Abstract
Community-based organisations (CBOs) are important for eliminating health disparities globally and translating research findings to inform interventions. Engagement is an integral part of partnerships between CBOs and community health researchers and impacts the quality and quantity of any desired outcome. Despite the acknowledged benefits of community-based organisation engagement (CBOE), there are variations in its operationalisation and paucity in the understanding of its use in community-scientific partnerships. To further understand CBOE, the aim of this study was to synthesise published literature relevant to the definitions and applications of CBOE and identify its key components. A systematic search was conducted in March 2017, and updated in June 2017. Keywords were varied to account for international differences in spelling and word usage. Five major databases, MEDLINE, PubMed, CINAHL, PsycINFO and Google Scholar, were used to identify potential research studies. A total of 32 studies were included in this review. Following the analysis of the literature, four salient themes emerged as components of CBOE: (1) Need (a consensus between all the parties in a partnership on the importance of a specified project and its proposed benefits to a target community); (2) Partnership Dynamics (the workings of a relationship between a CBO and a scientific/academic stakeholder); (3) Resources (include but are not limited to: personnel, money, work space, expertise and equipment); and (4) Outcomes (products of the partnership). This review provides a foundation for future research in applying CBOE to translational research and interventions. This analysis will assist community health researchers in planning partnerships with CBOs, and make necessary adjustments to improve study outcomes. Appropriate application of the components of CBOE in partnerships will assist researchers in addressing health disparities.
Keywords: community engagement, community-based organisation, community-based organization, community-based organisation engagement, community-based participatory research, translational research
1 |. BACKGROUND
Community-based organisations (CBOs) are an important part of research and creating successful interventions (Blakeney et al., 2015; Clinical and Translational Science Awards Consortium, 2011). A CBO is defined as a public or private non-profit organisation that represents a community or a specific part of a larger community, and targets meeting a specific need in that community (Caldwell, Reyes, Rowe, Weinert, & Israel, 2015; Glik et al., 2014; National Network of Libraries of Medicine, 2015). CBOs have been shown to provide access to target clients and resources needed for research/interventions, serve as liaisons between researchers and the community, disseminate findings and troubleshoot unexpected challenges (Blakeney et al., 2015; Burkhalter et al., 2013; Caldwell et al., 2015; Houston, Harada, & Makinodan, 2002). CBOs can improve the outcomes and relevance of research or interventions conducted in communities (Akintobi et al., 2012; Burkhalter et al., 2013; Caldwell et al., 2015; Darling et al., 2015).
Community-based participatory research (CBPR) is an approach or methodology that involves an equal partnership between scientific or academic entities and community stakeholders (e.g. members, researchers, organisations) in the research process of projects that aim to promote community health (Israel, Schulz, Parker, & Becker, 1998). CBPR has become popular in recent years due to its promising capability to generate programmes to improve health outcomes that are well positioned for adoption by communities (Faridi, Grunbaum, Gray, Franks, & Simoes, 2007). The effectiveness of CBPR in improving health outcomes among high-risk populations has been documented (Minkler & Wallerstein, 2008). Important elements for successful CBPR include power-sharing, building trust, effective communication, establishing mutually beneficial goals, and colearning/capacity building between community stakeholders and researchers, as well as funding, sustainability, finding the right stakeholders and resources (Caldwell et al., 2015; Fitzpatrick, 2016; Jurkowski & Manganello, 2016; Katigbak, Foley, Robert, & Hutchinson, 2016; McDonald & Stack, 2016). An inability to achieve these elements can present challenges to the implementation of CBPR and prevent the success of CBPR projects. Effective engagement within community-scientific partnerships has received less attention, though it may mitigate the barriers and challenges to its implementation.
In the current scientific literature, there is no consensus on how “community engagement” is defined. In describing engagement, “community” is often conceptualised as either the people affected by a particular problem, or the parties (e.g. academic institutions, community institutions, government institutions, health professionals and policy makers) involved in any particular project for a community, or an organisation that serves the needs of a specific group of people (Blakeney et al., 2015; Clinical and Translational Science Awards Consortium, 2011; Drake & Whitley, 2014; Patel et al., 2011). This difference in conceptualisation can lead to confusion regarding the meaning of community engagement, which may be linked to the prior cited challenges in the successful implementation of CBPR. The purpose of this paper was to specifically examine one type of community engagement that which occurs between CBOs and scientific/academic institutions. We refer to this as community-based organisation engagement (CBOE).
CBOE is defined as the collaborative interaction process of a CBO working with a scientific/academic institution to meet needs and improve health among a target population; a group of people bounded by a geographical location, disease, special interest or situation, that is affiliated with said CBO (Chandra et al., 2013; Clinical and Translational Science Awards Consortium, 2011; Kakietek et al., 2013; National Network of Libraries of Medicine, 2015). CBOE is an integral part of community-scientific partnerships (Bloom et al., 2009; Burkhalter et al., 2013; Honeycutt et al., 2015). CBOE increases the credibility and appropriateness of research projects to target the complex, multilevel nature of health disparities (Burkhalter et al., 2013; Honeycutt et al., 2015). Additionally, CBOE aids in ensuring accountability for research initiatives, and provides opportunities for sustained research partnerships and new collaborations (Johnson, Bobbitt-Cooke, Schwarz, & White, 2006). Furthermore, CBOE has become an especially important issue, because it impacts the research processes and the quality or quantity of the desired outcome in CBPR (Clinical and Translational Science Awards Consortium, 2011; Tait, Birchwood, & Trower, 2002). Therefore, non-engagement is a problem for researchers, clinicians and consequently the health of the public (Tait et al., 2002).
In CBOE, CBOs use their knowledge of the target community to positively influence a research project through active involvement in decision-making, planning and implementation (Chandra et al., 2013; Singer, Bennett-Levy, & Rotumah, 2015). Literature suggests that CBOE may be a major predictor of outcomes in public health (Clinical and Translational Science Awards Consortium, 2011; Patel et al., 2011). However, it is mostly acknowledged at the end of the research process, as opposed to earlier phases (Drake & Whitley, 2014; Roush, Monica, Pavlovich, & Drake, 2015). The problem with this is that not capturing CBOE early on in the research process can negatively influence a project or partnership (Clinical and Translational Science Awards Consortium, 2011). Additionally, there is a paucity in the understanding of CBOE among research partnerships (Bloom et al., 2009; Drake & Whitley, 2014), which may be due to the variation in operational definitions of CBOE (Chandra et al., 2013; Honeycutt et al., 2015; Kakietek et al., 2013; Singer et al., 2015). Not understanding the different nuances of community engagement (e.g. CBOE vs. participant engagement) may play a role in this “late engagement” phenomena and paucity of implementation. Therefore, a need for clear definitions of community engagement and its domains is apparent. The majority of literature on community engagement and CBPR has evaluated the engagement of study participants or community members (Blakeney et al., 2015; Clinical and Translational Science Awards Consortium, 2011; Drake & Whitley, 2014; Patel et al., 2011). However, little has been done to understand how researchers or scientific/academic institutions engage with CBOs (i.e. CBOE), and the effect of different levels of community engagement on research. To further understand CBOE, this systematic review aims to summarise published literature on CBOE and identify a consensus on its key components.
