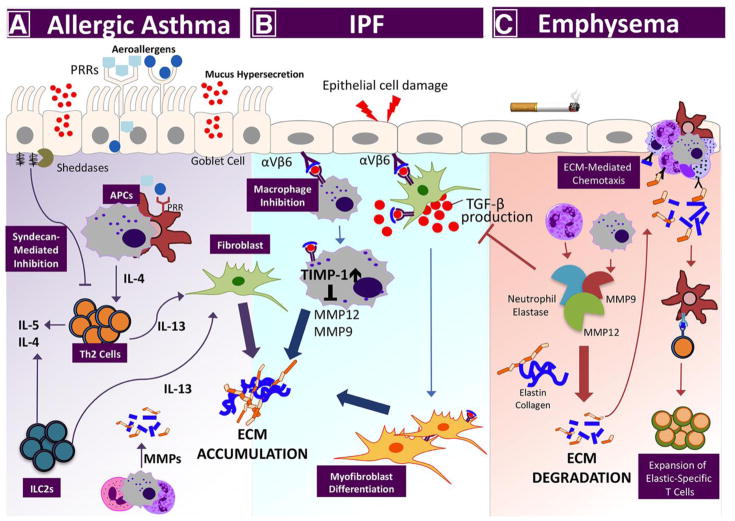
Figure 3. Lung disease pathogenesis by proteolytic enzyme/ECM imbalance.
Perturbations among the ECM networks of the lung are a hallmark feature of the most serious chronic lung diseases: asthma, IPF, and emphysema. A) In allergic asthma, aeroallergens bind pattern recognition receptors on airway epithelial cells and local antigen-presenting cells, initiating Th2-associated inflammation. Signature Th2 cytokines, (e.g., IL-13) from conventional T cells, and innate lymphoid cells (ILCs), signal through local fibroblasts to promote collagen synthesis, which leads to subepithelial fibrosis. Lung sheddases cleave proteoglycans, (e.g., syndecan-1) to release bioactive fragments that bind chemokines and impede Th2 cell recruitment. B) In response to cell injury, the immunosuppressive cytokine TGF-β promotes myofibroblast differentiation, inhibits macrophage MMP expression, and increases expression of tissue inhibitors of metalloproteinases (TIMPs) to promote idiopathic pulmonary fibrosis (IPF). (C) In emphysema, inflammatory cells secrete multiple proteinases, (e.g., MMP9, MMP12, and neutrophil elastase) that degrade collagen and elastin in the interstitial matrix. Collagen- and elastin-derived matrikines further promote lung inflammatory cell recruitment. Elastin fragments are also processed by antigen-presenting cells and presented to T cells in the regional lymph nodes to generate autoreactive, elastic-specific T cells that accelerate disease persistence and severity.