Abstract
Introduction
Hospital-acquired infections of Lassa fever (LF) have been described in many West African countries. We assessed the availability of Infection Prevention and Control (IPC) measures and their use in the health centres (HCs) at the affected Local Government Areas (LGAs) during an ongoing LF outbreak in Ondo State, Nigeria.
Methods
We included all primary and secondary HCs and their healthcare workers (HCWs) in the affected Ose and Owo LGAs. We collected data from respondents using self-administered questionnaires and used a checklist to assess the IPC measures at the HCs. We generated frequencies and proportions and tested associations using odds ratios at 95% CI.
Results
One hundred and ninety HCWs from 59 HCs were surveyed of which 34 (57.6%) were located in Owo LGA. All HCs had soap for handwashing, 57(96.6%) had wash-hand basins but only 52(88.1%) had water. While 57(96.6%) had gloves and 53(89.8%) had sharps boxes, only 16(27.1%) had an isolation room. Only 44(23.2%) respondents had been trained in IPC. The majority, 144 (91.6%) always had gloves available for their use, 79(41.6%) always had facemask/shield and 71(37.4%) always had full personal protective equipment. At the last patient contact, only 151 (79.8%) washed their hands before the contact, 188(98.9%) washed their hands after and 183 (96.2%) wore gloves. While there was no association between availability of gloves and its use (OR: 0.21, 95%CI 0.04-1.17), there was significant association between having had training in basic universal precautions and having used gloves (OR: 3.64, 95%CI 1.21-19.40) and having washed hands after last patient contact (OR: 2.31, 95%CI 1.67-12.30).
Conclusion
Among these HCs that serve as point of first contact with possible cases of LF in these endemic LGAs, none met the minimum standard for IPC. We recommend that IPC committee for each LGA and the whole state should be set up and IPC trainings made mandatory.
Keywords: Lassa fever, infection prevention and control, health centres, health care workers
Introduction
Lassa fever is a zoonotic disease caused by an arenavirus, the lassa virus, so named after the town in Nigeria where it was first isolated [1]. Humans contract the virus primarily through contact with the contaminated excreta of Mastomys natalensis rodents (commonly known as the Multimammate rat), which is the natural reservoir for the virus. The infected rodents are reservoirs capable of excreting the virus through urine, saliva, excreta and other body fluids to man [2]. Secondary transmission of the virus between humans occurs through direct contact with infected blood or bodily secretions. This occurs mainly between individuals caring for sick patients although anyone who comes into close contact with a person carrying the virus is at risk of infection. Incubation period of Lassa fever is 1-3 weeks. It presents with symptoms and signs indistinguishable from those of febrile illnesses such as malaria and other viral haemorrhagic fevers such as Ebola. In approximately 80%, symptoms are mild and are often undiagnosed. Death may occur within two weeks after symptom onset due to multi-organ failure [3]. While approximately 15%-20% of patients hospitalized for Lassa fever die from the illness, only 1% of all lassa virus infections result in death [4].
Nosocomial transmission of Lassa fever in healthcare facilities represent a significant burden on the healthcare system [5]. Infection prevention and control (IPC) in healthcare settings has been documented as an important factor in controlling potential outbreaks of Lassa fever [6]. In support of this, studies have shown that in hospitals with improved IPC practices, transmission of Lassa virus was minimal [7,8]. Lassa fever is endemic in parts of West Africa including Sierra Leone, Liberia and Nigeria; affecting about 100,000 to 300,000 people every year in this regions [9, 10]. There have been several Lassa fever outbreaks in various parts of Nigeria since it was first reported in 1969. The worst outbreak was recorded in 2012 when 623 cases including 70 deaths were reported from 19 out of the 36 states. Three doctors and four nurses were reported to be among the fatalities [11]. Between August 2015 and 17 May 2016, WHO was notified of 273 cases of Lassa fever reported from 23 states in Nigeria; these included 149 deaths. Of these, ten cases were health care workers (HCWs) and four were hospital acquired infections [11]. Many Local Government Areas in Ondo State have yearly outbreaks of Lassa fever which often affect health workers who are particularly at risk in resource poor settings like Nigeria due to lack of availability and use of IPC materials. Conscientious use of IPC during patient care irrespective of diagnosis and the use of transmission specific IPC materials when caring for patients with Lassa fever reduces the risk of hospital based transmission. The aim of this study was to assess the knowledge of Lassa fever among health care workers, availability of infection prevention and control measures and their use during Lassa fever outbreak in Ondo State.