2 |. METHOD
2.1 |. Literature search
This review was guided by The Principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines for data retrieval and reporting (Moher, Liberati, Tetzlaff, & Altman, 2009). A systematic review of the literature was conducted in March 2017 and updated in June 2017, to identify key articles. The search accounted for the international difference in spelling of a keyword, ‘organization’ and ‘organisation’. Five major databases, MEDLINE, PubMed, CINAHL, PsycINFO, and Google Scholar were searched using the following key search term categories: Community Based Organization* AND Engag*, Community Based Organisation* AND Engag*, CBO* AND Engag*, Community Organization* AND Engag*, Community Organisation* AND Engag*. There was no temporal restriction on the search of the databases. There were no restrictions on the country of publication to account for a global perspective of CBOE. Titles and abstracts were reviewed by one author to identify articles published in English language that discussed engagement related to CBOs. Articles selected for full-article review were reviewed by two authors. Grey literature (magazines, commentary, conference proceedings, editors report and dissertation/thesis) were excluded from the review. During review of the full-text, ancestry search was undertaken to identify references that met the inclusion criteria. The inclusion criteria were: (a) articles published in English language; and (b) articles that described, defined or discuss engagement in CBOs. In each of the reviewed full texts, the reviewers abstracted: (a) descriptions of CBOE; (b) factors that led to CBOE; (c) activities that constituted CBOE; and (d) consequences of CBOE.
2.2 |. Data evaluation and abstraction
The articles included in this review consisted of original studies (quantitative, qualitative and mixed-method), case study and review articles. The review articles, qualitative studies and quantitative studies were appraised with The Critical Appraisal Skills Programme (CASP) (“Critical Appraisal Skills Programme [CASP] (2013). Retrieved from http://www.casp-uk.net/casp-tools-checklists“). The CASP consists of different versions based on the different designs of the study. For this review, the following CASP versions were used for appraisal: (a) CASP Systematic Review Checklist; (b) CASP Cohort Study Checklist; (c) CASP Qualitative Checklist (“CASP (2013). Retrieved from http://www.casp-uk.net/casp-tools-checklists“). Each study was assigned a score of 1 for a fulfilled criterion, and a score of 0 for an unfulfilled criterion. The maximum score varied based on the version of the CASP tool, ranging from 10 to 12. The case study articles were appraised with the Center for Evidence-Based Medicine (CEBM) Critical Appraisal Checklist (“Center for Evidence-Based Medicine (CEBM) Critical Appraisal of a Case Study (2017). Retrieved from https://www.cebma.org/wp-content/uploads/Critical-Appraisal-Questions-for-a-Case-Study.pdf“). Case studies were scored 1 for a fulfilled criterion and 0 for an unfulfilled criteria, with a maximum score of 10 (“CEBM Critical Appraisal of a Case Study (2017). Retrieved from https://www.cebma.org/wp-content/uploads/Critical-Appraisal-Questions-for-a-Case-Study.pdf“). The Mixed Method Analysis Tool (MMAT) was used to appraise the mixed-method studies (Pluye et al., 2011). Each mixed-method study was assigned a score of 25% for a fulfilled criterion, and a score of 0 for an unfulfilled criterion, leading to a maximum score of 100%.
Data were abstracted and appraised by two authors, and findings were reviewed by the other two authors to ensure objectivity and credibility. Data were abstracted from the sections in the articles that discussed or described CBOE. Data abstraction occurred from the method, results and discussion section of the reviewed articles. Upon data abstraction, the first author synthesised findings and developed four overarching themes that described the findings. These themes were evaluated by other authors, and verified for consistency and accuracy. Table 1 presents the different studies and their inclusion of the different CBOE components.
Table 1.
Inclusion of CBOE components among included articles
3 |. RESULTS
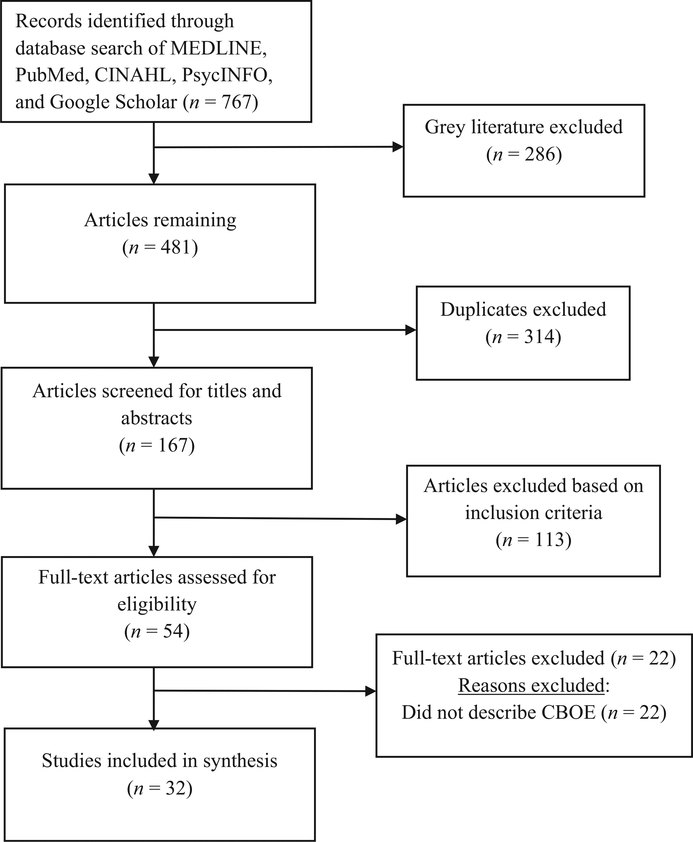
The search of the databases identified 767 articles, 286 of which were grey literature. The 481 remaining titles were compiled and 314 duplicate titles were removed. These duplicates were the sum of the same articles retrieved from the different databases and search term categories. The titles and abstracts of 167 articles were screened and 113 were excluded; 54 full-text articles were reviewed. Following full-text review, 22 articles did not meet the inclusion criteria of the review. The reference list of the articles was reviewed but no new articles were found. The final pool consisted of 32 articles published between 2001 and 2016. Figure 1 presents the process for article review and selection.
FIGURE 1.
