | 9.1 (3.5) | 9.3 (3.5) | 0.13 | 9.5 (3.4) | 9.6 (3.5) | 0.24 | ||||
| Early pregnancy body mass indexd | ||||||||||
| <18.5 | 33 | 2.1 | 30 | 1.7 | 0.84 | 19 | 1.8 | 23 | 1.9 | 0.24 |
| 18.5–24.9 | 744 | 47.2 | 844 | 48.0 | 523 | 49.4 | 591 | 48.4 | ||
| 25.0–29.9 | 578 | 36.7 | 637 | 36.2 | 394 | 37.2 | 433 | 35.5 | ||
| ≥30.0 | 204 | 12.9 | 226 | 12.8 | 112 | 10.6 | 163 | 13.3 | ||
| Childhood abuse | 1,068 | 67.8 | 1,306 | 74.2 | <0.0001 | 744 | 70.3 | 910 | 74.5 | 0.02 |
| Lifetime intimate partner violence (physical or sexual) | 466 | 29.6 | 745 | 42.4 | <0.0001 | 324 | 30.6 | 473 | 38.8 | 0.0002 |
| Lifetime abuse | ||||||||||
| No abuse | 404 | 25.6 | 330 | 18.8 | <0.0001 | 257 | 24.3 | 223 | 18.3 | <0.0001 |
| Childhood abuse only | 701 | 44.5 | 682 | 38.8 | 476 | 45.0 | 522 | 42.8 | ||
| Intimate partner violence only | 104 | 6.6 | 124 | 7.0 | 57 | 5.4 | 88 | 7.2 | ||
| Childhood abuse and intimate partner violence | 362 | 23.0 | 621 | 35.3 | 267 | 25.2 | 385 | 31.5 | ||
a Low social support satisfaction before pregnancy was defined as a score of ≤33 on the Social Support Questionnaire Satisfaction Scale (at interview 1).
b Low social support satisfaction since becoming pregnant was defined as a score of ≤32 on the Social Support Questionnaire Satisfaction Scale (at interview 2).
c Values are expressed as mean (standard deviation).
d Weight (kg)/height (m)2.
Table 2.
Characteristics of Women According to Social Support Status Measured by Number of Available Support Providers in the Pregnancy Outcomes, Maternal and Infant Cohort Study, Peru, 2012–2014
| Characteristic | Number of Available Support Providers | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before Pregnancya | Since Becoming Pregnantb | |||||||||
| High (n = 1,299) | Low (n = 2,037) | P Value | High (n = 996) | Low (n = 1,283) | P Value | |||||
| No. | % | No. | % | No. | % | No. | % | |||
| Maternal age, yearsc | 27.5 (5.9) | 28.6 (6.5) | <0.0001 | 27.5 (6.0) | 28.7 (6.2) | <0.0001 | ||||
| Maternal age group, years | <0.0001 | 0.0007 | ||||||||
| 18–19 | 70 | 5.4 | 102 | 5.0 | 59 | 5.9 | 51 | 4.0 | ||
| 20–29 | 783 | 60.3 | 1,076 | 52.8 | 589 | 59.1 | 683 | 53.2 | ||
| 30–34 | 265 | 20.4 | 437 | 21.5 | 198 | 19.9 | 302 | 23.5 | ||
| ≥35 | 181 | 13.9 | 422 | 20.7 | 150 | 15.1 | 247 | 19.3 | ||
| Education, years | <0.0001 | <0.0001 | ||||||||
| ≤6 | 3.0 | 106 | 5.2 | 27 | 2.7 | 67 | 5.2 | |||
| 7–12 | 633 | 48.7 | 1,183 | 58.1 | 492 | 49.4 | 723 | 56.4 | ||
| >12 | 624 | 48.0 | 742 | 36.4 | 472 | 47.4 | 491 | 38.3 | ||
| Mestizo ethnicity | 1,035 | 79.7 | 1,474 | 72.4 | <0.0001 | 773 | 77.6 | 953 | 74.3 | 0.06 |
| Married/living with partner | 1,057 | 81.4 | 1,634 | 80.2 | 0.46 | 772 | 77.5 | 1,077 | 83.9 | 0.0001 |
| Employed during pregnancy | 580 | 44.6 | 953 | 46.8 | 0.24 | 444 | 44.6 | 599 | 46.7 | 0.33 |