Methods
Study design: We conducted a descriptive cross sectional study among HCWs in Owo and Ose LGAs.
Study area: We purposively selected Owo and Ose LGAs because they were experiencing an outbreak at the time of this study. The two LGAs are the boundaries of the State with neighbouring Edo State which is known to be endemic for Lassa fever. Ondo state, with Akure as the capital, consists of 18 LGAs. The population was 3,441,024 as at 2006 census. Majority of the state´s citizens live in urban centers [12].
Study population: We carried out the study among HCWs who had been working in either secondary or primary health centers in the selected LGAs for at least six months prior to the commencement of our study.
Sampling: We did a total sampling of all primary and secondary health centers (both government and private owned) and their HCWs in the selected LGAs.
Data collection: We administered semi-structured interviewer administered questionnaire to the HCWs to assess their knowledge on Lassa and their practice of IPC. We used a checklist to assess the availability of infection prevention and control measures in the Health centers.
Data management: Data was entered and analyzed using Statistical Package for Social Sciences version (SPSS) 23 and Microsoft Excel 2016 software. Results were presented in frequencies, means and proportions. Each rightly answered question on knowledge was scored one and wrong answers scored zero. The scores were summed, seventy percent (70%) of the total score was used as the cut off between good and poor knowledge. Maximum achievable score for knowledge on epidemiological features of Lassa fever among all respondents was 11 and minimum zero. Maximum achievable score on knowledge of the clinical features of Lassa fever was 15 and minimum zero. Maximum achievable score for knowledge of precautions to be taken while caring for Lassa patients was eight and minimum zero. Associations between knowledge and availability of measures and practice were tested using chi square or Fishers test, where appropriate, with the level of significance set at 5%.
Ethical considerations: We obtained ethical approval from the Ondo State Hospital Management Board Ethical Review Board. We obtained informed consent from the respondents. We made them to understand that participation was voluntary and there was no consequence for non-participation. All information obtained were kept confidential.
Results
Fifty-nine health facilities and one hundred and ninety healthcare workers were surveyed. Of the 59 health facilities surveyed, 9 (15.3%) were secondary health facilities the rest were primary. Of the 190 healthcare workers, 144 (75.8%) worked at primary health facilities while 155 (81.6%) worked at Government-owned facilities (Table 1).
Table 1.
Sociodemographic characteristics of respondents, Ose and Owo LGAs, Ondo State, 2016
| Sociodemographic characteristics | Ose (n=74) | % | Owo (n=116) | % | Total (N= 190) | % |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 16 | 21.6 | 19 | 16.4 | 35 | 18.4 |
| Female | 58 | 78.4 | 97 | 83.6 | 155 | 81.6 |
| Mean age (in years) | 28.8(±9.0) | 33.7(±10.7) | 31.8 (10.3) | |||
| Religion | ||||||
| Christianity | 65 | 87.8 | 109 | 88.8 | 174 | 91.6 |
| Islam | 9 | 12.2 | 7 | 6.0 | 16 | 8.4 |
| Ethnicity | ||||||
| Yoruba | 68 | 91.9 | 103 | 88.8 | 171 | 90.0 |
| Others# | 6 | 8.1 | 13 | 11.2 | 19 | 10.0 |
| Profession | ||||||
| Doctor | 0 | 0 | 1 | 0.9 | 1 | 0.5 |
| Registered nurse | 12 | 16.2 | 21 | 18.1 | 33 | 17.4 |
| Community Health worker | 41 | 55.4 | 55 | 47.4 | 96 | 50.5 |
| Auxiliary nurses | 11 | 14.9 | 13 | 11.2 | 24 | 12.6 |
| Health assistants | 5 | 6.7 | 9 | 7.7 | 14 | 7.4 |
| Others* | 5 | 6.8 | 17 | 14.7 | 22 | 11.6 |
| Facility ownership | ||||||
| Government owned | 59 | 79.7 | 96 | 82.8 | 155 | 81.6 |
| Private owned | 15 | 20.3 | 20 | 17.2 | 35 | 18.4 |
| Facility tier | ||||||
| Secondary | 20 | 27.0 | 26 | 22.4 | 46 | 24.2 |
| Primary | 54 | 73.0 | 90 | 77.6 | 144 | 75.8 |
Ibo and Edo
Pharmacists and Laboratory scientists and technicians
Healthcare workers
Of 190 respondents, 44 (23.2%) worked at Ose LGA and 35 (18.4%) were males. Mean age was 31.8±10.3 years. They were mostly Christians (174, 91.6%) and mainly Yoruba (171, 90%). Half (96, 50.5%) of them were Community Health Workers, 33 (17.4%) were registered nurses, 24 (12.6%) were auxiliary nurses or auxiliary trainee nurses and 1 (0.5%) was a doctor (Table 1). Among the respondents, only 44 (23.2%) have had a training in infection prevention and control (IPC).
