Short abstract
The incidence of tuberculosis is increasing worldwide, especially in developing countries. The prevalence of abdominal tuberculosis has been found to be as high as 12% in people with extrapulmonary tuberculosis. Peritoneal thickening and intestinal adhesions can occur in patients with abdominal tuberculosis. Inguinal hernias are extremely rare in people with abdominal tuberculosis; only 11 cases have been reported in the English-language literature, half of which involved pediatric patients. No definitive guideline on the management of such cases is available. In this report, we describe the unusual finding of an incarcerated inguinal hernia in an adult with abdominal tuberculosis and propose a therapy to treat this complicated disease based on our successful experience.
Keywords: Abdominal tuberculosis, inguinal hernia, adult, treatment, developing countries, case report
Introduction
Tuberculosis (TB) is a universal disease with an incidence that is increasing worldwide because of the high prevalence of acquired immunodeficiency syndrome and poverty, especially in developing countries.1 Abdominal TB accounts for a large proportion of cases of TB and is characterized by different presentations, such as acute abdomen, intestinal perforation or obstruction, or chronic abdominal pain.1 Inguinal hernias are extremely rare in people with abdominal TB. Additionally, no definitive guideline regarding how to manage abdominal TB in adults is currently available. In this report, we describe the unusual finding of an incarcerated inguinal hernia in an adult with abdominal TB and propose a therapy to treat this complicated disease based on our successful experience. This case is being reported to alert surgeons to the fact that an inguinal hernia and abdominal TB may coexist and to provide therapy to deal with this complicated situation in clinical practice.
Case report
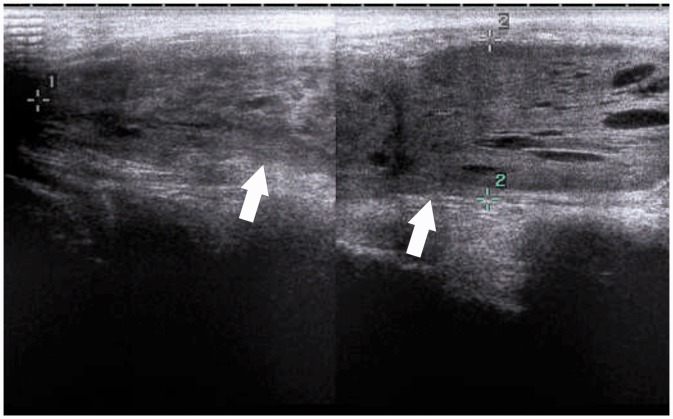
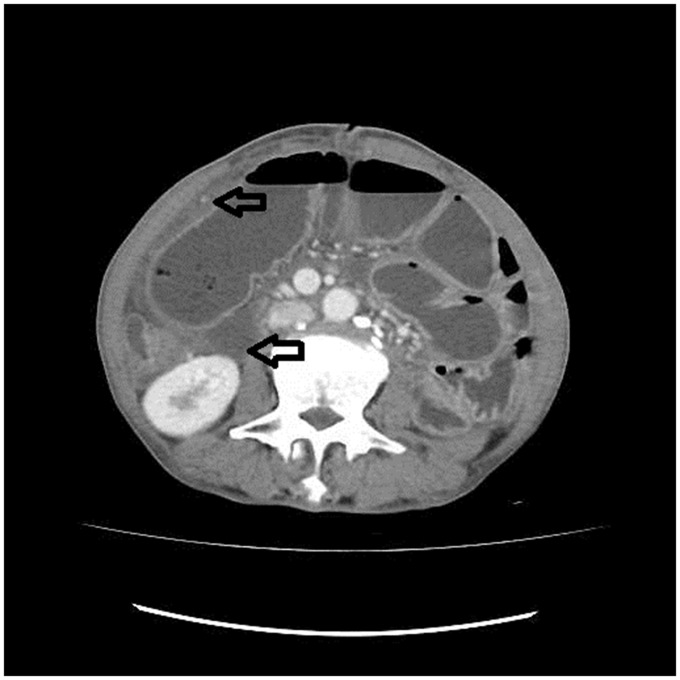
A 64-year-old man presented with a 2-month history of a non-tender right inguinoscrotal swelling that was irreducible and associated with mild abdominal pain. He had no constitutional symptoms (morning fever, night sweats, cough, or weight loss). He denied any history of pulmonary TB, alteration in bowel habits, or blood in his stools. Clinical abdominal examination revealed an irreducible right incarcerated inguinal hernia with slight abdominal distention but without tenderness or free fluid. Ultrasound confirmed a 90- × 30-mm hypoechoic mass with suspected mesentery localized to the right spermatic cord, indicating an inguinal hernia (Figure 1). Axial contrast-enhanced computed tomography of the abdomen revealed a right inguinal hernia, intestinal obstruction, and a small amount of ascites in the abdominal cavity (Figure 2). Thoracic computed tomography findings were normal, and hematological and biochemical parameters were all within normal limits. The result of a human immunodeficiency virus test was negative.
