Short abstract
Objective
This study was performed to compare the functional and anatomical results of endoscopic-assisted and temporary keratoprosthesis (TKP)-assisted vitrectomy in patients with combat ocular trauma (COT).
Methods
The medical records of 14 severely injured eyes of 12 patients who underwent endoscopy or TKP implantation in combination with vitreoretinal surgery from 2007 to 2015 were retrospectively evaluated. The patients’ ocular history and functional and anatomic anterior and posterior segment results were analyzed.
Results
Eight eyes (57%) underwent TKP-assisted vitrectomy and six eyes (43%) underwent endoscopic vitrectomy. The most common cause of COT was detonation of improvised explosive devices (72%), and the most common type of injury was an intraocular foreign body (50%). The median time from trauma to surgery and the median surgical time were significantly shorter in the endoscopy than TKP group. The postoperative functional and anatomical results were not significantly different between the two groups.
Conclusions
TKP-assisted vitrectomy should be performed in eyes requiring extensive bimanual surgery. In such cases, a corneal graft must be preserved for the TKP at the end of the surgery. Endoscopy shortens the surgical time and can reduce the complication rate.
Keywords: Combat ocular trauma, temporary keratoprosthesis, endoscopy, vitrectomy, complications, functional outcome, anatomical outcome
Introduction
The rates of eye injuries on battlefields have increased with war-related changes that have led to increased use of explosives during the last century.1,2 Although the development of high-quality body armor has decreased the vulnerability of the chest and abdomen, an increasing proportion of injuries occur to unprotected areas, such as the eyes.3 Ocular tissue is more vulnerable to projectile injuries than are other parts of the body.3 Open-globe injury and combat ocular trauma (COT) in the posterior segment of the eye have poor visual outcomes.4
Corneal opacities often result from severe ocular trauma and may complicate the diagnosis and management of posterior segment pathology.5 The cornea was reportedly involved in 46% of perforating injuries during Iraqi operations of US troops.6 Corneal clarity may be affected by severe corneal edema, sutures, glue, foreign bodies, and distortion caused by large repaired defects.5 Given the features of COT, most affected patients require the performance of vitreoretinal surgery (VRS) within a few days after the injury.4 In ocular trauma with opaque corneas, early intervention with an intraoperative viewing system may prevent iatrogenic injury and some late complications.5,7 Techniques used in such cases are the open-sky technique, temporary keratoprosthesis (TKP) implantation, penetrating keratoplasty, and endoscopic surgery.
Several studies have examined various TKPs for vitrectomy combined with penetrating keratoplasty following ocular trauma.5 A TKP maintains a closed globe with normal intraocular pressure, increasing the success of vitrectomy and keratoplasty with a clear corneal graft in a single surgical procedure.8 However, TKPs can be associated with intraoperative complications and a prolonged surgery time, and the requirement of a corneal graft at the end of the surgery is a limitation of this technique.
Endoscopy for posterior segment pathologies in patients with opaque corneas is a valuable diagnostic procedure. Since the introduction of the first described ophthalmic endoscope prototypes, the size, resolution, and maneuverability of these endoscopes have been optimized.9 The present study was performed to compare the functional and anatomical results of endoscopic-assisted and TKP-assisted vitrectomy in patients with COT. The results of this study will provide clinicians with valuable information for rapid decision-making regarding the optimal vitrectomy technique in patients who present with COT.
Material and methods
Patients
The data of patients who underwent vitrectomy with endoscopy or TKP implantation in our clinic from January 2007 to December 2015 were retrospectively reviewed. The study was approved by the local ethics committee and adhered to the tenets of the Helsinki declaration, and informed consent was obtained from all patients. The inclusion criteria were a history of COT requiring vitrectomy, an opaque cornea without the required intraocular view for endoscopy or TKP implantation, and a follow-up of at least 6 months (Figure 1). The exclusion criteria were poor documentation in the medical record, previous surgeries, or a short follow-up. Baseline characteristics including age, ocular diagnosis, medical history, visual acuity, intraocular pressure, anterior and posterior ocular findings, and surgeries were recorded.