| Access to basic foods | 0.002 | 0.26 | ||||||||
| Hard | 603 | 46.4 | 1,055 | 51.8 | 480 | 48.2 | 649 | 50.6 | ||
| Not very hard | 696 | 53.6 | 980 | 48.1 | 516 | 51.8 | 634 | 49.4 | ||
| Planned pregnancy | 562 | 43.3 | 834 | 40.9 | 0.17 | 436 | 43.8 | 524 | 40.8 | 0.15 |
| Nulliparous | 711 | 54.7 | 919 | 45.1 | <0.0001 | 547 | 54.9 | 584 | 45.5 | <0.0001 |
| Gestational age at interview 1, weeksc | 9.2 (3.5) | 9.2 (3.4) | 0.97 | 9.5 (3.5) | 9.6 (3.4) | 0.70 | ||||
| Early pregnancy body mass indexd | 0.006 | 0.50 | ||||||||
| <18.5 | 30 | 2.3 | 33 | 1.6 | 18 | 1.8 | 24 | 1.9 | ||
| 18.5–24.9 | 661 | 50.9 | 927 | 45.5 | 503 | 50.5 | 611 | 47.6 | ||
| 25.0–29.9 | 436 | 33.6 | 779 | 38.2 | 356 | 35.7 | 471 | 36.7 | ||
| ≥30.0 | 158 | 12.2 | 272 | 13.4 | 111 | 11.1 | 164 | 12.8 | ||
| Childhood abuse | 853 | 65.7 | 1,521 | 74.7 | <0.0001 | 688 | 69.1 | 966 | 75.3 | 0.001 |
| Lifetime intimate partner violence (physical or sexual) | 362 | 27.9 | 849 | 41.7 | <0.0001 | 289 | 29.0 | 508 | 39.7 | <0.0001 |
| Lifetime abuse | <0.0001 | <0.0001 | ||||||||
| No abuse | 363 | 27.9 | 371 | 18.2 | 249 | 25.0 | 231 | 18.0 | ||
| Childhood abuse only | 572 | 44.0 | 811 | 39.8 | 457 | 45.9 | 541 | 42.2 | ||
| Intimate partner violence only | 83 | 6.4 | 145 | 7.1 | 59 | 5.9 | 86 | 6.7 | ||
| Childhood abuse and intimate partner violence | 279 | 21.5 | 704 | 34.6 | 230 | 23.1 | 422 | 32.9 | ||
a Low number of available support providers before pregnancy was defined as a score of ≤8 (at interview 1) on the Social Support Questionnaire Number Scale.
b Low number of available support providers since becoming pregnant was defined as a score of ≤8 (at interview 2) on the Social Support Questionnaire Number Scale.
c Values are expressed as mean (standard deviation).
d Weight (kg)/height (m)2.
Using marginal structural models (Table 3, Web Tables 3 and 4), compared with women reporting high social support both before and during early pregnancy (reference group), women were at increased risk of depression in late pregnancy if they reported, at both time points, low satisfaction with social support (adjusted odds ratio (aOR) = 1.41, 95% confidence interval (CI): 0.99, 1.99) and low number of support providers (aOR = 1.62, 95% CI: 1.12, 2.34). The risk of depression in late pregnancy was not significantly higher among women who reported low social support before pregnancy and high social support during early pregnancy (for low satisfaction, aOR = 0.88, 95% CI: 0.57, 1.35; for low number of support providers, aOR = 0.84, 95% CI: 0.54, 1.31) or high social support before pregnancy but low social support during early pregnancy (for low satisfaction, aOR = 1.43, 95% CI: 0.97, 2.10; for low number of support providers, aOR = 1.38, 95% CI: 0.89, 2.14).
Table 3.
