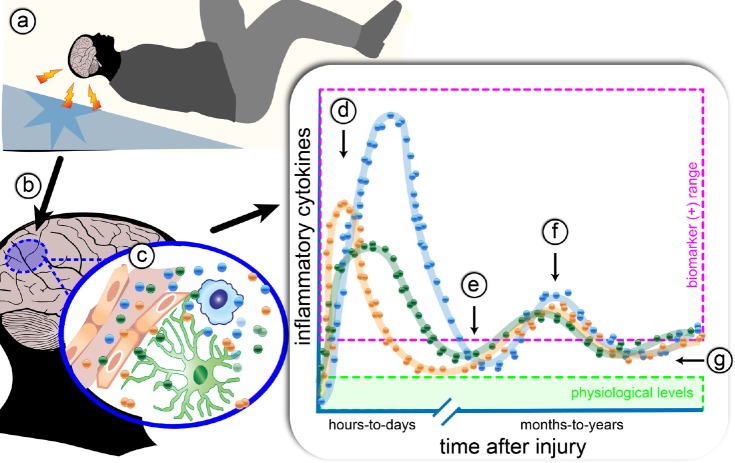
Figure 1.
The effect of traumatic brain injury (TBI) on acute cytokine response, and chronic cytokine dysregulation.
(a) A TBI causes local reactive microglia/macrophages and astrocytes (b). Humoral, cellular, and neural routes (c) lead to increase in local and systemic cytokines. The profile of the different cytokines (for example, interleukin (IL)-1, IL-6, and tumor necrosis factor α (TNFα)), indicated by the blue, orange, and green dots, have slightly different temporal patterns and max amplitude, but in general, follow a similar profile. (d) The acute inflammatory response to injury results in a surge of cytokines within the first hours-to-days after injury, which can be easily detected by biomarker assays (pink box). After the first week post-injury (e), cytokines fall below the level of sensitivity for most biomarker assays, but potentially remain above physiological levels (green box). Compounding factors, such as psychosocial stress and infection, may result in secondary spikes in inflammatory cytokines as measured in biomarker assays (f). Regardless, of the ability to measure cytokines in biomarker assays, therapeutically targeting the chronic dysregulated cytokines during the months-to-years after injury (g), could reduce cognitive, psychological, and physical complications of a TBI. Future studies are warranted to test this prediction. However, as cytokines have essential physiological functions, it will be necessary to have selective therapeutics that restore the physiological balance of cytokines, and not pan-immune suppression.