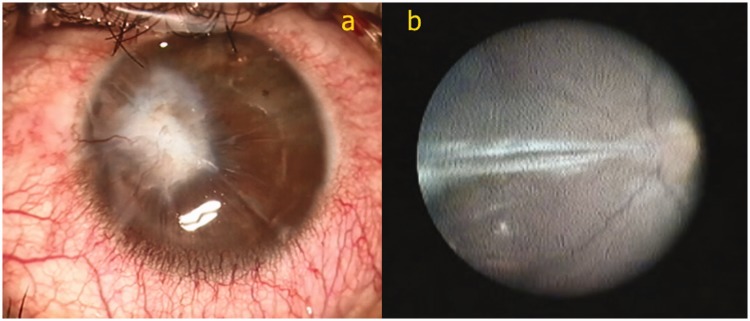
Figure 1.
A 29-year-old patient. He had an open globe injury in his right eye due to detonation of an improvised explosive device. Only primary suture closure was performed for this eye at the primary center. His visual acuity was hand movements at presentation. The patient had a right eye perforating injury affecting zone 1, and his ocular trauma score was 45. He had a centrally opaque cornea (a). No view of the posterior segment was possible. Tractional retinal detachment was present, and he underwent endoscopic vitrectomy (b).
Definitions
Ocular trauma was classified according to the Ocular Trauma Classification, and the Ocular Trauma Score was calculated for each eye.10,11 According to the Ocular Trauma Classification, a full-thickness wound of the eyewall is defined as an open-globe injury. The other definitions are as follows: rupture, a full-thickness wound of the eyewall caused by a blunt object; laceration, a full-thickness wound of the eyewall usually caused by a sharp object; penetrating injury, a single laceration of the eyewall usually caused by a sharp object; perforating injury, two full-thickness lacerations of the eyewall; and intraocular foreign body (IOFB) injury, a retained foreign object causing an entrance laceration.10 An IOFB is actually a penetrating injury, but is grouped separately because of different clinical implications (treatment modality, timing, and rate of endophthalmitis).10
Surgical procedures
Patients underwent either implantation of an Eckardt TKP (Heinrich Wöhlk Kontaktlinsen, Kiel, Germany) or use of an endoscopic system (Endo Optiks E4 Endoscopy System; Endo Optiks Inc., Little Silver, NJ, USA) for intraocular visualization.
In all eyes, primary wound closure was performed before admission to our clinic. All surgeries in our clinic were performed under general anesthesia. The surgical approach was determined based on the urgency of the case, availability of a donor cornea, and surgeon’s choice. Before implantation of the TKP, a scleral fixation ring was sutured to the sclera. A trephine was then used to excise a corneal button. Cataract extraction and other anterior segment surgeries were performed as necessary. After suture fixation of the Eckardt TKP, a standard three-port, 23-gauge pars plana vitrectomy was performed using the Accurus and Constellation systems (Alcon, Fort Worth, TX, USA). An Eibos wide-angle viewing system (Möller-Wedel, Wedel, Germany) was used during the surgery. Pars plana lensectomy, scleral buckling, IOFB removal, membrane stripping, relaxing retinectomy, endolaser therapy, and cryotherapy were performed when needed. For IOFB removal, the superior temporal sclerotomy was enlarged depending on the diameter of the IOFB. After the VRS, the Eckardt TKP was removed, and implantation of a donor cornea was performed during the same surgical session. At the end of the procedure, fluid/air/gas or air/silicone oil exchange was made. The silicone oil was removed 3 to 6 months after the surgery.
The endoscopic procedures were performed when any indication for vitrectomy was identified without waiting for corneal clearing. The endoscopic system housed a 20-gauge curved probe and a 17,000-pixel camera with a 140-degree viewing angle. A high-resolution monitor (PVM-14M2MDU; Sony, Tokyo, Japan) was also used for video display. The endoscope probe was inserted into the eye through a 20-gauge sclerotomy incision. The other sclerotomy incisions were used for the irrigation cannula and vitrectomy cutter as in conventional pars plana vitrectomy. The VRS was performed as usual. However, the vitreoretinal procedures were followed on the monitor instead of through a microscope. The fundus was evaluated by ultrasonography in the follow-up period after endoscopic surgery.
