Abstract
Study Objectives:
The aim of this study was to assess the frequency of past and current psychiatric disorders among patients referred to a sleep unit for polysomnography.
Methods:
A total of 152 patients referred to the Sleep Center of Timone Hospital in Marseille were included from January 12 to March 31, 2015. Clinical data were collected using the Mini International Neuropsychiatric Interview.
Results:
The final sample consisted of 102 patients. Polysomnography helped diagnose the following common sleep disorders: obstructive sleep apnea, restless legs syndrome, insomnia, and non-rapid eye movement sleep arousal disorder. Ninety patients (88%) had psychiatric disorders. All patients (27) without a common sleep disorder diagnosis had psychiatric disorders and among patients with a common sleep disorder diagnosis 84% had psychiatric disorders. Among the psychiatric disorders a past major depressive episode was the most frequent pathology.
Conclusions:
This study shows that patients referred to a sleep unit have a high prevalence of psychiatric disorders. This may be explained by residual symptoms of psychiatric illnesses, a diagnostic misdirection, a denial of psychiatric diagnosis, or an undiagnosed somatic symptom disorder. Finally, this study shows the importance of cross-disciplinary communication considering the diagnostic heterogeneity that may represent a sleep complaint.
Citation:
Pradines M, Rey M, Dumas R, Rhondali W, Lemoine P, Azorin JM, Vedie C. Frequency of past and current psychiatric disorders in patients referred for polysomnography: a pilot study. J Clin Sleep Med. 2018;14(9):1503–1507.
Keywords: cross-disciplinary communication, polysomnography, psychiatric disorders, sleep disorders
BRIEF SUMMARY
Current Knowledge/Study Rationale: Many studies have already shown that sleep disorders are very common among patients with psychiatric disorders. Conversely, this study evaluated psychiatric disorders among patients with a sleep complaint.
Study Impact: This study found a high frequency of past and current psychiatric disorders among patients with a sleep complaint. It demonstrates the importance of trying to understand the sleep complaint even if polysomnography does not show evidence of any common sleep disorder.
INTRODUCTION
Sleep has a crucial role in the health, well-being, and physical and psychological state of individuals.1 Sleep disorders are very frequent in the general population but have long been neglected by the medical community.2 Currently, they appear as a public health problem because of their prevalence and consequences3,4 (quality of life, road accidents, accidents at work, etc.). In addition, sleep recordings are much more developed and have highlighted the high prevalence of syndromes such as sleep apnea syndrome.5 Sleep disorders are also frequent in patients with psychiatric disorders6–8 and were found to be both a risk factor for and a consequence of depression.6,9–11 However, literature about psychiatric disorders in population with sleep disturbances is scarce. In fact, when the sleep complaint is at the forefront (for example, sleepiness or diurnal fatigue), the patient will first be directed to a sleep center for a polysomnography (PSG) recording. This recording does not always provide any relevant element in understanding the sleep complaint and a differential diagnosis with psychiatric disorders will often not be considered.
The main objective of our research is to evaluate the proportion of patients with past and current psychiatric disorders in patients who underwent a PSG for sleep complaints. To achieve this aim, we carried out a pilot cross-sectional clinical study within a sleep center.
METHODS
This study was approved by the local ethics committee in compliance with French law and the Declaration of Helsinki. Verbal information about the study and its aim was given to all participants, and consent was obtained prior to enrollment in the study.
Population
The study included patients who were referred to a sleep medicine unit in Timone Hospital (Marseille, France) from January 12 to March 31, 2015, for PSG. These patients were referred to the sleep center by somaticians (26 neurologists, 21 general practitioners, 14 pneumologists, 11 ear, nose, throat specialists, 9 internists, 8 endocrinologists, 2 ophthalmologists, 1 urolo-gist, 1 company doctor, 2 dentists) and only 7 by psychiatrists. Inclusion criteria were: French-speaking patient with nighttime PSG for sleep disturbances, with written informed consent. Exclusion criteria were: age younger than 18 years, intellectual disability, other indication of PSG (epilepsy for example).