Figure 1.
Ultrasound showing a 90- × 30-mm hypoechoic mass with suspected mesentery localized to the spermatic cord (white arrow)
Figure 2.
Axial contrast-enhanced computed tomography scan of the abdomen showing intestinal obstruction, a small amount of ascites (arrow) in the abdominal cavity, and a right inguinal hernia
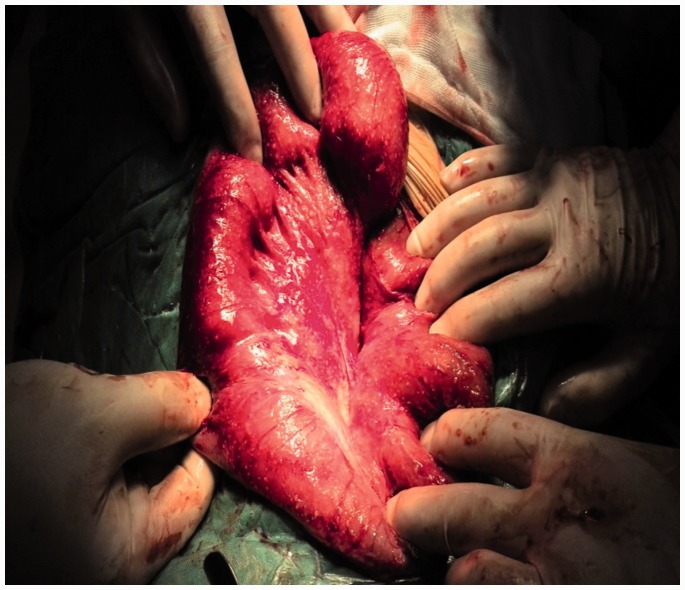
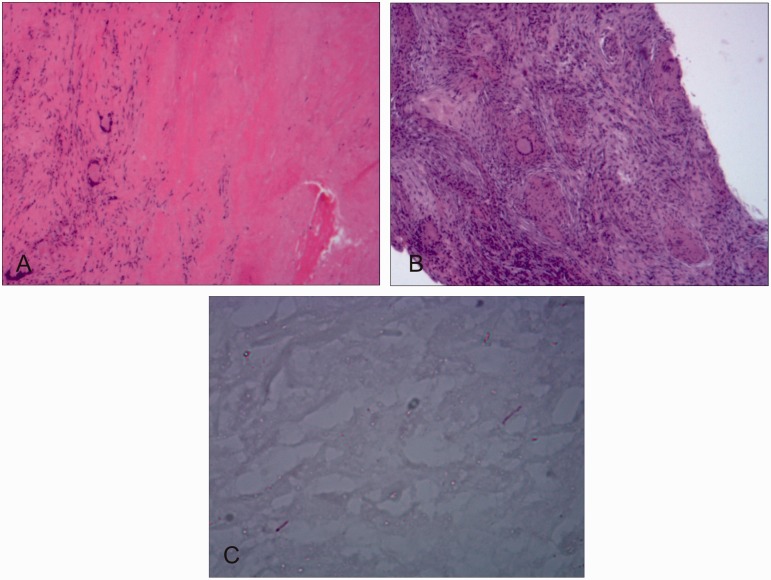
An exploratory laparotomy was performed, in which numerous white small miliary nodules were observed on the surface of the peritoneum, liver, stomach, small intestine, and colon (Figure 3). A small amount of straw-colored ascitic fluid and heavy intestinal adhesions were found in the abdominal cavity. During surgery, we found a thickened hernial sac containing small intestine and multiple miliary nodules that had resulted in adherence of the hernia to the deep inguinal ring and impeded its reduction. Intraoperative frozen section of the nodules revealed granulomatous inflammation that was suspicious for TB. In view of these findings, the patient underwent surgery with reduction of the incarcerated hernia and closure of the right deep inguinal ring. No intestinal necrosis, perforation, or stenosis was present. Histological examination showed multiple granulomas along with Langhans giant cells, epithelioid cells, and caseous necrosis, all of which were suggestive of TB (Figure 4). His postoperative recovery was uneventful. The patient was treated with antitubercular drug therapy comprising rifampicin, isoniazid, and pyrazinamide for 6 months. He thereafter experienced clinical and laboratory resolution of his symptoms. Open prolene mesh repair of the hernia was performed 1 month after the systematic antitubercular chemotherapy. No mesh-related complications occurred. He was doing well 2 years following the mesh repair without hernia recurrence.