Statistical analysis
Data analysis was performed using IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, NY, USA). The data are expressed as percentage values or as group mean and standard deviation or median and range values. Comparisons between the groups were performed using the Mann–Whitney U test and Fisher’s exact test. A p-value of <0.05 was accepted as statistically significant.
Results
This study included 14 eyes of 12 male patients, the characteristics of whom are listed in Table 1. Eight eyes of six patients (57%) underwent TKP implantation, and six eyes of six patients (43%) underwent endoscopic-assisted vitrectomy. The most common cause of COT was detonation of improvised explosive devices (72%), also known as roadside bombs. Improvised explosive devices are mostly homemade, highly destructive explosives and that usually include additional materials such as rocks, metals, or glass fragments to increase the lethal effects of shrapnel propelled by the explosion.12 The other causes of COT were mine explosions (14%), hand grenade detonation (7%), and rockets (7%). The type of trauma was open-globe injury in all eyes, and the mean follow-up period was 12 months (range, 9–34 months).
Table 1.
Patients’ ocular trauma data and preoperative characteristics
| Characteristics | TKP | Endoscopy | Total |
|---|---|---|---|
| No. of eyes** | 8 | 6 | 14 |
| Age, years* | 22 ± 2 | 25 ± 4 | 24 ± 3 |
| Ocular trauma score* | 68 (36–70) | 69 (45–80) | 69 (36–80) |
| Type of injury** | |||
| IOFB | 4 | 3 | 7 |
| Penetrating | 1 | 1 | 2 |
| Perforating | 2 | 2 | 4 |
| Rupture | 1 | 0 | 1 |
| Preoperative characteristics** | |||
| BCVA ≥20/200 | 0 | 0 | 0 |
| Vitreous hemorrhage | 4 | 4 | 8 |
| Traumatic aphakia | 2 | 1 | 3 |
| Traumatic cataract | 6 | 4 | 10 |
| Traumatic maculopathy | 1 | 3 | 4 |
| Traumatic optic neuropathy | 1 | 1 | 2 |
| Retinal tears | 6 | 6 | 12 |
| Retinal detachment | 5 | 5 | 10 |
| PVR | 2 | 3 | 5 |
| Choroidal hemorrhage | 2 | 1 | 3 |
| Time to surgery, days* | 38 (15–104) | 12 (5–38) | 31 (5–104) |
| Surgical time, hours* | 4.0 (3.6–5.3) | 2.9 (2.4–4.1) | 3.7 (2.4–5.3) |
Data are presented as n, mean ± standard deviation, or median (range).
*Mann–Whitney U test, **Fischer’s exact test.
BCVA, best-corrected visual acuity; IOFB, intraocular foreign body; PVR, proliferative vitreoretinopathy; TKP, temporary keratoprosthesis.
No differences in the number of eyes, mean age, ocular trauma variables, or preoperative characteristics were found between the TKP and endoscopy groups (p > 0.05). The median time from trauma to surgery and the median surgical time were significantly shorter in the endoscopy than TKP group (p = 0.03 and p = 0.04, respectively).
No differences in ocular trauma variables were present between the TKP and endoscopy groups (Table 1). IOFB was the most common type of injury (50%), and 42% of all eyes had zone III injuries. The two groups were similar with respect to the preoperative characteristics (Table 1). None of the eyes had vision better than 20/200 preoperatively. The most common baseline ocular findings were traumatic cataract, retinal tears, and retinal detachment. All retinal tears were diagnosed intraoperatively.
The median time from trauma to surgery and the median surgical time were significantly shorter in the endoscopy than TKP group (p = 0.03 and p = 0.04, respectively) (Table 1). There were no differences in the surgical procedures performed between the two groups.