Overall knowledge
The overall knowledge score achieved by all respondents was 24.3±4.0. Less than half, 79 (41.6%) of respondents had good overall knowledge of Lassa fever epidemiology, clinical features and precautions to be taken in caring for affected patients. Registered nurses had better knowledge compared to auxiliary nurses/trainees (OR: 10, 95% CI: 5.06-15.0), Health Assistants (OR: 5, 95%CI: 1.27-19.6), Community Health Workers (OR: 2.5, 95% CI: 1.07-5.6), and other cadres of health workers (OR: 5.6, 95%CI: 2.74-12.5). Those that have had training in IPC had better knowledge than those who had not (OR: 3.9, 95% CI: 1.8-8.2).
Knowledge of epidemiology of Lassa fever
The mean score on knowledge of epidemiology of Lassa fever among all respondents was 6.8 (±1.5). There was a statistically significant difference between the mean score among respondents from government owned facilities (mean score = 6.9 ±1.3) and private (mean score = 6.2 ±2.2) (p = 0.015). Only 26.8% had good knowledge and there was no statistically significant relationship with profession (p=0.325), facility ownership (p = 0.474) and LGA (p=0.413) (Figure 1).
Figure 1.
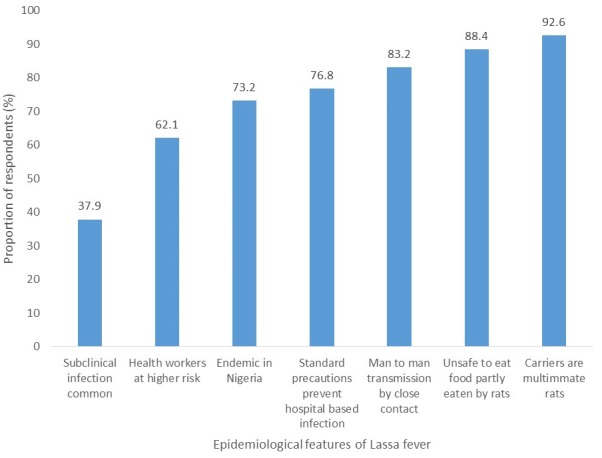
Proportion of HCWs that correctly identified each of the epidemiological features of LF, Ose and Owo LGA, Ondo State, 2016
Knowledge of clinical features
The mean score achieved by all respondents was 11.4±2.4. There was a statistically significant difference between the mean score among respondents in government facilities (11.6±2.1) and private (10.4±3.2) (p = 0.009). Only 100 (52.6%) of all respondents had good knowledge of clinical features (Figure 2). There was a statistically significant relationship with LGA (p = 0.002). Majority (125, 65.8%) knew it was not 100 % fatal while about a third (58, 30.5%) knew deafness was a sequela.
Figure 2.