Associations Between Social Support and Antepartum Depression in Late Pregnancy Using Marginal Structural Models in the Pregnancy Outcomes, Maternal and Infant Cohort Study, Peru, 2012–2014
| Social Support (Before Pregnancy) | Social Support (Since Becoming Pregnant) | Marginal Structural Model | |
|---|---|---|---|
| aOR | 95% CI | ||
| Satisfaction with social support | |||
| Lowa | Lowb | 1.41 | 0.99, 1.99 |
| Low | High | 0.88 | 0.57, 1.35 |
| High | Low | 1.43 | 0.97, 2.10 |
| High | High | 1.00 | Referent |
| Number of available support providers | |||
| Lowc | Lowd | 1.62 | 1.12, 2.34 |
| Low | High | 0.84 | 0.54, 1.31 |
| High | Low | 1.38 | 0.89, 2.14 |
| High | High | 1.00 | Referent |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval.
a Low social support satisfaction before pregnancy was defined as a score of ≤33 on the Social Support Questionnaire Satisfaction Scale (at interview 1).
b Low social support satisfaction since becoming pregnant was defined as a score of ≤32 on the Social Support Questionnaire Satisfaction Scale (at interview 2).
c Low number of available support providers before pregnancy was defined as a score of ≤8 on the Social Support Questionnaire Number Scale.
d Low number of available support providers since becoming pregnant was defined as a score of ≤8 on the Social Support Questionnaire Number Scale.
Next, we evaluated satisfaction with social support and number of available support providers as continuous variables (Table 4). No statistically significant association was observed between satisfaction with social support and antepartum depression. An increase by 1 available support provider at one of the 2 time points was associated with decreased risk of antepartum depression (prior to pregnancy, aOR = 0.85, 95% CI: 0.73, 0.98; during early pregnancy, aOR = 0.73, 95% CI: 0.63, 0.84). There was a 37% (aOR = 0.63, 95% CI: 0.49, 0.81) decrease in the risk of antepartum depression for 1-unit increase in available support providers at both time points.
Table 4.
Inverse-Probability-of-Treatment Weighted Estimates of the Causal Association of Social Support (Continuous) on Antepartum Depression at Interview 2, Pregnancy Outcomes, Maternal and Infant Cohort Study, Peru, 2012–2014
| Social Support Score | aOR | 95% CI |
|---|---|---|
| Satisfaction with social support | ||
| Before pregnancy (per 5 units) | 1.01 | 0.52, 1.95 |
| Since becoming pregnant (per 5 units) | 0.75 | 0.36, 1.56 |
| Before pregnancy (per 5 units) × since becoming pregnant (per 5 units) | 0.76 | 0.20, 2.92 |
| Number of available support providers | ||
| Before pregnancy (per 1 unit) | 0.85 | 0.73, 0.98 |
| Since becoming pregnant (per 1 unit) | 0.73 | 0.63, 0.84 |
| Before pregnancy (per 1 unit) × since becoming pregnant (per 1 unit) | 0.63 | 0.49, 0.81 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval.
We observed similar estimates from multivariate logistic regression compared with the estimates from the MSMs (Web Table 5). Next, we completed sensitivity analyses to evaluate the extent to which an unmeasured confounder would fully explain away the observed estimates. For example, for the observed estimate of aOR = 1.62 for the low number of support providers before pregnancy and in early pregnancy, an unmeasured confounder associated with both low number of support providers and depression by risk ratios of 2.02-fold each, above and beyond the measured confounders, would explain away the association, but weaker confounding would not. To shift the lower bound of the confidence limit of 1.12 to include the null, an unmeasured confounder that was associated with low number of support providers and depression by risk ratios of 1.39-fold each would suffice, but weaker confounding would not. This association is thus relatively robust to potential unmeasured confounding.
DISCUSSION
In this prospective cohort study, after applying methods that adjusted for potential confounding and the intermediary role of depression during early pregnancy, we found that women with low social support at both (early and late pregnancy) interview time points were at higher risk of depression in late pregnancy. Depression risk was not significantly higher among women who reported high social support at one of the 2 time points. We observed a stronger association with a low number of support providers, compared with low satisfaction with social support, on depression risk.