Six of the 14 eyes (43%) had 20/200 or better best-corrected visual acuity (BCVA) at 9 months postoperatively (Table 2). Six of 8 eyes (75%) in the TKP group had clear corneal grafts, and 11 of 14 eyes (79%) in the whole study cohort showed retinal attachment (Figure 2). Two eyes (14%) had worse vision than 20/200 because of corneal graft failure, and three eyes (21%) had worse vision than 20/200 because of recurrent retinal detachment at 9 months postoperatively. Repeat penetrating keratoplasty and repeat retinal detachment repair were performed for these eyes. Optic atrophy, proliferative vitreoretinopathy, and glaucoma were the other causes of low vision. The postoperative functional and anatomical results were not significantly different between the two groups.
Table 2.
Postoperative results at 9 months
| Results* | TKP (n = 8) | Endoscopy (n = 6) | Total (n = 14) |
|---|---|---|---|
| BCVA ≥20/200 | 2 | 4 | 6 |
| Clear corneal graft | 6 | – | – |
| Retinal attachment | 6 | 5 | 11 |
| Causes of BCVA ≤20/200 | |||
| Corneal graft failure | 2 | – | – |
| Retinal detachment | 2 | 1 | 3 |
| Optic atrophy | 1 | 0 | 1 |
| PVR | 1 | 0 | 1 |
| Glaucoma | 0 | 1 | 1 |
TKP, temporary keratoprosthesis; BCVA, best-corrected visual acuity; PVR, proliferative vitreoretinopathy.
*There was no significant difference in the postoperative results between the two groups (Fischer’s exact test, p > 0.05).
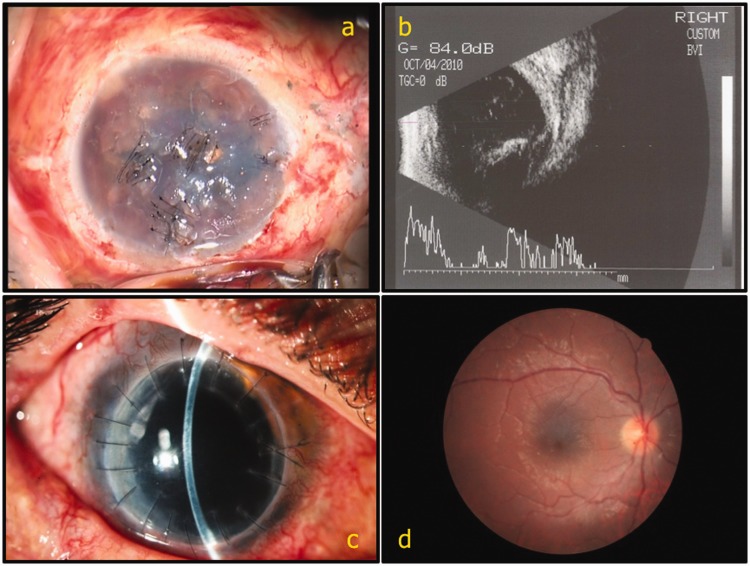
Figure 2.
A 20-year-old patient with open globe injuries in his eyes after a mine explosion. At the primary center, only primary suture closure was performed for his right eye, and evisceration of his left eye was performed. His visual acuity was hand movements in his right eye at presentation. He had an opaque cornea (a). No view of the posterior segment was possible. Orbital ultrasound revealed an inferiorly located retinal detachment (b). The patient had a right eye penetrating injury affecting zone 3, and his ocular trauma score was 60. He underwent temporary keratoprosthesis implantation and vitrectomy. His vision was 20/200 at the first month. At the ninth month, his vision improved to 20/40 and he still had a clear corneal graft and attached retina (c, d).
Discussion
COT differs from noncombat trauma. In COT, the male:female ratio is 24:1; in noncombat trauma, however, the male:female ratio is 4:1.13 Previous studies have revealed that blast or explosion injuries account for 79% of COT compared with 3% of noncombat trauma.13 In the current study, all patients were young men injured by explosive devices or blast effects. Regardless of how severely injured the eyes were secondary to COT in this study, 57% of the eyes had a BCVA of less than 20/200 at 9 months postoperatively. A total of 27% of COT-affected eyes have BCVA worse than 20/200 in the United States Eye Injury Registry, and 33% of COT-affected eyes have BCVA worse than 20/200.13,14 Several risk factors for a poor visual outcome after ocular trauma have been identified.15 These factors are poor initial visual acuity, afferent pupillary defect, vitreous hemorrhage, choroidal hemorrhage, globe perforation, globe rupture, and retinal detachment.13,15 In the present study, the number of patients was too low for statistical analysis of all of these risk factors, but retinal detachment, corneal graft failure, optic atrophy, proliferative vitreoretinopathy, and glaucoma were causes of BCVA of less than 20/200 at 9 months postoperatively.