Flow diagram of studies examined for systematic review
3.1 |. Overview of Studies
The studies that analysed CBO partnerships, shared lessons learned from CBO partnerships and evaluated individual cases of engagement of CBOs were grouped and appraised as case studies. The majority of studies (n = 13) in this review were case studies. The remaining studies included quantitative design (Bloom et al., 2009; Chandra et al., 2013; Geist, 2010; Glik et al., 2014; Goytia et al., 2013; Patterson et al., 2011); qualitative design (Boutain & McNees, 2013; Burkhalter et al., 2013; Collignon, Men, & Tan, 2001; Honeycutt et al., 2015; Johnson et al., 2006; Radermacher, Karunarathna, Grace, & Feldman, 2011; Taras et al., 2015); systematic review (Frew et al., 2014); and mixed-method design (Houston et al., 2002; Kakietek et al., 2013; Kelaher et al., 2014; Laborde, Brannock, Breland-Noble, & Parrish, 2007; Riehman et al., 2013).
High variability was found during critical appraisal of case studies, with scores ranging from 1 to 10 (Akintobi et al., 2012; Caldwell et al., 2015; Chaskin, Goerge, Skyles, & Guiltinan, 2006; Darling et al., 2015; LoConte, Weeth-Feinstein, Conlon, & Scott, 2013; McFarlane, Kahili, & Johnson, 2014; Napoles et al., 2014; Panapasa et al., 2012; Singer et al., 2015). Five studies met all the criteria (Chaskin et al., 2006; Darling et al., 2015; Gainforth, Latimer-Cheung, Moore, Athanasopoulos, & Martin Ginis, 2015; Jewett-Tennant et al., 2016; Woodruff et al., 2016). Points were deducted from case studies that did not describe the methods, analysis and results for the project itself (Caldwell et al., 2015; Panapasa et al., 2012; Singer et al., 2015; Tisnado et al., 2010). Other case studies lost points for not describing the analysis and the conclusions drawn (LoConte et al., 2013; McFarlane et al., 2014; Napoles et al., 2014). All the quantitative and qualitative studies scored 8 and above with the CASP tools. Two qualitative studies met all the CASP tool’s criteria (Boutain & McNees, 2013; Taras et al., 2015). The other qualitative studies lost points for the absence of data analysis process and study limitations (Collignon et al., 2001; Honeycutt et al., 2015; Johnson et al., 2006; Radermacher et al., 2011). Three quantitative studies met all the criteria from CASP tool (Chandra et al., 2013; Glik et al., 2014; Goytia et al., 2013). Points were deducted from quantitative studies that did not describe: the measures used and data collection strategy (Bloom et al., 2009; Geist, 2010; Patterson et al., 2011). The systematic review met all the CASP tool criteria (Frew et al., 2014). The mixed-method studies were rated between 75% and 100%. One mixed-method study met all the criteria of the MMAT (Riehman et al., 2013). The other mixed-method studies lost points for reasons that include: not delineating different objectives or research questions for both qualitative and quantitative methods, not describing the analysis process for either of the collected data and lack of description for measures used in collecting quantitative data (Akintobi et al., 2012; Houston et al., 2002; Kakietek et al., 2013; Kelaher et al., 2014· Laborde et al., 2007) The studies in this review were included regardless of their appraisal score to provide an overall state of science on CBOE.
In the articles, descriptions of CBOE were elicited in different ways. Some examples are: evaluation of research partnerships with CBOs (Bloom et al., 2009; Honeycutt et al., 2015; Riehman et al., 2013), process of engagement of CBOs (Akintobi et al., 2012; Boutain & McNees, 2013; Chandra et al., 2013; Chaskin et al., 2006; Goytia et al., 2013; Johnson et al., 2006; Radermacher et al., 2011; Singer et al., 2015; Taras et al., 2015) and experiences/lessons from research partnerships with CBOs (Darling et al., 2015; McFarlane et al., 2014; Napoles et al., 2014; Taras et al., 2015). The components that were discovered from the articles were synthesised and categorised leading to the emergence of four salient themes: Need, Partnership Dynamics, Resources and Outcomes. These have been summarised in Table 2.
Table 2.
Domains of community-based organisation engagement
| Domain | Definition | Key characteristics |
|---|---|---|
| Needs | A consensus between all parties in a partnership of the importance of a particular project and its benefits. | 1. A community need is required for a CBO
to engage in a research project 2. Understanding and consensus regarding the aims of the proposed research from both the CBO and stakeholder are required for CBOE to occur 3. Identified needs should align with the mission, vision or goals of the CBO |
| Partnership dynamics | The norms, values and mission that guide the actions of a partnership between a CBO and stakeholder. | 1. Partnership dynamics may provide
structure and guidance for a CBO 2. Partnership dynamics are facilitated when CBOs are involved throughout the entire duration of the research project 3. CBO trust and contribution are two components of partnership dynamics that can affect the outcomes of a partnership |
| Resources | The available means in a partnership that contribute to the success of a research project. | 1. Resources may include personnel, money,
space, expertise and equipment 2. All members in a research partnership should possess resources to facilitate the project 3. Required resources will be linked to the aims of the project and existing conditions for a research project 4. Lack of resources and poor management of available resources are deterrents to engagement of CBOs |
| Outcomes | The product(s) that result(s) from research, and from the partnership itself. | 1. An important potential outcome of CBOE
is the generation of recommendations that could inform subsequent
research 2. CBOE could also lead to subsequent research opportunities with other organisations and sustenance of current research partnerships 3. CBOE leads to identified benefits for CBOs, such as new ideas, skills and experiences |
3.2 |. Need
A need can be defined as a consensus between all the parties in a partnership of the importance of a particular project to address both the needs of the community-academic partnership and a target community (Akintobi et al., 2012; Burkhalter et al., 2013; Caldwell et al., 2015; Frew et al., 2014; Gainforth et al., 2015; Tisnado et al., 2010; Woodruff et al., 2016).
The need for the community-academic partnership between CBOs and researchers provides the foundation for engagement and an assessment of the readiness of the CBO for said engagement (Akintobi et al., 2012; Woodruff et al., 2016). CBOs engage when they possess a clear understanding and are in consensus with stakeholders, regarding the aims of the proposed research projects and its benefits to the target community (Akintobi et al., 2012; Gainforth et al., 2015; Jewett-Tennant et al., 2016; Johnson et al., 2006). The roles, rights and responsibilities of the members of the partnership are also specified, clarified and verbalised, when the need for a partnership or project is identified (Bloom et al., 2009; Caldwell et al., 2015; Chaskin et al., 2006; Jewett-Tennant et al., 2016; Johnson et al., 2006; Laborde et al., 2007; LoConte et al., 2013; McFarlane et al., 2014; Napoles et al., 2014). Need for community-academic partnerships has been previously established by dialogues between leaders in CBOs and stakeholder institutions (Akintobi et al., 2012; Boutain & McNees, 2013; Burkhalter et al., 2013; Tisnado et al., 2010). Identifying the need for a partnership enables CBOs to be actively involved in selecting best approaches to achieve the goals of a research project, and promotes successful partnerships (Akintobi et al., 2012; Bloom et al., 2009; McFarlane et al., 2014). CBOs can identify the appropriate participants; determine effective means of accessibility; and assist in the development of assessment tools and data collection methods (Frew et al., 2014; Geist, 2010; Goytia et al., 2013; Honeycutt et al., 2015; Radermacher et al., 2011; Taras et al., 2015).