Consistent with many previous studies (2, 10, 16, 22, 23, 26), we found that low social support was associated with higher risk of depression. One possible mechanism involved in this association is the buffering effect of social support. The buffering hypothesis proposes that social support is related to health only (or primarily) when stressful life events occur (47). This hypothesis predicts that social support will protect individuals from the potentially negative impact of stressful events (47), and thus protect against depression by altering perceptions of negative events; enhancing an individual’s self-esteem, self-confidence, and self-efficacy; transferring coping resources; and facilitating changes in health-related behaviors (7, 10, 48).
A larger magnitude of associations between social support during early pregnancy, compared with before pregnancy, with antepartum depression were found in our study. This finding suggested that interventions aimed at increasing social support during early pregnancy might be more influential on depression risk than social support prior to pregnancy. In addition, our results demonstrated a stronger association of the low number of support providers on depression risk in late pregnancy compared with low social support satisfaction. The difference between the number of support providers and satisfaction with social support in relation to depression was also seen in previous studies. For example, significant associations were reported for the number of social support providers during pregnancy with postpartum depression but not the satisfaction with social support during pregnancy (2, 24). As suggested by Sarason et al. (32), the number of support providers, a measure for perceived social support network size, and satisfaction with social support, a measure of the perceived quality of social support, reflected 2 different aspects of perceived social support, and different aspects of social support were associated with different health outcomes (49). Our results suggest benefits of interventions targeted at increasing the number of support providers to prevent antepartum depression (2).
Our results also provide valuable quantitative information on the development of practical interventions. A hypothetical intervention on social support designed to increase by 1 available support provider for one of the 6 situations in the SSQ-6 before pregnancy or during early pregnancy would decrease the risk of depression in late pregnancy. A greater decrease in the risk of depression was seen when the intervention was targeted at increasing available support providers during early pregnancy compared with prior to pregnancy. The available support providers could be friends, family members, or health professionals such as mental health and medical professionals, because pregnancy is a time that women come into frequent contact with healthcare providers. Of note, different sources of social support relationship have different strengths and mechanisms of support for pregnant women (16, 18). For example, in a sample of 156 outpatients with major depression, Clara et al. (50) found that perceived social support provided by family and friends had the strongest association with depression. Future studies illuminating how the source of social support affects the risk of antepartum depression during pregnancy is warranted.
As noted previously, MSMs require several assumptions. For conditional exchangeability, we assumed that measured covariates were sufficient to adjust for both confounding and selection bias due to loss to follow-up. Sensitivity analyses for unmeasured confounding indicated that relatively substantial residual unmeasured confounding was needed to explain away the observed significant associations of early pregnancy social support with depression. With regard to positivity, we concluded that the assumption of positivity was likely to hold in our analysis based on descriptive statistics (Tables 1 and 2) when social support measures were dichotomized. The assumption of correct model specification was likely to hold considering that stabilized weights had a mean of 1 (Web Table 1), a necessary condition for correct model specification (42). We might fail to satisfy the assumptions of consistency. Consistency was not straightforward in our situation (42, 51, 52). It is difficult to intervene on a woman’s satisfaction with social support. In addition, a woman could achieve a high number of available support providers through different pathways (53), which could have different implications for the outcome. For our analysis, we defined the high number of available support providers as a summary endpoint of these different pathways.
This study had some limitations. First, there might be a timing overlap between depression measured at interview 1 (Dep1, in the 7 days prior to interview 1) and social support measured at interview 2 (SS2, since becoming pregnant). However, interview 1 was conducted during the first prenatal visit, which was unlikely to be a long time after women learned they were pregnant. Therefore, we would not expect a drastic change in social support between pregnancy confirmation and the first prenatal visit. Second, we measured only perceived social support, one of the 3 main aspects of social support (social integration, received support, or perceived support), in this study (10). Nevertheless, prior research suggested that the perceived level of social support might be more important to an individual’s mental health than the objective level of social support (11). Third, measures of social support might be susceptible to recall bias, especially for social support measured at interview 1, which covered a long time period. Fourth, we defined depressive state using a depression screening instrument, the EPDS, rather than diagnostic interviews completed by psychiatrists.
The strengths of this study included the large sample size of pregnant women, repeated measures of social support and depression, the inclusion of 2 distinct aspects of perceived social support, and the analytical methods accounting for the bidirectional relationship between social support and depression. Furthermore, we adjusted for a wide range of potential confounders, including reproductive and abuse history, using validated questionnaires.