Vitrectomy in a severely injured eye, especially with an opaque cornea, is associated with many technical difficulties. An endoscope or TKP is useful to visualize the retina during vitrectomy in these eyes. TKPs have some advantages including a clear view of the posterior segment, increased ease of surgery, binocularity, and stereopsis.16 However, after the vitrectomy, the need for a donor cornea for penetrating keratoplasty is a disadvantage. Moreover, surgical implantation of the TKP prolongs the operative period, and the open-sky stage is associated with a risk of suprachoroidal hemorrhage.16 Loss of transparency of the corneal graft is another problem when performing combined keratoplasty and vitrectomy. In the present study, 75% of eyes (n = 6) in the TKP group had BCVA worse than 20/200, two cases of which were due to corneal graft failure. The complexity of surgery, intraoperative manipulations, postoperative inflammation, and use of silicone oil are reported causes of graft failure.16,17 Minimally invasive surgery and effective anti-inflammatory treatment are necessary to obtain corneal clarity. It has also been suggested that a clear corneal graft can be obtained if an endoscope is used first and penetrating keratoplasty is performed later, thus stabilizing the eye and removing the silicone oil.18
Ophthalmic endoscopy is a valuable technology in the field of VRS. The ability to bypass anterior segment opacities makes it a useful tool for eyes with corneal edema or scarring. Additionally, it is useful for the complex surgeries required to treat open globe injuries or COT, especially those involving retinal detachment and IOFBs. The duration of surgery with endoscopy is shorter than that with TKP implantation because complex procedures such as keratoprosthesis and corneal graft implantation are avoided. The endoscope is not simply a diagnostic tool; with its high-magnification and high-resolution imaging and tangential approach, it allows for the performance of surgical tasks that would be difficult or impossible to accomplish with traditional viewing techniques.7 The endoscope makes scleral indentation unnecessary. However, endoscopy also has some disadvantages and difficulties. The learning curve is quite steep. Loss of stereopsis during viewing from a monitor is another difficulty. The high cost of the instruments, limited field of view, and difficulty of bimanual surgery are other limitations.16 Nonetheless, previous studies have shown that endoscopic vitrectomy improves anatomical and functional outcomes with the capability of earlier intervention and lower rates of proliferative vitreoretinopathy and postoperative retinal detachment.7,9 Endoscopic-assisted vitrectomy is an effective method for treating the sequelae of COT. Not only the corneal opacity but also the IOFB is a complicating factor in COT. An IOFB was the most common type of injury in our study. Endoscopy can allow detection and later removal of an IOFB that is not recognized preoperatively.8 A retained IOFB is a risk factor for post-traumatic endophthalmitis; therefore, early intervention is required in eyes with trauma, especially COT.9,18
The main limitations of this study are its retrospective nature and small sample size. Additionally, we reviewed and compared the results of TKP-assisted and endoscopic-assisted vitrectomies that were described previously.5,8,16 To the best of our knowledge, however, this is the first reported experience from a tertiary eye center in Turkey. Moreover, our study may contribute to the reproducibility of these techniques.