Assessments
At study entry, sociodemographic characteristics as well as height, weight, and body mass index were collected. Psychiatric assessment was made using the Mini International Neuropsychiatric Interview (MINI).12,13 It consists in a standardized and structured diagnostic examination using a nonhierarchical case-identification procedure. The MINI enables the diagnosis of 17 of the main disorders listed in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) and International Classification of Diseases, Tenth Revision. Psychiatric assessment was made during daytime hours, and the PSG was performed during the following nighttime hours.
Patients underwent a single night of PSG (using the MEDATEC system) to obtain sleep recordings. For PSG, the following channels were recorded: FP2-A1, C4-A2,02-A1 way, bilateral electrooculogram, mentalis electromyogram and bilateral tibial electromyogram, electrocardiogram, and nasal/ oral flow using nasal air pressure transducer. Pulse oximetry, respiratory efforts (thoracic and abdominal), sound recordings to measure snoring, and sleep position were simultaneously monitored. PSG analysis was performed by an experienced neurophysiologist according to the American Academy of Sleep Medicine scoring rules14 and included study of respiratory parameters and leg movements.
PSG has proved useful to help diagnose common sleep disorders. In obstructive sleep apnea (OSA), the apnea-hypopnea index is greater than 15 events/h. In restless legs syndrome, the index of periodic limb movements is greater than 15 events/h. In parasomnia, such as non-rapid eye movement sleep disorder, PSG helps reveal sleep walking and sleep terrors. In insomnia, it may support diagnosis by showing a sleep onset latency greater than 30 minutes, early awakening, and many arousals.
Statistical Analysis
Categorical variables were expressed as number (n) and percentage. The hypothesis of normal distribution of quantitative variables was tested using the Kolmogorov-Smirnov test. Quantitative variables were expressed as mean ± standard deviation when the distribution was normal or median with first and third quartile when the distribution was not normal.
We compared differences between two groups depending on the PSG results: patients with a common sleep disorder diagnosis (CSDD) versus patients without CSDD.
Quantitative variables were compared between groups using the nonparametric Mann-Whitney U test. Categorical variables were compared using the Fisher exact test when the required criteria for chi-square test were not met.
The test for Bonferroni correction was not performed, because of the exploratory nature of the analysis. All the tests were two-sided. Statistical significance was defined at P < .05. Statistical analysis was performed using the Statistical Package for the Social Sciences (version 17.0; SPSS Inc., Chicago, Illinois, United States).
RESULTS
Patients
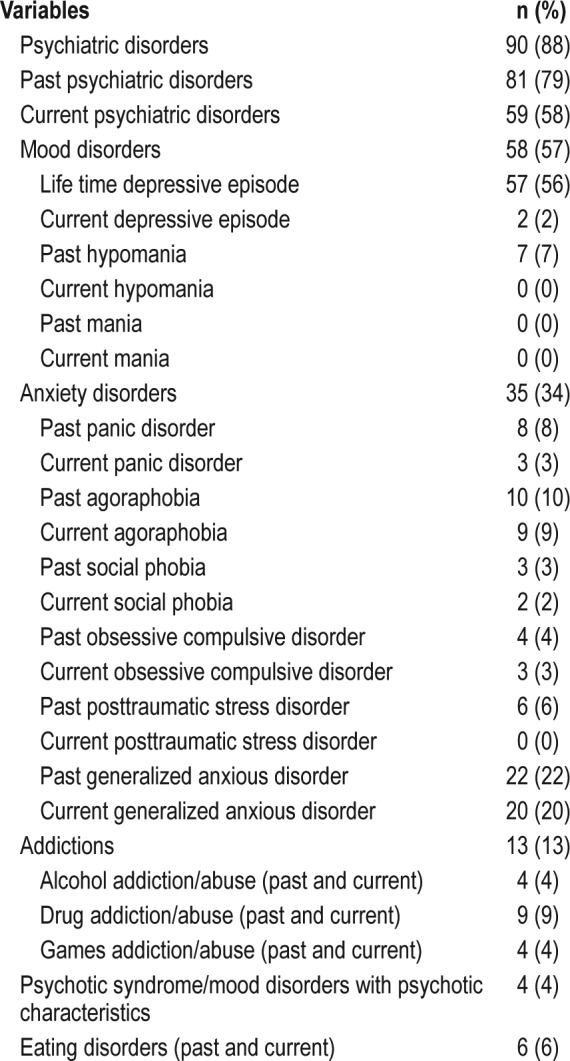
A total of 152 patients were assessed using nighttime PSG from January 12 to March 31, 2015. Only 102 of these patients were included in the current study (Figure 1). Demographic and clinical characteristics of study patients are presented in Table 1. Psychiatric disorders found in these patients are described in Table 2.