Furthermore, the identified need should align with the mission statements, visions or goals of the CBOs (Burkhalter et al., 2013; Caldwell et al., 2015; Chaskin et al., 2006; Darling et al., 2015; Geist, 2010; Johnson et al., 2006; McFarlane et al., 2014; Napoles et al., 2014). Similarly, the outcome or data collected should be of interest and practical importance to CBOs (Chaskin et al., 2006). CBOs in community-academic partnerships have to be familiar with the needs of the target community they serve (Radermacher et al., 2011). Need involves identifying research questions that are of interest to both CBOs and the target community (Darling et al., 2015). Additionally, in assessing need, CBOs past involvement in similar research projects should be evaluated to assess fit with new project (LoConte et al., 2013).
3.3 |. Partnership dynamics
The dynamics of a partnership describe the workings of a relationship between a CBO and a stakeholder. Most studies agree that partnership dynamics are facilitated when CBOs are involved throughout the duration of the research project as opposed to one point (Geist, 2010; Kelaher et al., 2014; Napoles et al., 2014; Singer et al., 2015). A CBO can contribute to a partnership through several ways that include: planning, recruitment, developing instruments, data collection, data analysis and interpretation, dissemination of findings, intervention development and providing recommendations (Bloom et al., 2009; Boutain & McNees, 2013; Chaskin et al., 2006; Honeycutt et al., 2015; Houston et al., 2002). Depending on the proposed project, one or more of these levels will be more appropriate. The point of contribution for a CBO is also important for engagement. For example, Honeycutt et al., 2015 reported that CBO engagement at the intervention phase of the research project ensured that findings were adequately utilised. CBOs are direct links to target communities they serve and can utilise findings from a study in the services they provide beyond the duration of the study or the partnership; they can also influence changes in policy and health outcomes of the target community (Honeycutt et al., 2015). If CBOs do not contribute or contribute inappropriately to a partnership, the outcomes of that partnership may be unfavourable (Chaskin et al., 2006). For example, in one study, a CBO was tasked with data collection for a research partnership and lacked adequate staff and resources necessary to carry out the activities, which led to: burdening of CBO staff members, delays in decisions and actions, and a change in the perception of the cost and benefit of engaging in the partnership (Chaskin et al., 2006).
Another important aspect of partnership dynamics is trust between CBOs and stakeholders (Akintobi et al., 2012; Bloom et al., 2009; Caldwell et al., 2015; Laborde et al., 2007; Taras et al., 2015; Tisnado et al., 2010). Trust in partnerships can be built through effective, regular and bidirectional communication through means like: regular meetings, conference calls, webinars and online dialogue (Akintobi et al., 2012; Bloom et al., 2009; Caldwell et al., 2015; Collignon et al., 2001; Darling et al., 2015; Glik et al., 2014; Honeycutt et al., 2015; Houston et al., 2002; Johnson et al., 2006; Napoles et al., 2014; Singer et al., 2015; Tisnado et al., 2010). Trust can also be developed through transparency of research processes and procedures, and accountability between members of the partnership (Akintobi et al., 2012; Caldwell et al., 2015; Laborde et al., 2007; Singer et al., 2015). The suggestions and inputs of the CBOs have to be acknowledged and should guide the research project wherever appropriate. Similarly, concerns of CBOs should be adequately addressed (Akintobi et al., 2012; Bloom et al., 2009; Chaskin et al., 2006; Houston et al., 2002; Kelaher et al.,.2014) For example, CBOs can provide input in development of protocols and trainings that will serve a target community (Bloom et al., 2009; Boutain & McNees, 2013).
In community-scientific partnerships, conflicts which are detrimental to engagement should be acknowledged; provisions for conflict resolution should be made at the onset of community-scientific partnerships (Bloom et al., 2009; Caldwell et al., 2015). An effective way to resolve conflicts is through dialogue (Darling et al., 2015; Napoles et al., 2014). In ensuring healthy partnership dynamics, stakeholders should be cognizant of the imbalance of power that could exist between CBOs and other members of the partnership (Bloom et al., 2009; Caldwell et al., 2015). CBOs should be treated as full partners with adequate decision-making power and fair compensation (Bloom et al., 2009; Chandra et al., 2013; Kelaher et al., 2014; Napoles et al., 2014; Panapasa et al., 2012; Tisnado et al., 2010). In a partnership, CBOs could lack adequate training, experience or expertise that other members of the partnership may possess (Bloom et al., 2009), which can lead to a power imbalance. Power imbalances should be addressed by targeting and intervening in areas of weakness (Caldwell et al., 2015). For example, staff in a CBO could be trained in research methods, conducts or approaches that will enable them to be active participants in a research project (Bloom et al., 2009). Unaddressed imbalances in power could lead to distrust, which impedes the development or growth of engagement (Bloom et al., 2009; Caldwell et al., 2015). Through the duration of research projects, partnerships should be continuously evaluated to determine where changes in roles of partners will benefit engagement (Bloom et al., 2009).
3.4 |. Resources
The success of a research project depends significantly on the resources available. Resources include but are not limited to: personnel, money, space, expertise and equipment (Bloom et al., 2009; Caldwell et al., 2015; Darling et al., 2015; Radermacher et al., 2011). All the members of a research partnership must possess adequate resources needed to facilitate a research project (Kelaher et al., 2014). For CBOs to be engaged in research partnerships, they have to be actively involved, which undertakes the utilisation of one or more resources (Goytia et al., 2013). First, there needs to be a clearly defined plan and consensus on what resources are needed and how they will be utilised for a project (Akintobi et al., 2012; Singer et al., 2015). Required resources will be linked to the aims of the project and existing conditions for a research project (Akintobi et al., 2012). CBOs can assist by identifying resources in target communities that will inform the research project (Akintobi et al., 2012; Woodruff et al., 2016). Outlining and identifying needed resources allows CBOs and other involved parties to understand what they contribute, how it will be contributed and its efficient use (Bloom et al., 2009). For example, staff in a CBO could be in charge of recruiting participants, providing informed consent and collecting data (Bloom et al., 2009; Chaskin et al., 2006; LoConte et al., 2013). Engagement of CBOs is facilitated when research projects and partnerships maximise the use of their resources and expertise, and build on existing resources (Chaskin et al., 2006; Darling et al., 2015; Glik et al., 2014; LoConte et al., 2013; Panapasa et al., 2012; Patterson et al., 2011).