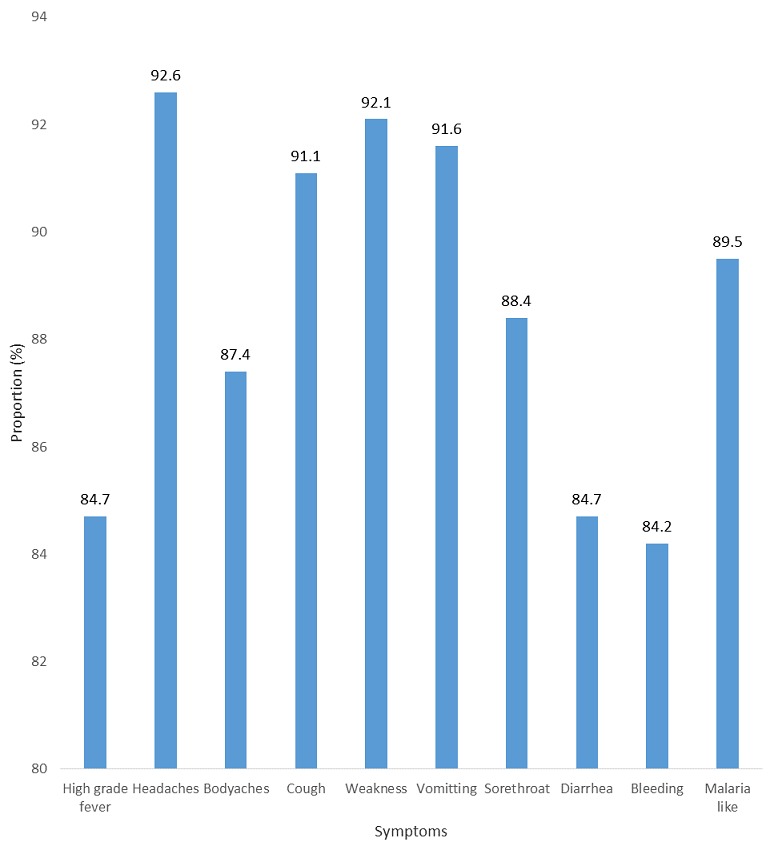
Proportion of HCWs that correctly identified each symptom of LF, Ose and Owo LGAs, Ondo state, 2016
Knowledge of precautionary measures (Figure 3)
Figure 3.
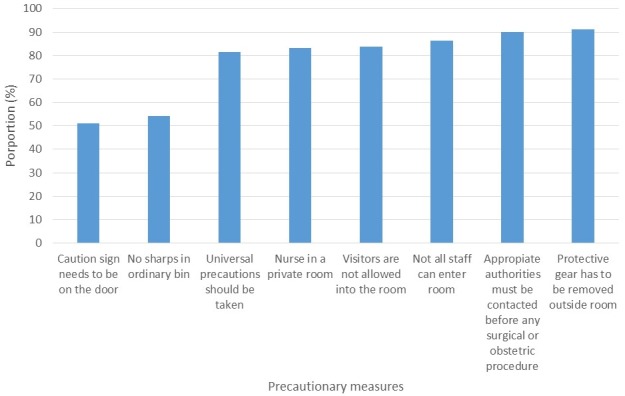
Proportion of HCWs who recognized appropriate precautionary measures to be taken while caring for a LF patient, Ose and Owo LGAs, 2016
Mean knowledge score achieved by all respondents was 6.2 ±1.6. There was a significant association between mean knowledge scores of respondents from government facilities (mean score=6.4±1.4) and those from private (mean score= 5.5±1.6), (p=0.03).
Availability of Personal Protective Equipment (PPEs) at work place
In all, 174 (91.6%), always had gloves available for their use, 79 (41.6%) always had facemask/shield always available, and less than a third, 56 (29.5%), always had googles available. About two-thirds, 129 (67.9%), always had apron available and almost half 94 (49.5%) always had boots available, while 71 (37.4%) always had full body PPE available (Figure 4).
Figure 4.