In conclusion, in our prospective study in a cohort of pregnant Peruvian women, we found that consistently low social support before pregnancy and during early pregnancy was associated with increased risk of antepartum depression at late pregnancy, with the associations being stronger in relation to the number of available support providers. Social support during early pregnancy is more influential on the risk of antepartum depression than is social support prior to pregnancy. Assessing social support before and during pregnancy would likely help identify pregnant women vulnerable to depression. The development of interventions targeted at increasing the number of support providers would be beneficial in preventing antepartum depression. Future studies illuminating how different sources of social support affect the risk of depression during pregnancy are warranted.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, Massachusetts (Qiu-Yue Zhong, Bizu Gelaye, Tyler J. VanderWeele, Michelle A. Williams); and Asociación Civil Proyectos en Salud, Lima, Peru (Sixto E. Sanchez); and Facultad de Medicina, Universidad Peruana de Ciencias Aplicados, Lima, Peru (Sixto E. Sanchez).
This research was supported by an award from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant R01-HD-059835).
We thank the dedicated staff members of Asociación Civil Proyectos en Salud, Peru, and Instituto Especializado Materno Perinatal, Peru, for their expert technical assistance with this research. We also thank Dr. Changzheng Yuan for her help with analysis.
The National Institutes of Health had no further role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Conflict of interest: none declared.
Abbreviations
- aOR
adjusted odds ratio
- CI
confidence interval
- EPDS
Edinburgh Postnatal Depression Scale
- MSM
marginal structural model
- SSQ-6
Social Support Questionnaire–6
- SSQN
Social Support Questionnaire Number Scale
- SSQS
Social Support Questionnaire Satisfaction Scale
REFERENCES
- 1. King M, Nazareth I, Levy G, et al. . Prevalence of common mental disorders in general practice attendees across Europe. Br J Psychiatry. 2008;192(5):362–367. [DOI] [PubMed] [Google Scholar]
- 2. Morikawa M, Okada T, Ando M, et al. . Relationship between social support during pregnancy and postpartum depressive state: a prospective cohort study. Sci Rep. 2015;5:10520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization Maternal Mental Health and Child Health and Development in low and Middle Income Countries: Report of the Meeting Geneva, Switzerland: World Health Organization; 2008. http://apps.who.int/iris/bitstream/10665/43975/1/9789241597142_eng.pdf. [Google Scholar]
- 4. Zhong Q, Gelaye B, Rondon M, et al. . Comparative performance of Patient Health Questionnaire–9 and Edinburgh Postnatal Depression Scale for screening antepartum depression. J Affect Disord. 2014;162:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chung TK, Lau TK, Yip AS, et al. . Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosom Med. 2001;63(5):830–834. [DOI] [PubMed] [Google Scholar]
- 6. Sidebottom AC, Harrison PA, Godecker A, et al. . Validation of the Patient Health Questionnaire (PHQ)-9 for prenatal depression screening. Arch Womens Ment Health. 2012;15(5):367–374. [DOI] [PubMed] [Google Scholar]
- 7. Cohen S, Gottlieb BH, Underwood LG. Social relationships and health In: Cohen S, Underwood LG, Gottlieb BH, eds. Social Support Measurement and Intervention: A Guide for Health and Social Scientists. New York, NY: Oxford University Press; 2000:3–28. [Google Scholar]
- 8. Giesbrecht GF, Poole JC, Letourneau N, et al. . The buffering effect of social support on hypothalamic-pituitary-adrenal axis function during pregnancy. Psychosom Med. 2013;75(9):856–862. [DOI] [PubMed] [Google Scholar]
- 9. Rini C, Schetter CD, Hobel CJ, et al. . Effective social support: antecedents and consequences of partner support during pregnancy. Pers Relatsh. 2006;13(2):207–229. [Google Scholar]
- 10. Ibarra-Rovillard MS, Kuiper NA. Social support and social negativity findings in depression: perceived responsiveness to basic psychological needs. Clin Psychol Rev. 2011;31(3):342–352. [DOI] [PubMed] [Google Scholar]