Figure 1. Flow chart inclusion/exclusion of patients.
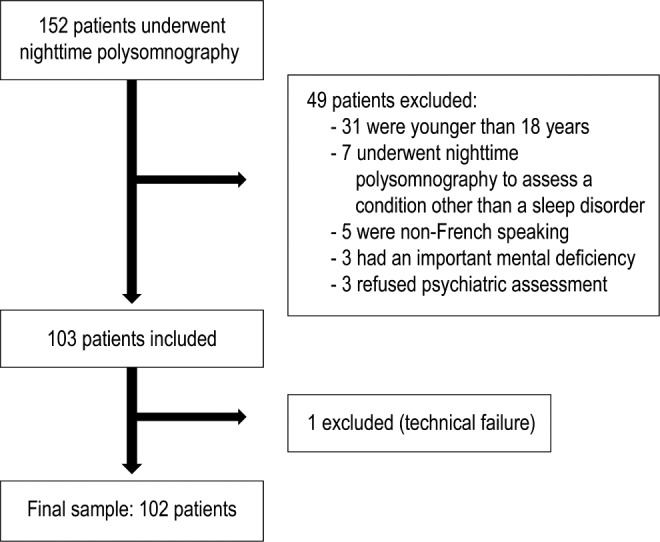
Table 1.
Demographic and clinical characteristics of study patients (n = 102).
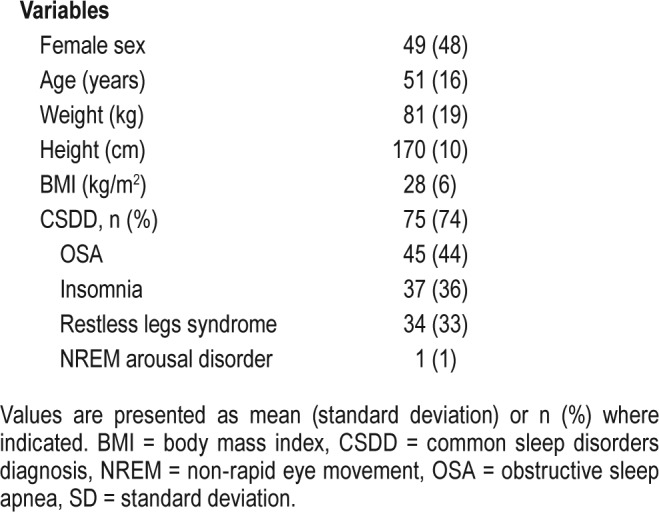
Table 2.
Psychiatric disorders in study patients.
Results of PSG
Common sleep disorders were recorded by PSG in 75 patients (74%): 45 (44%) had OSA, 37 (36%) insomnia, 34 (33%) had restless legs syndrome, and 1 (1%) non-rapid eye movement sleep arousal disorder (Table 1). Some patients suffered from multiple disturbances simultaneously. In the 27 remaining patients, PSG did not record any sleep disorder.
Psychiatric Assessment
Psychiatric assessment showed that 90 patients (88%) experienced current (58%) or past (79%) psychiatric disorders (Table 2). The proportion of patients with current or past mood disorders (57%) was superior to that of patients suffering from current or past anxiety disorders (34%). Past major depressive episode was the most prevalent disorder (56%). However only 34 patients (33%) were on current psychiatric medication.
Comparison Between Patients With and Without CSDD (Table 3)
Table 3.
Clinical characteristics and psychiatric disorders in patients with and without CSDD.