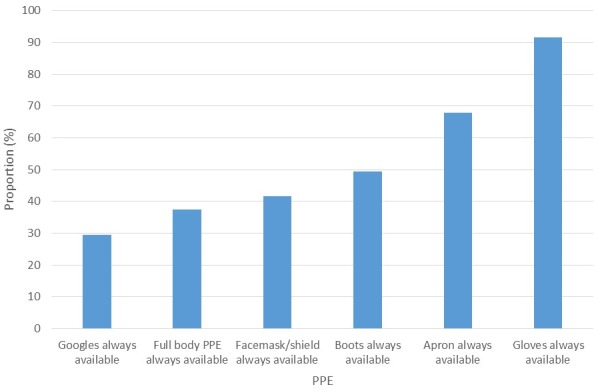
Availability of PPEs to HCWs, Ose and Owo LGAs Ondo state, 2016
Practice of basic universal precautions
About 183 (96.3%) reported that they routinely used gloves when handling body secretions and contaminated items while, 171 (90.5%) reported that they routinely washed hands before and after all procedures. Only 86.3% routinely disposed all sharps into sharps bin. Sixty percent of respondents routinely used gown and boots during a procedure likely to generate splashes while 116 (61.1%) routinely used facemask and eye protection during such procedures as well. At the last patient contact, only 152 (79.8%) washed their hands before the contact, 188 (98.9 %) washed their hands after and 183 (96.2%) wore gloves (Figure 5). While there was no association between availability of gloves and its use (OR: 0.21, 95%CI: 0.04-1.17), health workers who have had a training in IPC were more likely to have used gloves at the last patient contact (OR: 3.64, 95%CI 1.21-19.40) and they were also more likely to have washed their hands at the last patient contact (OR: 2.31, 95%CI 1.67-12.30).
Figure 5.
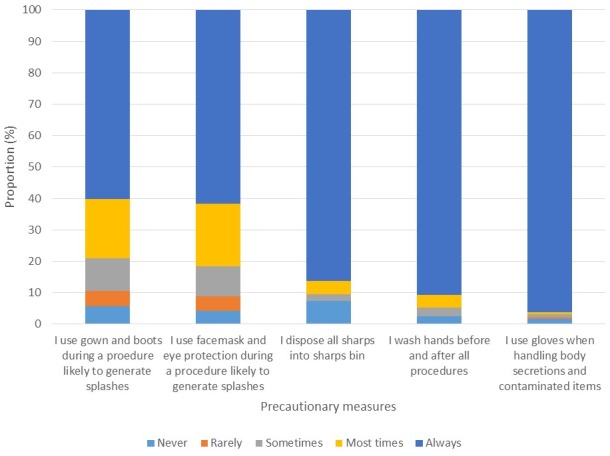
Use of precautionary measures during patient care by HCW in Owo and Ose LGAs, Ondo state, 2016
Health facilities
All 59 had soap for hand-washing, but 7 (11.9%) didn’t have water out of which 6 (85.7%) were government-owned facilities and all were primary facilities. Wash-hand basin was available in 57 (96.6%) and 52 (88.1%) had water available. Two (3.4%) of the facilities didn’t have gloves. Only 20 (33.9%) had chlorine solution, 52 (87.2%) of these were government-owned facilities and primary facilities respectively. No health facility had all Infection Prevention and Control (IPC) requirements (Table 2).
Table 2.
Facility ownership of IPC measures by facility tier, Ondo State, 2016
| Characteristic | Secondary N=9 | % | Primary N=50 | % | Fishers P Value |
|---|---|---|---|---|---|
| Had isolation ward or room | 4 | 44.4 | 12 | 24.0 | 0.236 |
| Had changing room | 7 | 77.8 | 29 | 58.0 | 0.460 |
| Had restricted access room | 4 | 44.4 | 10 | 20.0 | 0.195 |
| Had soap for hand-washing | 9 | 100 | 43 | 86.0 | N/A |
| Had water | 9 | 100 | 48 | 96.0 | 0.581 |
| Had wash hand basin present | 9 | 100 | 44 | 88.0 | 1.000 |
| Had sharps box | 9 | 100 | 16 | 32.0 | 0.577 |
| Had chlorine solution | 4 | 44.4 | 48 | 96.0 | 1.477 |
| Had gloves | 9 | 100 | 48 | 96.0 | 1.000 |
| Had face shield or goggles | 9 | 100 | 33 | 66.0 | 0.471 |
| Had apron | 9 | 100 | 12 | 24.0 | 0.480 |
| Had full body PPE | 3 | 33.3 | 25 | 50.0 | 0.680 |
| Had boots | 6 | 66.7 | 38 | 76.0 | 0.477 |
| Had red color-coded waste bin | 4 | 44.4 | 34 | 68.0 | 0.103 |
| Had black color-coded waste bin | 5 | 55.6 | 28 | 56.0 | 0.471 |
| Had yellow color-coded waste bin | 2 | 22.2 | 23 | 67.6 | 0.800 |
Discussion
General knowledge of Lassa fever was low among health workers in the Lassa fever endemic LGAs under study. Particularly, the knowledge of the clinical features of the disease was low despite the fact that early diagnosis and treatment with ribavirin contributes significantly to survival from Lassa fever [9]. This could mean that even if patients with Lassa fever present early at health facilities, they may not be diagnosed and receive appropriate treatment on time. This finding of low knowledge of Lassa fever is in contrast to that of Omotowo et al and Adebayo et al, both of which were conducted among healthcare workers in tertiary facilities in Nigeria. The difference in the results however, maybe due to the fact that doctors and nurses constituted the majority of their respondents and the studies were conducted at tertiary health facilities that were specialised in caring for Lassa fever cases [13,14]. However, the study by Aigbiremolen which was conducted among staff of primary health facilities only and used 75% as a cut off, found that almost 80% of the respondents had good knowledge [15]. The same study found that Community Health Extension Workers (CHEWs) had poorer knowledge of Lassa fever than trained nurses as this study did [15]. Therefore, the low knowledge found in this study could also be due to the high proportion of CHEWs and trainee auxiliary nurses [16]. However, other studies have also documented poor knowledge among other cadres of health workers (16).