Although a partnership requires involved parties to provide specific resources that will maximise the potential of the relationship, there are competing demands in a research project that call for prioritising the use of resources (Caldwell et al., 2015; Goytia et al., 2013). For example, financial resources are often limited and need to be addressed at the onset of partnerships (Caldwell et al., 2015; Goytia et al., 2013; Radermacher et al., 2011). Studies have shown that lack of resources and poor management of available resources are deterrents to engagement of CBOs (Kelaher et al., 2014; Radermacher et al., 2011). Financial resources can influence human resources by determining how many people can be employed by a CBO or parties in the partnership, which in turn influences their ability to initiate and sustain partnerships (Radermacher et al., 2011). For example, one article cited limited financial resources and insufficient staff as the reasons for reduced team meeting/event time which consequently led to poor engagement (Radermacher et al., 2011). Resources provide a pointer for the stability, experience, capacity and expertise of a CBO which influences their ability to effectively engage (Bloom et al., 2009; Burkhalter et al., 2013; LoConte et al., 2013). Additionally, a low level of engagement can lead to mismanagement of resources which could adversely affect meeting a target community’s need (Chaskin et al., 2006; Kelaher et al., 2014; Radermacher et al., 2011). For example, a CBO with insufficient staff can contribute inefficiently to the planning of a research project, which can in turn influence the effect on the target community. It is not unusual for CBOs to experience challenges in the owning and distribution of their resources, hence partnerships should harness the strength of CBOs as opposed to creating or requiring tasks that strain the resources of the CBO (Chaskin et al., 2006; Gainforth et al., 2015).
3.5 |. Outcome
Generally, engagement of CBOs creates and encourages trust, builds alliances, mediates relationships and improves health outcomes in the target community (Akintobi et al., 2012; Bloom et al., 2009; Burkhalter et al., 2013; Collignon et al., 2001; Houston et al., 2002; Johnson et al., 2006; Kakietek et al., 2013; Kelaher et al., 2014). Unlike outcomes for a research study, where the main focus is meeting the specific aims of that study, CBOE goes beyond the desired results of a research project and includes the product of the partnership (Caldwell et al., 2015; Darling et al., 2015; Johnson et al., 2006; Riehman et al., 2013).
An important consequence of CBOE is the generation of recommendations that could inform subsequent research initiatives (Bloom et al., 2009; Darling et al., 2015; Honeycutt et al., 2015). CBOE also leads to subsequent research opportunities with other organisations and a sustenance of current research partnerships (Darling et al., 2015; Houston et al., 2002; Laborde et al., 2007; LoConte et al., 2013). For example, the CBO could opt to continue partnerships that build upon the results of a completed research project (LoConte et al., 2013). Alternatively, a CBO can choose to discontinue a partnership if engagement was carried out ineffectively.
CBOE facilitates achievement of results that are beneficial to the target community (Akintobi et al., 2012; Bloom et al., 2009; Burkhalter et al., 2013; Collignon et al., 2001; Houston et al., 2002; Johnson et al., 2006; Kakietek et al., 2013; Kelaher et al., 2014). For example, a CBO that served abused Latina women engaged in a partnership that led to the development of a workplace intervention that increased the access and use of intimate partner violence (IPV) services that were culturally appropriate and incorporated into daily routines (Bloom et al., 2009). Other reported benefits to target communities were: removal of soda/ vending machines, increase in colorectal cancer screening, creation of jobs, availability of HIV/AIDS prevention services, reduced HIV risk behaviours, stress management for Latina women with breast cancer and reduction in air pollution (Boutain & McNees, 2013; Caldwell et al., 2015; Kakietek et al., 2013; Kelaher et al., 2014; LoConte et al., 2013; Napoles et al., 2014; Riehman et al., 2013).
CBOE also leads to identified benefits for CBOs (Collignon et al., 2001; Darling et al., 2015; Johnson et al., 2006; Napoles et al., 2014). Additionally, CBOE assists CBOs in developing their ability and capacity to undertake independent projects (Goytia et al., 2013). CBOs gain new ideas, skills and experiences through their involvement in research partnerships (Johnson et al., 2006; McFarlane et al., 2014). For example, in a study by McFarlane et al. (2014), CBO staff gained the ability to critically appraise literature following their involvement in a research partnership. The expertise and credibility of CBOs are also improved following effective CBOE (Goytia et al., 2013; McFarlane et al., 2014).
4 |. DISCUSSION
A systematic review of 32 studies was conducted to understand components necessary for effective CBOE. Upon analysis, four themes emerged including: Need, Partnership Dynamics, Resources and Outcomes. Effective engagement of CBOs requires an incorporation of the four identified components.
First, when a partnership is to be initiated, a meeting with key persons in the CBO and research institution is the initial step needed to identify the need and goals for the partnership. These should align with the vision and the mission of the CBO as well as the services they provide to their target communities (Burkhalter et al., 2013; Caldwell et al., 2015; Chaskin et al., 2006; Geist, 2010; Johnson et al., 2006; Napoles et al., 2014). For example, a CBO that provides services to HIV-infected youth will not effectively engage in a partnership aimed at reducing stress levels of elderly women. In identifying the need for a partnership, inputs from the CBO could further clarify the aims of the partnership as well as the purpose, methods and anticipated outcomes of the proposed project (Chaskin et al., 2006; Darling et al., 2015; Honeycutt et al., 2015; McFarlane et al., 2014; Napoles et al., 2014). For example, a CBO can provide information on needs of a target community, appropriate forms of recruitment and data collection, and effective ways of implementing interventions. Based on the identification and clarification of the needs, members of the partnership can agree on roles of the CBO and the resources to harness (Caldwell et al., 2015; Darling et al., 2015; Goytia et al., 2013; Kakietek et al., 2013; Kelaher et al., 2014; Panapasa et al., 2012). During this process, the set goals and roles are matched with the resources of the CBOs and members of the partnership. In line with this, there should be a clear plan and consensus on how resources will be allocated to address the identified needs (Caldwell et al., 2015; Darling et al., 2015; Goytia et al., 2013; Kakietek et al., 2013; Kelaher et al., 2014; Panapasa et al., 2012). This will avoid mismanagement of resources that could potentially affect engagement. Effective engagement occurs when CBOs can dedicate available resources in the ways that benefit a partnership without strains that could negatively impact the CBO or the partnership (Chaskin et al., 2006). For example, a CBO with limited human resources put in charge of data collection will experience difficulties stretching the duties of their staff, leading to delays in data collection and poor obtained results (Chaskin et al., 2006). In the event of a disparity between the resources and needs that cannot be addressed, the need for the partnership should be reassessed to avoid low engagement.