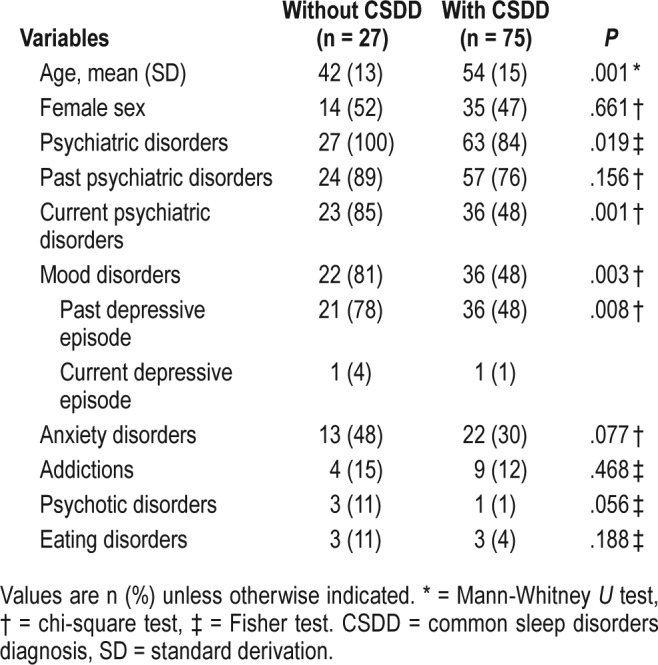
Patients with CSDD were found to be older (P = .001) than those without. Psychiatric disorders were more frequent in patients without CSDD (P = .019). In fact, all the 27 patients without CSDD had current and/or past psychiatric disorders whereas only 63 patients (84%) with CSDD had psychiatric disorders. Current psychiatric disorders were found for 23 patients (85%) without CSDD versus 36 patients (48%) with (P = .001). Among psychiatric disorders, past major depressive episode was found in 22 patients (81%) without CSDD and 36 patients (48%) with CSDD (P = .008).
DISCUSSION
Our study showed a high prevalence of psychiatric disorders in patients referred for PSG. Ninety patients (88%) experienced psychiatric disorders. This may suggest a higher prevalence than that found in the French general population: a prevalence of 31.9% was evidenced in a study15 which, like ours, used the MINI to assess psychiatric disorders.
Sleep disturbances and psychiatric disorders have been associated in several studies16–19 but interestingly, in our study, current and/or past psychiatric disorders were found in 100% of patients without CSDD versus only 84% in patients with CSDD. This is noteworthy and may be explained by several hypotheses:
Absence of CSDD does not necessarily imply total absence of sleep disturbances. The fact that 21 of these patients (78%) experienced a past depressive episode leads us to hypothesize that subjective complaints of sleep disturbances might be residual symptoms of depression, as shown in previous reports.8,10 Some of these patients could be referred to a cognitive behavioral therapy for insomnia (CBT-I) practitioner. Indeed, several recent studies20,21 have shown the effectiveness of cognitive behavioral therapy on improving quality of sleep in this population.
Diagnostic misdirection: some symptoms (such as daytime sleepiness) can be found in sleep disorders as well as in psychiatric diseases. Moreover, sleep medicine is not recognized as a specialty in France and most of these patients (95) were referred to the sleep center by somaticians. Only seven were referred by psychiatrists. These somaticians probably have varying knowledge about sleep and psychiatric disorders. Brief questionnaires22 have been developed for physicians who have never been trained in the field of sleep medicine. The questionnaires attempt to provide a basis by which to approach the more common sleep complaints by obtaining information related to specific sleep problems. This may help physicians in their decision to refer their patients to a sleep laboratory. Screening instruments for psychiatric disorders23 may be useful as well, but given that a high number of patients with CSDD had comorbid psychiatric disorders, the decision to refer to a sleep unit should be based on the results of sleep questionnaires and, of course, a full clinical history as well as a careful patient examination. In this regard, our study confirms that old age may be a risk factor for the occurrence of CSDD.3,4,17,18
Denial attitude: most of these patients may have experienced self-stigma linked to prejudices about mental disorders.15 This can lead them to attribute their health condition to sleep issues instead of mental issues.
Somatic symptom disorder: the presence of sleep complaints in psychiatric patients without CSDD could be explained by comorbid somatic symptom disorders. Unfortunately, the diagnosis of such disorders is not possible when using the MINI.