A similarly low knowledge was found by the study of Ekuma and Akpan which was conducted in a tertiary facility among medical students, interns and resident doctors in Uyo [17]. Therefore, it is also possible that other factors apart from profession and level of healthcare practice influence the acquisition of knowledge on Lassa fever. In addition, while a study by Olowookere et al found an association between ownership of health facility and knowledge of Lassa fever [18], we did not find a significant relationship. The study by Aigbiremolen did find that workers at private HCs had better knowledge than the workers at government owned PHCs though this relationship was also not significant [15]. Knowledge of precautionary measures was on the average and comparable with that of the findings of Izegbu et al in Lagos although there’s was conducted among laboratory staff only [19]. While the use of PPE was also comparable with that of the findings of Adebayo et al [14]. According to Adewuyi et al, the most dangerous exposure is parenteral and must be avoided through staff training [20]. Unfortunately, the result of the study shows that less than a quarter of the healthcare workers in these LGAs that are endemic for Lassa fever have had any training on IPC. Training of health workers on priority diseases is of importance [21]. The recommendation is for such patients to be treated in isolation rooms with adequate PPEs available at all times [22], our study found that none of the secondary health facilities had neither an isolation room nor have PPEs routinely available.
Concerning the routine practice of IPC measures, different studies have found varying levels of IPC practice in different parts of the country similar to what was found by this study [15, 23-27]. The consistent finding in all the study is that the practice of IPC was poor irrespective of the level of health facility. While it was not the focus of this study, it was however found that there was a lack of qualified health personnel at the primary and secondary health facilities that were studied. Community Health Workers (CHEWs) constituted majority of the workforce in the facilities. There was also a high proportion of auxiliary nurses/trainees. However in Nigeria, CHEWs are expected to predominantly be at the primary health care level [28,29], this is not supposed to be so at secondary health care level. This pattern seen here is probably because there is lack of incentives for qualified personnel to work at primary and secondary healthcare facilities especially those located in semi-rural or rural places. This further proves that we still have a mal-distribution of healthcare workers in the country [30]. A major limitation of this study was a probable high proportion of acceptable IPC practices among the respondents than usual as these were self-reported and thus prone to bias.
Conclusion
This study found that the knowledge of HCWs about Lassa fever, its management and the IPC practices at health facilities in the LGAs studied were still inadequate therefore putting the HCWs at risk of hospital based transmission of not only Lassa fever but other infections. Ondo State Government should ensure HCWs receive refresher training on IPC regularly, and also set up IPC committees in each LGA that will ensure all health facilities in the LGAs meet the necessary IPC requirements.