Power imbalance has been identified as a deterrent to engagement as it influences the relationship dynamics between CBOs and scientific/academic institutions (Bloom et al., 2009). Researchers should ensure that CBOs are treated as full partners emphasising the importance of every assigned role, with fair or equal remuneration given where appropriate (Bloom et al., 2009; Caldwell et al., 2015). Communication is also a vital part of the process of engagement (Akintobi et al., 2012; Caldwell et al., 2015). Communication should be open and regular, allowing for contributions from the CBO which should also be accounted for the decisions and actions of the project (Bloom et al., 2009; Darling et al., 2015; Glik et al., 2014; Napoles et al., 2014). Communication and meetings should also be realistic based on the situations of the CBOs involved (Glik et al., 2014; Honeycutt et al., 2015). For example, a CBO that is located far from a research institution should not be required to make long transits for frequent meetings without adequate resources. Regular meetings allow for needs to be reassessed, engagement to be evaluated and concerns to be addressed (Collignon et al., 2001; Darling et al., 2015; Honeycutt et al., 2015). CBOs should be trusted and trust members of the partnership; this is fuelled by communication and the absence of power differences (Akintobi et al., 2012; Bloom et al., 2009; Caldwell et al., 2015; Laborde et al., 2007; Taras et al., 2015). In ensuring good partnership dynamics, conflicts should be recognised as inevitable, and a plan should be in place for its resolution (Bloom et al., 2009).
The outcome of CBOE is important to evaluate the goals of both the partnership and the proposed project. Researchers and members of a partnership should evaluate that the identified needs and goals of the partnership were addressed during or at the end of the partnership (Akintobi et al., 2012; Honeycutt et al., 2015). Effective engagement meets the needs of the community the partnership sets out to serve (Caldwell et al., 2015; Johnson et al., 2006; Kakietek et al., 2013; LoConte et al., 2013; Riehman et al., 2013). Engagement of CBOs also leads to improvement in the knowledge and skills of the CBO and equips them to better serve their community or for future partnerships (Bloom et al., 2009; Collignon et al., 2001; Houston et al., 2002). Researchers should assess that CBOs identify benefits from engaging in the partnership. In facilitating engagement, the needs of a partnership should influence the goals of the proposed projects and the resources used; partnership dynamics should encourage the relationships between the CBOs and partnership members; and the outcome should reflect the set goals, available resources, and partnership dynamics of the CBO and partnership.
CBOE can be instrumental in reducing and mitigating the barriers to CBPR. Some noted barriers to CBPR like poor or ineffective communication, power imbalance, absence of trust, lack or inefficient use of resources and disagreement on research or partnership goals are addressed in the components of CBOE (Akintobi et al., 2012; Bloom et al., 2009; Caldwell et al., 2015; Darling et al., 2015; Fitzpatrick, 2016; Honeycutt et al., 2015; Johnson et al., 2006; Jurkowski & Manganello, 2016; Katigbak et al., 2016; Kelaher et al., 2014; McDonald & Stack, 2016; Napoles et al., 2014; Singer et al., 2015). Focusing on CBOE in research partnerships can facilitate CBPR and the benefits it brings to target communities, including reduced health disparities, and creation and implementation of interventions (Bloom et al., 2009; Boutain & McNees, 2013; Burkhalter et al., 2013; Kakietek et al., 2013; LoConte et al., 2013; Riehman et al., 2013). The results of this review will encourage future successful implementations of CBPR.
This analysis can assist healthcare researchers in planning partnerships with CBOs, and making necessary adjustments to improve study outcomes. Appropriate application of the components of CBOE in partnerships will assist researchers in addressing health disparities. This review also provides a foundation for developing a measure for CBOE. The different conceptualisations of “community” have led to a variation in tools used to assess community engagement. There is also a paucity of standardised instruments to measure community engagement. The findings from this study have delineated the important components of CBOE and therefore form the basis of the development of a standardised tool to measure CBOE. A measure that accounts for the need, partnership dynamics, resources and outcomes of the engagement of CBOs will show the level of engagement and point out areas of weaknesses that researchers can pay attention to. A measure that evaluates CBOE can be used to appraise different levels of engagement and evaluate the impact of the differences on study outcomes.
Although the effectiveness of CBPR and the use of CBOs for research has been documented in the literature, there is a paucity in research that evaluates how best to engage CBOs. Most of the literature on engagement evaluates engagement of study participants or community members (Blakeney et al., 2015; Clinical and Translational Science Awards Consortium, 2011; Drake & Whitley, 2014; Patel et al., 2011). Although the studies in this review identified major components of CBOE, only a few of them specifically examined engagement of CBOs as an outcome (Akintobi et al., 2012; Bloom et al., 2009; Boutain & McNees, 2013; Kakietek et al., 2013). More research is needed to further understand CBOE and how it influences research partnerships.
There are some limitations to this review. First, the systematic literature search and title/abstract review was conducted by one author. This could lead to an inadvertent omission or misrepresentation of literature. Furthermore, reviewed literature was limited to peer-reviewed publications in English language. This could also lead to omission of literatures in other databases, grey literature or publications that are not in English language. Additionally, our review aimed at identifying salient themes peculiar to organisational structures with the hope of improving research partnerships and their effects research. Hence, the differences in cultures and societies that could be reflected in CBOs were out of our scope and would benefit from future research to address this gap. The studies in this review were included irrespective of their appraisal score; hence, there might be some weak findings that were included as reflected by the appraisal scores. Additionally, this review describes and discusses the components of CBOE, it is not yet known in what way CBOE impacts community health exactly, and this is something that warrants further attention in the future. Although there were limitations, the large amount of literature in this review reduces the impacts of misrepresentations and omissions. Data abstraction and appraisal by multiple authors increase the credibility and validity of the findings.
5 |. CONCLUSION
CBOs continue to be very instrumental in research. The unique abilities of CBOs to represent vulnerable populations and hard-to-reach groups increase the effectiveness of translational research; lead to the development of timely and specific interventions; and most importantly address health disparities. Engagement of CBOs strengthens partnerships and increases the effectiveness of research collaborations. The findings from this review form the basis for understanding the meaning of CBOE, measurement of CBOE and future studies on CBOE. The identification of these components will assist researchers and CBOs in evaluating engagement in research partnerships, and aid in the making adjustments that could potentially improve CBOE. The review also provides a foundation for future research in applying CBOE to translational research and interventions. Knowledge of CBOE components will inform research, practice, policies and interventions that target CBPR and health disparities.
What is known about this topic
Community-based organisations (CBOs) are an important and necessary component for the success of community-based participatory research (CBPR) projects aiming to address health disparities.
Engagement of CBOs impacts outcomes in CBPR, but engagement is often conceptualised differently, and used limitedly in CBPR.
What constitutes engagement of CBOs is unclear and limits its proper application in CBPR, which may negatively impact community health.
What this paper adds
There are four main components of community-based organisation engagement (CBOE).