- 11. Park M, Cuijpers P, van Straten A, et al. . The effects of psychotherapy for adult depression on social support: a meta-analysis. Cognit Ther Res. 2014;38(6):600–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cronin LBA. Low social support and major depression: research, theory and methodological issues In: Dobson KS, Dozois DJA, eds. Risk Factors in Depression. San Diego, CA: Elsevier Academic Press; 2008:385–408. [Google Scholar]
- 13. Gladstone GL, Parker GB, Malhi GS, et al. . Feeling unsupported? An investigation of depressed patients’ perceptions. J Affect Disord. 2007;103(1–3):147–154. [DOI] [PubMed] [Google Scholar]
- 14. Stice E, Ragan J, Randall P. Prospective relations between social support and depression: differential direction of effects for parent and peer support? J Abnorm Psychol. 2004;113(1):155–159. [DOI] [PubMed] [Google Scholar]
- 15. Oxman TE, Hull JG. Social support, depression, and activities of daily living in older heart surgery patients. J Gerontol B Psychol Sci Soc Sci. 1997;52B(1):P1–P14. [DOI] [PubMed] [Google Scholar]
- 16. Spoozak L, Gotman N, Smith MV, et al. . Evaluation of a social support measure that may indicate risk of depression during pregnancy. J Affect Disord. 2009;114(1–3):216–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Werner E, Miller M, Osborne LM, et al. . Preventing postpartum depression: review and recommendations. Arch Womens Ment Health. 2015;18(1):41–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. O’Hara MW. Social support, life events, and depression during pregnancy and the puerperium. Arch Gen Psychiatry. 1986;43(6):569–573. [DOI] [PubMed] [Google Scholar]
- 19. Mckee MD, Cunningham M, Jankowski KR, et al. . Health-related functional status in pregnancy: relationship to depression and social support in a multi-ethnic population. Obstet Gynecol. 2001;97(6):988–993. [DOI] [PubMed] [Google Scholar]
- 20. Rahman A, Iqbal Z, Harrington R. Life events, social support and depression in childbirth: perspectives from a rural community in the developing world. Psychol Med. 2003;33(7):1161–1167. [DOI] [PubMed] [Google Scholar]
- 21. Chen CM, Kuo SF, Chou YH, et al. . Postpartum Taiwanese women: their postpartum depression, social support and health-promoting lifestyle profiles. J Clin Nurs. 2007;16(8):1550–1560. [DOI] [PubMed] [Google Scholar]
- 22. Xie RH, He G, Koszycki D, et al. . Prenatal social support, postnatal social support, and postpartum depression. Ann Epidemiol. 2009;19(9):637–643. [DOI] [PubMed] [Google Scholar]
- 23. Westdahl C, Milan S, Magriples U, et al. . Social support and social conflict as predictors of prenatal depression. Obstet Gynecol. 2007;110(1):134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Husain N, Cruickshank K, Husain M, et al. . Social stress and depression during pregnancy and in the postnatal period in British Pakistani mothers: a cohort study. J Affect Disord. 2012;140(3):268–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stuchbery M, Matthey S, Barnett B. Postnatal depression and social supports in Vietnamese, Arabic and Anglo-Celtic mothers. Soc Psychiatry Psychiatr Epidemiol. 1998;33(10):483–490. [DOI] [PubMed] [Google Scholar]
- 26. Webster J, Nicholas C, Velacott C, et al. . Quality of life and depression following childbirth: impact of social support. Midwifery. 2011;27(5):745–749. [DOI] [PubMed] [Google Scholar]
- 27. Liabsuetrakul T, Vittayanont A, Pitanupong J. Clinical applications of anxiety, social support, stressors, and self-esteem measured during pregnancy and postpartum for screening postpartum depression in Thai women. J Obstet Gynaecol Res. 2007;33(3):333–340. [DOI] [PubMed] [Google Scholar]
- 28. VanderWeele TJ, Hawkley LC, Thisted RA, et al. . A marginal structural model analysis for loneliness: implications for intervention trials and clinical practice. J Consult Clin Psychol. 2011;79(2):225–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Felitti VJ, Anda RF, Nordenberg D, et al. . Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. [DOI] [PubMed] [Google Scholar]
- 30. The DHS Program Demographic health survey questionnaires and modules: domestic violence module. 2005. https://dhsprogram.com/publications/publication-DHSQM-DHS-Questionnaires-and-Manuals.cfm. Accessed January 1, 2011.