Figure 3.
Intraoperative photograph showing numerous white small miliary nodules on the surface of the small intestine
Figure 4.
Histopathology of the miliary nodules showing (A) necrosis and multinucleated giant cells (hematoxylin–eosin, ×100), (B) granuloma and multinucleated giant cells (hematoxylin–eosin, ×100), and (C) a positive result using an anti-acid staining method (×1000)
The Ethics Committee of Beilun District People’s Hospital approved this study. The analysis was performed in accordance with the ethical standards of the hospital and the tenets of the Declaration of Helsinki/Declaration of Istanbul. The patient reported in this study provided written informed consent. Additionally, consent for publication of the individual patient data was obtained by Beilun District People’s Hospital.
Discussion
The incidence of TB is increasing worldwide, especially in developing countries.1 The prevalence of abdominal TB has been found to be as high as 12% in people with extrapulmonary TB.1 People with abdominal TB often present with acute abdomen, intestinal perforation or obstruction, or chronic abdominal pain that is difficult to diagnose.1 However, abdominal TB is not a major preoperative concern in daily practice. The preoperative diagnosis of abdominal TB based on radiologic findings is challenging because abdominal TB has no specific radiologic appearance. Computed tomography may demonstrate adhesion of the bowel loops, calcification of the mesenteric lymph nodes, and thickening of the omentum with irregular soft tissue densities.1 In the present report, axial contrast-enhanced computed tomography only showed intestinal obstruction and a small amount of ascites in the middle abdominal cavity, which can be seen in many other diseases. Thickening of the peritoneum and intestinal adhesions can also occur in abdominal TB. The incidence of inguinal hernia is extremely rare in people with abdominal TB; only 11 cases have been reported in the English-language literature, half of which involved pediatric patients.2–12
In this report, we have described the unusual finding of an adult with an incarcerated inguinal hernia associated with abdominal TB. Different from other case reports, the contents of the hernia sac in this patient were part of the small intestine. Hernias occur at sites of weakness in the abdominal wall. The layers of the abdominal wall may be weakened by the chronic abdominal TB, resulting in a potential inguinal hernia. The inflammatory adhesions caused by multiple miliary nodules between the small intestine and inner inguinal ring induced the intestinal incarceration and obstruction in the present case. However, we should remain cautious and also consider the possibility that the coexistence of the incarcerated inguinal hernia and abdominal TB was coincidental, especially because such co-occurrence has been rarely reported.7
Abdominal TB is extremely rare in our hospital. After encountering this patient, we searched the literature for reports regarding the treatment of inguinal hernias in patients with intestinal TB. Faccin et al.7 reported a 6-month regimen comprising rifampicin, isoniazid, and pyrazinamide, which provided a good result. Therefore, we adopted this regimen in the present case. However, when we reviewed the whole treatment process, we subsequently considered that we may have achieved an even better result if this regimen had been modified to a more common therapy such as isoniazid, rifampin, pyrazinamide, and ethambutol for 2 months followed by isoniazid, rifampin, and ethambutol for 4 months.
Inguinal hernias in children are repaired by high ligation (elimination) of the sac without any other type of repair, such as muscle repair.2–6 Lazarus and Pillay6 reported a case in which high ligation of the sac was performed in an 8-year-old child with abdominal TB presenting with an inguinal hernia. However, no definitive guideline regarding how to manage this condition in adults is currently available. Faccin et al.7 resected the hernia sac in a 41-year-old man with this condition. Datta et al.8 performed an anatomical repair of the hernia defect in a 60-year-old man with abdominal TB. However, neither report provided details on the specific surgical procedure. Vashist et al.9 performed a prolene mesh-plasty on man with abdominal TB in the hernial sac and reported no mesh-related complications. However, considering the potential for mesh-related infection, Basrur et al.10 performed a modified Bassini-type herniorrhaphy to strengthen the posterior abdominal wall in a 32-year-old man who presented with abdominal TB in an inguinal hernia.