What is known about this topic
Hospital-acquired infections of Lassa fever has been described in many West African countries;
Nosocomial transmission and outbreaks in healthcare facilities in endemic areas represent a significant burden on the healthcare system;
Infection prevention and control (IPC) in healthcare settings is an important factor in controlling potential outbreaks of Lassa fever.
What this study adds
The knowledge of Lassa fever among health care workers;
Availability and use of infection prevention and control measures during Lassa fever outbreak in Ondo State, Nigeria.
Competing interests
The authors declare no competing interests.
Authors’ contributions
ITI, OSI, OA, IO and AA developed the concept note and participated in data collection. ITI and OSI analysed the data using the data analysis plan accepted by all authors. Draft manuscript was written by ITI. All authors read and approved the final manuscript.
References
- 1.Frame JD, Baldwin JM, Gocke DJ, Troup JM. “Lassa fever, a new virus disease of man from West Africa. I. clinical description and pathological findings. Am J Trop Med Hyg. 1970 Jul;19(4):670–6. doi: 10.4269/ajtmh.1970.19.670. [DOI] [PubMed] [Google Scholar]
- 2.Kennlyside RA, McCormick JB, Webb PA, Smith E, Elliot L, Johnson KM. Case-control study of Mastomys natalensis and humans in Lassa virus-infected households in Sierra Leone. Am J Trop Med Hyg. 1983 Jul;32(4):829–37. doi: 10.4269/ajtmh.1983.32.829. [DOI] [PubMed] [Google Scholar]
- 3.McCormick JB. Lassa fever. In: Saluzzo JF, Dodet B, editors. Emergence and Control of Rodent-borne Viral Diseases. Paris: Elsevier; 1999. pp. 177–795. [Google Scholar]
- 4.World Health Organisation Lassa fever. Accessed on 10th November 2016.
- 5.Viral Hemorrhagic Fever Consortium About Viral Hemorrhagic Fever Consortium. Accessed on 24th November 2016.
- 6.Ajayi NA, Nwigwe CG, Azuogu BN, Onyire BN, Nwonwu EU, Ogbonnaya LU, et al. Containing a Lassa fever epidemic in a resource-limited setting: outbreak description and lessons learned from Abakaliki, Nigeria (January-March 2012) Int J Infect Dis. 2013 Nov;17(11):e1011–6. doi: 10.1016/j.ijid.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Ijarotimi IT, Oladejo JA, Jegede O, Nasidi A. Lassa fever in the State Specialist Hospital Akure, Nigeria: Case report, Contact tracing and outcome of hospital contacts. International Journal of Infectious and Tropical Diseases. 2015;3(1):20–28. [Google Scholar]
- 8.Fisher-Hoch SP, Tomori O, Nasidi A, Perez-Oronz GI, Fakile Y, Hutwagner L. Review of cases of nosocomial Lassa fever in Nigeria: the high price of poor medical practice. BMJ. 1995 Sep 30;311(7009):857–9. doi: 10.1136/bmj.311.7009.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention Fact sheet: Lassa fever. 2015. Accessed January 2016.
- 10.Leparc-Goffart I, Emonet SF. An update on Lassa virus. Med Trop (Mars) 2011 Dec;71(6):541–5. [PubMed] [Google Scholar]
- 11.World Health Organisation Lassa fever in Nigeria. Accessed on 25th November 2016.
- 12.Ondo State Government Building Ondo State into a Hub of Investment Opportunities in West Africa. Accessed on 19th November 2016.