In conclusion, TKP implantation should be performed in eyes with complex anterior and posterior segment injuries requiring extensive bimanual surgery. A corneal graft must be reserved for TKP implantation at the end of the surgery. However, endoscopic surgery requires long-term training, and the learning curve is very steep. In our experience, endoscopic surgery has some advantages over TKP. It allows earlier intervention and shorter surgical times and can reduce the complications associated with TKPs. Endoscopy provides more time for the surgeon to find a useful corneal graft for implantation. Additionally, the postoperative inflammation is less severe after endoscopic surgery than after TKP implantation.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Wong TY, Seet MB, Ang CL. Eye injuries in twentieth century warfare: a historical perspective. Surv Ophthalmol 1997; 41: 433–459. [DOI] [PubMed] [Google Scholar]
- 2.Ünlü A, Cetinkaya RA, Ege T, et al. Role 2 military hospitals: results of a new trauma care concept on 170 casualties. Eur J Trauma Emerg Surg 2015; 41: 149–155. [DOI] [PubMed] [Google Scholar]
- 3.Thomas R, McManus JG, Johnson A, et al. Ocular injury reduction from ocular protection use in current combat operations. J Trauma 2009; 66: S99–S103. [DOI] [PubMed] [Google Scholar]
- 4.Boiko EV, Churashov SV, Haritonova NN, et al. Vitreoretinal surgery in the management of war-related open-globe injuries. Graefes Arch Clin Exp Ophthalmol 2013; 251: 637–644. [DOI] [PubMed] [Google Scholar]
- 5.Chun DW, Colyer MH, Wroblewski KJ. Visual and anatomic outcomes of vitrectomy with temporary keratoprosthesis or endoscopy in ocular trauma with opaque cornea. Ophthalmic Surg Lasers Imaging 2012; 43: 302–310. [DOI] [PubMed] [Google Scholar]
- 6.Colyer MH, Weber ED, Weichel ED, et al. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology 2007; 114: 1439–1447. [DOI] [PubMed] [Google Scholar]
- 7.Morishita S, Kita M, Yoshitake S, et al. 23-gauge vitrectomy assisted by combined endoscopy and a wide-angle viewing system for retinal detachment with severe penetrating corneal injury: a case report. Clin Ophthalmol 2011; 5: 1767–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roters S, Szurman P, Hermes S, et al. Outcome of combined penetrating keratoplasty with vitreoretinal surgery for management of severe ocular injuries. Retina 2003; 23: 48–56. [DOI] [PubMed] [Google Scholar]
- 9.Marra KV, Yonekawa Y, Papakostas TD, et al. Indications and techniques of endoscope assisted vitrectomy. J Ophthalmic Vis Res 2013; 8: 282–290. [PMC free article] [PubMed] [Google Scholar]
- 10.Kuhn F, Morris R, Witherspoon CD, et al. A standardized classification of ocular trauma. Ophthalmology 1996; 103: 240–243. [DOI] [PubMed] [Google Scholar]
- 11.Kuhn F, Maisiak R, Mann L, et al. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am 2002; 15: 163–165. [DOI] [PubMed] [Google Scholar]
- 12.Erdurman FC, Hurmeric V, Gokce G, et al. Ocular injuries from improvised explosive devices. Eye (Lond) 2011; 25: 1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weichel ED, Colyer MH, Ludlow SE, et al. Combat ocular trauma visual outcomes during operations Iraqi and enduring freedom. Ophthalmology 2008; 115: 2235–2245. [DOI] [PubMed] [Google Scholar]
- 14.Kuhn F, Morris R, Witherspoon CD, et al. Epidemiology of blinding trauma in the United States Eye Injury Registry. Ophthalmic Epidemiol 2006; 13: 209–216. [DOI] [PubMed] [Google Scholar]
- 15.Schmidt GW, Broman AT, Hindman HB, et al. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology 2008; 115: 202–209. [DOI] [PubMed] [Google Scholar]
- 16.Sabti KA, Raizada S. Endoscope-assisted pars plana vitrectomy in severe ocular trauma. Br J Ophthalmol 2012; 96: 1399–403. [DOI] [PubMed] [Google Scholar]
- 17.Noorily SW, Foulks GN, McCuen BW. Results of penetrating keratoplasty associated with silicone oil retinal tamponade. Ophthalmology 1991; 98: 1186–1189. [DOI] [PubMed] [Google Scholar]
- 18.Ahmed Y, Schimel AM, Pathengay A, et al. Endophthalmitis following open-globe injuries. Eye (Lond) 2012; 26: 212–217. [DOI] [PMC free article] [PubMed] [Google Scholar]