The incidence of hernial recurrence is high if only high ligation of the sac or closure of the hernia neck is performed because patients with abdominal TB are at risk of enlargement of the deep inguinal ring, ascites, recurrence of intestinal obstruction, and chronic cough. The infection could spread to the mesh if mesh-plasty is immediately performed. The presence of infection after mesh hernia repair is known to jeopardize the strength of the repair and increase the incidence of recurrence.10 The placement of mesh in this area might delay or inhibit the effect of the antitubercular chemotherapy and serve as a source of chronic sepsis.10 In the present case, closure of the right deep inguinal ring was performed upon suspicion of TB. The histological examination confirmed abdominal TB. Open prolene mesh repair of the hernia was performed 1 month after systemic antitubercular chemotherapy. No mesh-related complications or hernia recurrence occurred.
With the increased prevalence of human immunodeficiency virus and the subsequent increase in TB, this problem is likely to be more frequently encountered in areas affected by TB epidemics. On the basis of our successful experience of treatment in this patient, we suggest closure of the deep inguinal ring in a first-stage operation, followed by open prolene mesh hernia repair 1 month after systemic antitubercular chemotherapy.
Acknowledgments
The authors would like to thank Jenny Hopwood (GMC Development Unit of University College London) for her language editing assistance.
Authors’ contributions
L-BZ drafted this manuscript. Y-YZ, J-QL, P-BZ, and J-WJ were involved in acquiring the data and preparing the figures. P-FL conceived of the study and revised the manuscript. All authors read and approved the final manuscript.
Availability of data and materials
All data and materials are freely available upon request. For further information, please contact Dr. Peng-fei Li (nbblyy1288@sina.com), who is responsible for the dataset.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Pattanayak S, Behuria S. Is abdominal tuberculosis a surgical problem? Ann R Coll Surg Engl 2015; 97: 414–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Narasimharao KL, Pradeep R, Mitra SK, et al. Abdominal tuberculosis presenting as inguinal hernia. Indian Pediatr 1983; 20: 790–791. [PubMed] [Google Scholar]
- 3.Bhatia S, George RK, Sharma R. Abdominal tuberculosis presenting as an inguinal hernia. Trop Gastroenterol 2005; 26: 98. [PubMed] [Google Scholar]
- 4.Dhandore P, Hombalkar NN, Ahmed MH. Unusual finding in the inguinal canal: abdominal tuberculosis presenting as inguinal hernia. J Clin Diagn Res 2016; 10: PD13–PD14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dewanda NK, Midya M, Rai NN. Hernial sac tuberculosis- an unusual presentation of gastrointestinal tuberculosis: case report with review of literature. IJSRP 2014; 4. http://www.ijsrp.org/research-paper-0214.php?rp=P262290
- 6.Lazarus J, Pillay K. Abdominal tuberculosis presenting as an inguinal hernia in a child. Urology 2011; 77: 1470–1471. [DOI] [PubMed] [Google Scholar]
- 7.Faccin M, Youssef SR, Mozetic V, et al. Inguinal hernia incarceration as a form of intestinal tuberculosis. Sao Paulo Med J 1996; 114: 1097–1099. [DOI] [PubMed] [Google Scholar]
- 8.Datta S, Vincent PJ, Singh Y, et al. Tuberculous peritonitis in a hernia sac. Med J Armed Forces India 2000; 56: 163–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vashist M, Singhal N, Verma M, et al. Abdominal tuberculosis in a hernial sac: a rare presentation. The Internet Journal of Surgery 2012; 28 http://ispub.com/IJS/28/2/13968 [Google Scholar]
- 10.Basrur GB, Naik RP, Doctor NH. Primary presentation of abdominal tuberculosis in an inguinal hernia. Indian J Surg 2006; 68: 174. [Google Scholar]
- 11.Taylor BA. Tuberculous peritonitis presenting in a hernial sac. J R Coll Surg Edinb 1986; 31: 313–315. [PubMed] [Google Scholar]
- 12.Rao BJ, Kabir MJ, Varshney S. Richter’s hernia: a rare presentation of abdominal tuberculosis. Indian J Gastroenterol 1999; 18: 33. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data and materials are freely available upon request. For further information, please contact Dr. Peng-fei Li (nbblyy1288@sina.com), who is responsible for the dataset.