This study is significant in many ways. The MINI is a standardized and structured diagnostic instrument validated within the general population setting that permits the diagnosis of current and past psychiatric disorders.12,13 Measurement bias is therefore limited. As in our study, Hsu et al.24 used the MINI to assess psychiatric disorders in patients who visited a sleep disorders clinic. However, assessment of sleep disorders was based on sleep questionnaires, leading to less objective data than those obtained with the support of PSG.
The results of the current study should be considered in the context of several limitations. First, a recruitment bias cannot be excluded. Our sample might not be representative of the entire population of patients with sleep disturbances. Our sleep unit is a referral center. Patients in consultation are already integrated in a health care system. Most of the time they have already received medical care for their sleep disturbances. They are referred to the sleep unit to refine the diagnosis when the sleep complaint is persisting. Because psychiatric disorders may be rarely considered in this context, their prevalence could be overrepresented in our sample. Second, because the MINI does not cover all the DSM-IV diagnoses, some psychiatric disorders may have not been taken into account in our sample. Third, because patients with less common sleep disorders were not recruited in this study, we were not able to assess their comorbidity with psychiatric disorders. Finally, the lack of consensual criteria for the diagnosis of insomnia remains a major limitation.
This study found that patients who underwent PSG showed a high prevalence of psychiatric disorders. Interestingly, in our sample, psychiatric disorders were more prevalent in patients without CSDD.
This study highlights the need for a more comprehensive teamwork between psychiatrists, neurologists, general practitioners, and sleep physicians. Indeed, growing interest toward sleep disorders has led to the development of sleep recordings. However, in certain cases, PSG does not find anything, and there is no diagnosis and no further therapeutic suggestions despite the complaint and the suffering of the patient. Consultation in a sleep medicine service and PSG can be a way to detect psychiatric disorders, and thus a way to refer patients to a psychiatrist. Therefore, when the patient is referred to a sleep center, a psychiatric evaluation could be an important addition to the patient's care.
DISCLOSURE STATEMENT
Work for this study was conducted in the Sleep Center of Timone Hospital in Marseille. All authors have seen and approved the manuscript. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the members and the patients of the sleep center of Timone Hospital.
ABBREVIATIONS
- CBT-I
cognitive behavior therapy for insomnia
- CSDD
common sleep disorders diagnosis
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- MINI
Mini International Neuropsychiatric Interview
- OSA
obstructive sleep apnea
- PSG
polysomnography
REFERENCES
- 1.Beck F, Richard JB, Léger D. Prévalence et facteurs sociodémographiques associés à l'insomnie et au temps de sommeil en France. Rev Neurol. 2013;169(12):956–964. doi: 10.1016/j.neurol.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 2.National Institutes of Health. National Institutes of Health State of the Science Conference statement on Manifesations and Management of Chronic Insomnia in Adults, June 13-15, 2005. Sleep. 2005;28(9):1049–1057. doi: 10.1093/sleep/28.9.1049. [DOI] [PubMed] [Google Scholar]
- 3.Touitou Y. Troubles du sommeil et hypnotiques: impacts médicaux et socioéconomiques. Ann Pharm Fr. 2007;65:230–238. doi: 10.1016/s0003-4509(07)90041-3. [DOI] [PubMed] [Google Scholar]
- 4.Ohayon MM, Lemoine P. Répercussions diurnes de l'insomnie dans la population générale française. Encephale. 2004;30(3):222–227. doi: 10.1016/s0013-7006(04)95433-4. [DOI] [PubMed] [Google Scholar]