- 31. Sarason IG, Sarason BR, Shearin EN, et al. . A brief measure of social support: practical and theoretical implications. J Soc Pers Relat. 1987;4(4):497–510. [Google Scholar]
- 32. Sarason IG, Levine HM, Basham RB, et al. . Assessing social support: the social support questionnaire. J Pers Soc Psychol. 1983;44(1):127–139. [Google Scholar]
- 33. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. [DOI] [PubMed] [Google Scholar]
- 34. Bal S, Crombez G, Van Oost P, et al. . The role of social support in well-being and coping with self-reported stressful events in adolescents. Child Abuse Negl. 2003;27(12):1377–1395. [DOI] [PubMed] [Google Scholar]
- 35. Sewitch MJ, Abrahamowicz M, Bitton A, et al. . Psychological distress, social support, and disease activity in patients with inflammatory bowel disease. Am J Gastroenterol. 2001;96(5):1470–1479. [DOI] [PubMed] [Google Scholar]
- 36. Maunder RG, Nolan RP, Hunter JJ, et al. . Relationship between social support and autonomic function during a stress protocol in ulcerative colitis patients in remission. Inflamm Bowel Dis. 2012;18(4):737–742. [DOI] [PubMed] [Google Scholar]
- 37. Sewitch MJ, Abrahamowicz M, Bitton A, et al. . Psychosocial correlates of patient-physician discordance in inflammatory bowel disease. Am J Gastroenterol. 2002;97(9):2174–2183. [DOI] [PubMed] [Google Scholar]
- 38. Dalmida SG, Koenig HG, Holstad MM, et al. . The psychological well-being of people living with HIV/AIDS and the role of religious coping and social support. Int J Psychiatry Med. 2013;46(1):57–83. [DOI] [PubMed] [Google Scholar]
- 39. Gibson J, McKenzie-McHarg K, Shakespeare J, et al. . A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350–364. [DOI] [PubMed] [Google Scholar]
- 40. Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560. [DOI] [PubMed] [Google Scholar]
- 41. Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11(5):561–570. [DOI] [PubMed] [Google Scholar]
- 42. Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hernán MA, Brumback BA, Robins JM. Estimating the causal effect of zidovudine on CD4 count with a marginal structural model for repeated measures. Stat Med. 2002;21(12):1689–1709. [DOI] [PubMed] [Google Scholar]
- 44. Ding P, VanderWeele TJ. Sensitivity analysis without assumptions. Epidemiology. 2016;27(3):368–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–274. [DOI] [PubMed] [Google Scholar]
- 46. Ananth CV, Schisterman EF. Hidden biases in observational epidemiology: the case of unmeasured confounding. BJOG. 2018;125(6):644–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 48. Nezlek JB, Kowalski RM, Leary MR, et al. . Personality moderators of reactions to interpersonal rejection: depression and trait self-esteem. Pers Soc Psychol Bull. 1997;23(12):1235–1244. [Google Scholar]
- 49. Uchino BN. What a lifespan approach might tell us about why distinct measures of social support have differential links to physical health. J Soc Pers Relat. 2009;26(1):53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Clara IP, Cox BJ, Enns MW, et al. . Confirmatory factor analysis of the multidimensional scale of perceived social support in clinically distressed and student samples. J Pers Assess. 2003;81(3):265–270. [DOI] [PubMed] [Google Scholar]
- 51. Hernán MA. Invited commentary: hypothetical interventions to define causal effects—afterthought or prerequisite? Am J Epidemiol. 2005;162(7):618–620. [DOI] [PubMed] [Google Scholar]
- 52. Hernán MA, Taubman SL. Does obesity shorten life? The importance of well-defined interventions to answer causal questions. Int J Obes (Lond). 2008;32(suppl 3):S8–S14. [DOI] [PubMed] [Google Scholar]
- 53. Cole SR, Frangakis CE. The consistency statement in causal inference: a definition or an assumption? Epidemiology. 2009;20(1):3–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.