- 13.Omotowo Babatunde I, Eyisi IG, Obi IE, Agwu-Umahi RO. Assessment of knowledge, attitudes and practices regarding Lassa fever among healthcare workers in a tertiary hospital, Enugu, South-East, Nigeria: Implications for control. J Infect Dis Ther. 2016 [Google Scholar]
- 14.Adebayo D, Nwobi EA, Vincent T, Gonzalez JP. Response preparedness to Viral Hemorrhagic Fever in Nigeria: risk perception, attitude towards Lassa Fever. Epidemiology. 2015;5:199. [Google Scholar]
- 15.Aigbiremolen AO, Duru CB, Awunor NS, Abejegah C, Abah SO, Asogun AD. Knowledge and application of infectious disease control measures among primary care workers in Nigeria: the Lassa fever example. Int J Basic, Appl Innov Res. 2012;1(4):122–129. [Google Scholar]
- 16.Tobin EA, Asogun DA, Isah EC, Ugege OG, Ebhodaghe P. Assessment of knowledge and attitude towards Lassa fever among Primary care providers in an endemic suburban community of Edo state: implications for control. J Med Med Sci. 2013;4(8):311–318. [Google Scholar]
- 17.Ekuma Agantem E, Akpan Lassa fever and infection control: knowledge, attitudes and practice in a university teaching hospital in Uyo, Nigeria. Ibom Medical Journal. 2017;10:1. [Google Scholar]
- 18.Olowookere SA, Fatiregun AA, Gbolahan OO, Adepoju EG. Diagnostic proficiency and reporting of Lassa fever by physicians in Osun State of Nigeria. BMC Infect Dis. 2014 Jun 20;14:344. doi: 10.1186/1471-2334-14-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Izegbu MC, Amole OO, Ajayi GO. Attitudes, perception and practice of workers in laboratories in the two colleges of Medicine and their teaching hospitals in Lagos State, Nigeria as regards universal precaution measures. Biomedical Research. 2006;17(1):49–54. [Google Scholar]
- 20.Adewuyi GM, Fowotade A, Adewuyi BT. Lassa Fever: another infectious menace. African J Clin Exp Microbiol. 2009;10(3):144–55. [Google Scholar]
- 21.Olayinka Stephen Ilesanmi, Oluwafolakemi Mary Babasola. Clinician sensitization on integrated disease surveillance and response in Federal Medical : Centre Owo, Ondo State, Nigeria, 2016. Public Health of Indonesia. 2017 Jun;3(2):41–49. [Google Scholar]
- 22.Centers for Disease Control and Prevention and World Health Organization . Infection control for viral haemorrhagic fevers in the African Health Care Setting. Atlanta: Centers for Disease Control and Prevention; 1998. pp. 1–198. [Google Scholar]
- 23.Iliyasu G, Dayyab FM, Habib ZG, et al. Knowledge and practices of infection control among healthcare workers in a Tertiary Referral Center in North-Western Nigeria. Ann Afr Med. 2016 Jan-Mar;15(1):34–40. doi: 10.4103/1596-3519.161724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ogoina Dimie, Pondei Kemebradikumo, Adetunji Babatunde, Chima George, Isichei Christian, Gidado Sanusi. Knowledge, attitude and practice of standard precautions of infection control by hospital workers in two tertiary hospitals in Nigeria. J Infect Prev. 2015 Jan;16(1):16–22. doi: 10.1177/1757177414558957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osuala Eunice Ogonna, Oluwatosin Abimbola O. Infection control by nurses in selected hospitals in Anambra State, Nigeria. Tropical Journal of Medical Research. 2017;20(1):53–60. [Google Scholar]
- 26.Amoran O, Onwube O. Infection control and practice of standard precautions among healthcare workers in Northern Nigeria. J Glob Infect Dis. 2013 Oct;5(4):156–63. doi: 10.4103/0974-777X.122010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Isara AR, Ofili AN. Knowledge and practice of standard precautions among health care workers in the Federal Medical Centre, Asaba, Delta State, Nigeria. Niger Postgrad Med J. 2010 Sep;17(3):204–9. [PubMed] [Google Scholar]
- 28.Herman AA. Community health workers and integrated primary health care teams in the 21st century. J Ambul Care Manage. 2011 Oct-Dec;34(4):354–61. doi: 10.1097/JAC.0b013e31822cbcd0. [DOI] [PubMed] [Google Scholar]
- 29.Tulenko K, Møgedal S, Afzal MM, Frymus D, Oshin A, Quain E, Pinel A, Wynd S, Zodpey S. Community health workers for universal health-care coverage: from fragmentation to synergy. Bull World Health Organ. 2013 Nov 1;91(11):847–52. doi: 10.2471/BLT.13.118745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salafsky B, Glasser M. Addressing issues of maldistribution of health care workers. Ann Acad Med Singapore. 2005 Sep;34(8):520–6. [PubMed] [Google Scholar]