- 5.Colas des Francs C, Meksen B, Dinkelacker V, Roisman G, Escourrou P. Le syndrome d'apnées obstructives du sommeil en Europe: résultats de l'étude multicentrique ESADA 5eupean Sleep Apnea Data) Med Som. 2016;13(3):109–121. [Google Scholar]
- 6.Bastuji H. Sommeil et psychiatrie. Perspect Psy. 2001;40(5):401–408. [Google Scholar]
- 7.Lemoine P. Sommeil et psychiatrie. Encephale. 2011;31(3) [Google Scholar]
- 8.Brill S, Penagaluri P, Roberts RJ, Gao Y, El-Mallakh R-S. Sleep disturbances in euthymic bipolar patients. Ann Clin Psychiatry. 2011;23(2):113–116. [PubMed] [Google Scholar]
- 9.Beck F, Léon C, Pin-Le Corre S, Léger D. Troubles du sommeil : caractéristiques sociodémographiques et comorbidités anxiodépressives. Etude (Baromètre santé INPES) chez 14 734 adultes en France. Rev Neurol. 2009;165:933–942. doi: 10.1016/j.neurol.2009.01.046. [DOI] [PubMed] [Google Scholar]
- 10.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473–480. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sateia MJ. Update on sleep and psychiatric disorders. Chest. 2009;135(5):1370–1379. doi: 10.1378/chest.08-1834. [DOI] [PubMed] [Google Scholar]
- 12.Sheehan D-V, Lecrubier Y, Sheehan K-H, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(20):22–33. [PubMed] [Google Scholar]
- 13.Amorim P, Lecrubier Y, Weiller E, Hergueta T, Sheehan D. DSMIII-R Psychotic disorders: procedural validity of the mini international neuropsychiatric interview (MINI). Concordance and causes for discordance with the CIDI. Eur Psychiatry. 1998;13(1):26–34. doi: 10.1016/S0924-9338(97)86748-X. [DOI] [PubMed] [Google Scholar]
- 14.Berry RB, Brooks R, Gamaldo CC, et al. for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Technology and Technical Specifications. Darien, IL: American Academy of Sleep Medicine; 2015. Version 2.2. [Google Scholar]
- 15.Caria A, Roelandt JL, Bellamy V, Vandeborre A. Santé mentale en population générale : images et réalité : presentation de la méthodologie d'enquête. Encéphale. 2010;3(1):1–6. doi: 10.1016/S0013-7006(10)70011-7. [DOI] [PubMed] [Google Scholar]
- 16.Chan-Chee C, Bayon V, Bloch J, Beck F, Giordanella JP, Léger D. Epidémiologie de l'insomnie en France : état des lieux. Rev Epidemiol Sante. 2011;59:409–422. doi: 10.1016/j.respe.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 17.Beck F, Léon C, Léger D. Les troubles du sommeil en population générale. Sciences. 2009;25:201–206. doi: 10.1051/medsci/2009252201. [DOI] [PubMed] [Google Scholar]
- 18.Ohayon MM, Lemoine P. Liens entre insomnie et pathologie psychiatrique en population générale française. Encéphale. 2002;28:420–428. [PubMed] [Google Scholar]
- 19.Ohayon MM, Lemoine P. Sommeil et principaux indicateurs d'insomnie dans la population générale française. Encéphale. 2004;30:135–140. doi: 10.1016/s0013-7006(04)95423-1. [DOI] [PubMed] [Google Scholar]
- 20.Lovato N, Lack L, Kennaway DJ. Comparing and contrasting therapeutic effects of cognitive-behavior therapy for older adults suffering from insomnia with short and long objective sleep duration. Sleep Med. 2016;22:4–12. doi: 10.1016/j.sleep.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 21.Bathgate CJ, Edinger JD, Krystal AD. Insomnia patients with objective short sleep duration have a blunted response to cognitive behavioral therapy for insomnia. Sleep. 2017;1(1):40. doi: 10.1093/sleep/zsw012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thorpy MJ. Approach to the patient with a sleep complaint. Semin Neurol. 2004;24(3):225–235. doi: 10.1055/s-2004-835070. [DOI] [PubMed] [Google Scholar]
- 23.Beidas RS, Stewart RE, Walsh L, et al. Free, brief and validated: Standardized instruments for low-resource mental health settings. Cogn Behav Pract. 2005;22(1):5–19. doi: 10.1016/j.cbpra.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hsu SC, Liu CY, Chen NH. Psychiatric diagnoses of patients visiting a sleep disorder clinic due to dyssomnias. Psychol Rep. 2006;98(3):789–797. doi: 10.2466/pr0.98.3.789-797. [DOI] [PubMed] [Google Scholar]