Applying components of CBOE will create, strengthen and sustain research partnerships with CBOs.
Stronger partnerships with CBOs will improve the quality and effects of CBPR and improve community health.
Acknowledgments
Funding information
Support for this research was received from the Center of Excellence for Health Disparities Research: El Centro, National Center on Minority Health and Health Disparities grant P60MD002266. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
CONFLICTS OF INTEREST
No conflicts of interest have been declared.
REFERENCES
- Akintobi TH, Yancey EM, Daniels P, Mayberry RM, Jacobs D, & Berry J (2012). Using evaluability assessment and evaluation capacity-building to strengthen community-based prevention initiatives. Journal of Health Care for the Poor and Underserved, 23(2 Suppl), 33–48. 10.1353/hpu.2012.0077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakeney N, Michaels M, Green M, Richmond A, Long D, Robinson WS, …Corbie-Smith G (2015). Collaborative development of clinical trials education programs for African-American community-based organizations. Journal of Cancer Education, 30, 400–406. 10.1007/s13187-014-0673-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom T, Wagman J, Hernandez R, Yragui N, Hernandez-Valdovinos N, Dahlstrom M, & Glass N (2009). Partnering with community-based organizations to reduce intimate partner violence. Hispanic Journal of Behavioral Sciences, 31, 244–257. [Google Scholar]
- Boutain DM, & McNees M (2013). Initiating policy, systems, and environmental changes for childhood obesity prevention by engaging six faith-based organizations. Family & Community Health, 36, 248–259. 10.1097/FCH.0b013e31829315b1 [DOI] [PubMed] [Google Scholar]
- Burkhalter JE, Cahill S, Shuk E, Guidry J, Corner G, Berk A, … Lubetkin EI(2013). At the intersection of HIV/AIDS and cancer: A qualitative needs assessment of community-based HIV/AIDS service organizations. Health Education & Behavior, 40, 493–503. 10.1177/1090198112459049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell WB, Reyes AG, Rowe Z, Weinert J, & Israel BA (2015). Community partner perspectives on benefits, challenges, facilitating factors, and lessons learned from community-based participatory research partnerships in Detroit. Progress in Community Health Partnerships, 9, 299–311. 10.1353/cpr.2015.0031 [DOI] [PubMed] [Google Scholar]
- Center for Evidence-Based Medicine (CEBM) Critical Appraisal of a Case Study. (2017). Retrieved from https://www.cebma.org/wp-content/uploads/Critical-Appraisal-Questions-for-a-Case-Study.pdf
- Chandra A, Williams M, Plough A, Stayton A, Wells KB, Horta M, & Tang J (2013). Getting actionable about community resilience: The Los Angeles County Community Disaster Resilience project. American Journal of Public Health, 103, 1181–1189. 10.2105/ajph.2013.301270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaskin RJ, Goerge RM, Skyles A, & Guiltinan S (2006). Measuring social capital: An exploration in community-research partnership. Journal of Community Psychology, 34, 489–514. [Google Scholar]
- Clinical and Translational Science Awards Consortium (2011). Principles of Community Engagement (2nd ed.). Bethesda, MD: U.S. Department of Health and Human Services. [Google Scholar]
- Collignon FF, Men M, & Tan S (2001). Finding ways in: Community-based perspectives on Southeast Asian family involvement with schools in a New England state. Journal of Education for Students Placed at Risk, 6, 27–44. [Google Scholar]
- Critical Appraisal Skills Programme [CASP]. (2013). Retrieved from http://www.casp-uk.net/casp-tools-checklists
- Darling M, Gonzalez F, Graves K, Sheppard VB, Hurtado-de-Mendoza A, Leventhal KG, & Caicedo L (2015). Practical tips for establishing partnerships with academic researchers: A resource guide for community-based organizations. Progress in Community Health Partnerships, 9, 203–212. 10.1353/cpr.2015.0042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake RE, & Whitley R (2014). Recovery and severe mental illness: Description and analysis. Canadian Journal of Psychiatry, 59, 236–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faridi Z, Grunbaum JA, Gray BS, Franks A, & Simoes E (2007). Community-based participatory research: Necessary next steps. Preventing Chronic Disease, 4, A70. [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick JJ (2016). Community-based participatory research: Challenges and opportunities. Applied Nursing Research, 31, 187 10.1016/j.apnr.2016.06.005 [DOI] [PubMed] [Google Scholar]
- Frew PM, Saint-Victor DS, Isaacs MB, Kim S, Swamy GK, Sheffield JS, … Ault K (2014). Recruitment and retention of pregnant women into clinical research trials: An overview of challenges, facilitators, and best practices. Clinical Infectious Diseases, 59(Suppl 7), S400–S407. 10.1093/cid/ciu726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gainforth H, Latimer-Cheung A, Moore S, Athanasopoulos P, & Martin Ginis K (2015). Using network analysis to understand knowledge mobilization in a community-based organization. International Journal of Behavioral Medicine, 22, 292–300. 10.1007/s12529-014-9430-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geist MR (2010). Using the Delphi method to engage stakeholders: A comparison of two studies. Evaluation and Program Planning, 33, 147–154. 10.1016/j.evalprogplan.2009.06.006 [DOI] [PubMed] [Google Scholar]
- Glik DC, Eisenman DP, Donatello I, Afifi A, Stajura M, Prelip ML, … Martel A (2014). Reliability and validity of the Assessment for Disaster Engagement with Partners Tool (ADEPT) for local health departments. Public Health Reports, 129(Suppl 4), 77–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goytia CN, Todaro-Rivera L, Brenner B, Shepard P, Piedras V, & Horowitz C (2013). Community capacity building: A collaborative approach to designing a training and education model. Progress in Community Health Partnerships, 7, 291–299. 10.1353/cpr.2013.0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honeycutt S, Leeman J, McCarthy WJ, Bastani R, Carter-Edwards L, Clark H, … Kegler M (2015). Evaluating policy, systems, and environmental change interventions: Lessons learned from CDC’s prevention research centers. Preventing Chronic Disease, 12, E174 10.5888/pcd12.150281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston HR, Harada N, & Makinodan T (2002). Development of a culturally sensitive educational intervention program to reduce the high incidence of tuberculosis among foreign-born Vietnamese. Ethnicity & Health, 7, 255–265. 10.1080/1355785022000060718 [DOI] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, & Becker AB (1998). Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health, 19, 173–202. 10.1146/annurev.publhealth.19.1.173 [DOI] [PubMed] [Google Scholar]
- Jewett-Tennant J, Collins C, Matloub J, Patrick A, Chupp M, Werner JJ, & Borawski EA (2016). Partnership among peers: Lessons learned from the development of a community organization-academic research training program. Progress in Community Health Partnerships: Research, Education, and Action, 10, 461–470. 10.1353/cpr.2016.0052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson HH, Bobbitt-Cooke M, Schwarz M, & White D (2006). Creative partnerships for community health improvement: A qualitative evaluation of the Healthy Carolinians community micro-grant project. Health Promotion Practice, 7, 162–169. 10.1177/1524839905278898 [DOI] [PubMed] [Google Scholar]
- Jurkowski JM, & Manganello JA (2016). Using a CBPR Approach with Health Literacy Research for Community or Patient Stakeholder Engagement Presentation. Health Policy, Management & Behavior - School of Public Health, University at Albany. [Google Scholar]
- Kakietek J, Geberselassie T, Manteuffel B, Ogungbemi K, Krivelyova A, Bausch S, … Gar S(2013). It takes a village: Community-based organizations and the availability and utilization of HIV/AIDS-related services in Nigeria. AIDS Care, 25(Suppl 1), S78–S87. 10.1080/09540121.2012.740158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katigbak C, Foley M, Robert L, & Hutchinson MK (2016). Experiences and lessons learned in using community-based participatory research to recruit Asian American immigrant research participants. Journal of Nursing Scholarship, 48, 210–218. 10.1111/jnu.12194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelaher M, Sabanovic H, La Brooy C, Lock M, Lusher D, & Brown L (2014). Does more equitable governance lead to more equitable health care? A case study based on the implementation of health reform in Aboriginal health Australia. Social Science and Medicine, 123, 278–286. 10.1016/j.socscimed.2014.07.032 [DOI] [PubMed] [Google Scholar]
- Laborde DJ, Brannock K, Breland-Noble A, & Parrish T (2007). Pilot test of cooperative learning format for training mental health researchers and black community leaders in partnership skills. Journal of the National Medical Association, 99, 1359–1368. [PMC free article] [PubMed] [Google Scholar]
- LoConte NK, Weeth-Feinstein L, Conlon A, & Scott S (2013). Engaging health systems to increase colorectal cancer screening: Community-clinical outreach in underserved areas of Wisconsin. Preventing Chronic Disease, 10, E192 10.5888/pcd10.130180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald KE, & Stack E (2016). You say you want a revolution: An empirical study of community-based participatory research with people with developmental disabilities. Disability and Health Journal, 9, 201–207. 10.1016/j.dhjo.2015.12.006 [DOI] [PubMed] [Google Scholar]
- McFarlane E, Kahili A, & Johnson JA (2014). Insights in public health: Bridging the research to practice gap to prevent maternal stress and depression. Hawai’i Journal of Medicine & Public Health, 73, 195–196. [PMC free article] [PubMed] [Google Scholar]
- Minkler M, Wallerstein N, & The PRISMA Group. (2008). Community-based participatory research for health: From process to outcomes. Hoboken, NJ: Jossey-Bass. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6, e1000097 10.1371/jour-nal.pmed1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napoles AM, Santoyo-Olsson J, Ortiz C, Gregorich S, Lee HE, Duron Y, ... Stewart AL (2014). Randomized controlled trial of Nuevo Amanecer: A peer-delivered stress management intervention for Spanish-speaking Latinas with breast cancer. Clinical Trials, 11, 230–238. 10.1177/1740774514521906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Network of Libraries of Medicine. (2015). Community based organization defined.
- Panapasa S, Jackson J, Caldwell C, Heeringa S, McNally J, Williams D, … Fa’asisila S(2012). Community-based participatory research approach to evidence-based research: Lessons from the Pacific Islander American Health Study. Progress in Community Health Partnerships, 6, 53–58. 10.1353/cpr.2012.0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Collins PY, Copeland J, Kakuma R, Katontoka S, Lamichhane J, .. Skeen S (2011). The movement for global mental health. British Journal of Psychiatry, 198, 88–90. 10.1192/bjp.bp.109.074518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson L, Morzinski J, Ertl K, Wurm C, Hayes A, & Whittle J (2011). Engaging community-based veterans’ organizations in health promotion programs. Family & Community Health, 34, 311–318. 10.1097/FCH.0b013e31822b5425 [DOI] [PubMed] [Google Scholar]
- Pluye P, Robert E, Cargo M, Bartlett G, O’Cathain A, Griffiths F, ... Rousseau MC. (2011). Proposal: A mixed methods appraisal tool for systematic mixed studies. Retrieved from http://mixedmethodsapprais-altoolpublic.pbworks.com
- Radermacher H, Karunarathna Y, Grace N, & Feldman S (2011). Partner or perish? Exploring inter-organisational partnerships in the multicultural community aged care sector. Health and Social Care in the Community, 19, 550–560. 10.1111/j.1365-2524.2011.01007.x [DOI] [PubMed] [Google Scholar]
- Riehman KS, Kakietek J, Manteuffel BA, Rodriguez-Garcia R, Bonnel R, N’Jie N, Fruh J (2013). Evaluating the effects of community-based organization engagement on HIV and AIDS-related risk behavior in Kenya. AIDS Care, 25(Suppl 1), S67–S77. 10.1080/09540121.2013.778383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roush S, Monica C, Pavlovich D, & Drake RE (2015). Community engagement research and dual diagnosis anonymous. Journal of Dual Diagnosis, 11, 142–144. 10.1080/15504263.2015.1025214 [DOI] [PubMed] [Google Scholar]
- Singer J, Bennett-Levy J, & Rotumah D (2015). “You didn’t just consult community, you involved us”: Transformation of a ‘top-down’ Aboriginal mental health project into a ‘bottom-up’ community-driven process. Australasian Psychiatry, 23, 614–619. 10.1177/1039856215614985 [DOI] [PubMed] [Google Scholar]
- Tait L, Birchwood M, & Trower P (2002). A new scale (SES) to measure engagement with community mental health services. Journal of Mental Health, 11,191–198. 10.1080/09638230020023570-2 [DOI] [PubMed] [Google Scholar]
- Taras HL, Kalichman MW, Schulteis G, Dumbauld J, Bell Y, Seligman FF, & West KD (2015). Soliciting views of various communities on health research: A prelude to engagement in specific research projects. Health Expectations, 18, 2753–2763. 10.1111/hex.12249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tisnado D, Sablan-Santos L, Guevara L, Quitugua L, Castro K, Aromin J, … Tran J (2010). A case study in Chamorro community and academic engagement for a community-partnered research approach. Californian Journal of Health Promotion, 8, 39–51. [PMC free article] [PubMed] [Google Scholar]
- Woodruff RC, Coleman A, Hermstad AK, Honeycutt S, Munoz J, Loh L, … Kegler MC (2016). Increasing community access to fresh fruits and vegetables: A case study of the farm fresh market pilot program in Cobb County, Georgia, 2014. Preventing Chronic Disease, 13, 1–10. 10.5888/pcd13.150442 [DOI] [PMC free article] [PubMed] [Google Scholar]