Introduction
When filling prescriptions, drug interaction alerts about serotonin syndrome are common but often misunderstood, leaving pharmacists unsure of how to proceed. This uncertainty likely results from confusion about the drugs that cause serotonin toxicity and a lack of education about the underlying physiological and pharmacological mechanisms.1,2 Here is what pharmacists need to know to prevent and identify serotonin syndrome.
Clarifying serotonin toxicity
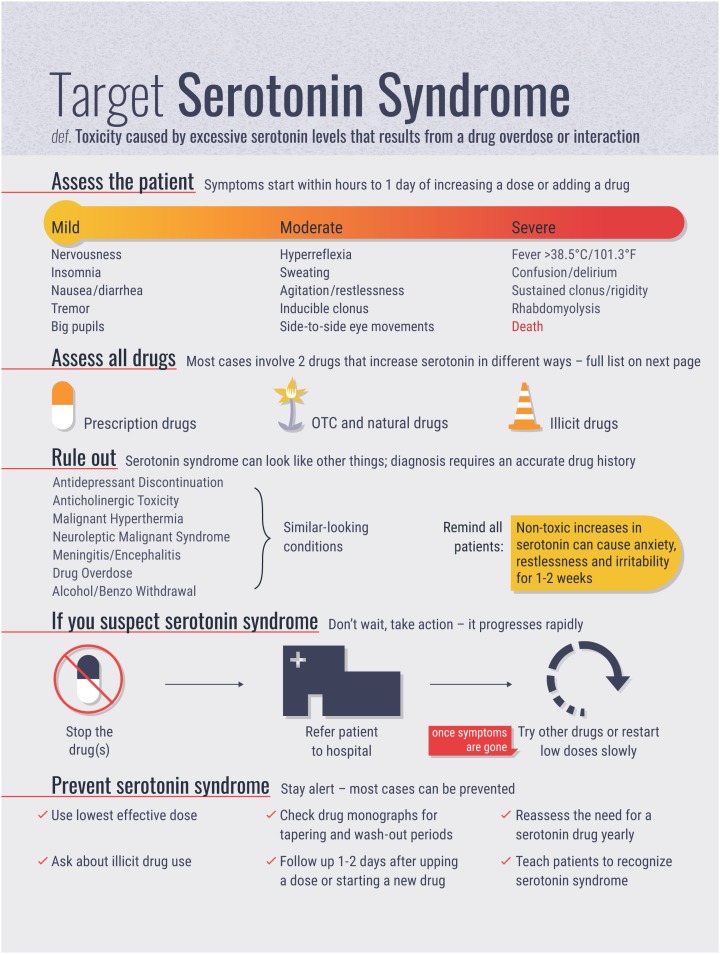
Although commonly called serotonin syndrome, serotonin toxicity is a more accurate term, since toxicity presents on a spectrum rather than as a defined set of symptoms (i.e., a syndrome).1,3 Serotonin toxicity is a drug-induced condition caused by too much serotonin in synapses in the brain.1-3 It begins within hours to 1 day of starting a new serotonin-elevating drug or increasing a dose of a serotonin-elevating agent and can be quickly fatal if untreated. Therapeutic doses of a single drug are unlikely to cause toxicity—serotonin toxicity is dose related and most often happens when 2 drugs that increase serotonin in the brain are used together, especially if they increase serotonin in different ways.1,3 Most cases do not require active medical intervention but can be managed by stopping the drug and reducing the dose. Cases that result in hospitalization are rare and occur almost exclusively when a monoamine oxidase inhibitor (MAOi) is used with a selective serotonin reuptake inhibitor (SSRI), serotonin and norepinephrine reuptake inhibitor (SNRI) or another MAOi.3
Assess the patient
Patients who have serotonin toxicity are likely to present with 1 or more symptoms of a triad of neuromuscular, autonomic and mental status changes (Table 1).1-5 Mild symptoms include nervousness, insomnia, nausea, diarrhea, tremor and dilated pupils. These can progress to moderate symptoms such as hyperreflexia (increased reflexes), sweating, agitation, clonus (rhythmic muscle spasms) and ocular clonus (side-to-side eye movements). Severe symptoms include temperature greater than 38.5°C (101.3°F), sustained clonus or rigidity, confusion, delirium and rhabdomyolysis. Patients with severe symptoms should be referred to the hospital immediately, as toxicity escalates quickly and is fatal.
Table 1.
| Neuromuscular |
|---|
| Tremor Hyperreflexia (increased reflexes)* Clonus (rhythmic muscle spasms that can be spontaneous, inducible and/or ocular)* |
| Autonomic |
| Mydriasis (dilated pupils) Diaphoresis (sweating) Tachycardia (increased heart rate) Tachypnea (increased breathing rate) |
| Mental status |
| Agitation Excitement Restlessness Confusion Delirium |
Hyperreflexia and clonus are often worse in the legs than the arms.
Serotonin toxicity that warrants hospitalization is straightforward to diagnose: classic symptoms such as bilateral, symmetric clonus in the legs more than in the arms are not seen in other conditions. Other key symptoms are clonus, hyperreflexia, tremor and agitation.1-3 However, milder serotonin elevations result in a range of symptoms that, combined with nonspecific autonomic symptoms and a lack of definitive laboratory tests, makes diagnosis difficult.1
Drugs that cause serotonin toxicity
In the brain, serotonin is formed from tryptophan, stored in the presynaptic terminal of a neuron and released into the synapse where it acts on serotonin receptors on the postsynaptic terminal. It is degraded by monoamine oxidase in the presynaptic terminal (see practice tool on next page).6 Following this pathway, there are 3 types of drugs that can increase serotonin in the brain.3 Common serotonin-elevating drugs are classified by mechanism of action in Table 2. Since serotonin toxicity is drug induced and dose related, an accurate drug history is necessary for diagnosis.
Table 2.
Drugs that increase serotonin classified by mechanism of action
| Monoamine oxidase inhibitors |
|---|
| Isocarboxazid Isoniazid Phenelzine Tranylcypromine Linezolid Selegiline Rasagiline Moclobemide Methylene blue Metaxalone |
| Serotonin reuptake inhibitors |
| Selective serotonin reuptake inhibitors: citalopram,
escitalopram, paroxetine, sertraline, fluvoxamine,
fluoxetine Serotonin norepinephrine reuptake inhibits: venlafaxine, desvenlafaxine, duloxetine Tricyclic antidepressants: clomipramine, imipramine Narcotics and pain medications: tramadol, meperidine, methadone, fentanyl Dextromethorphan Chlorpheniramine, brompheniramine St. John’s wort |
| Serotonin releasers |
| Ecstasy (MDMA) Amphetamine |
| Serotonin precursor |
| L-tryptophan |
MAOis block the MAO enzyme that breaks down serotonin.6 These serotonergic drugs—particularly those that bind to the MAO enzyme irreversibly and those that nonselectively inhibit both the MAO type A and type B enzymes—are most likely to cause toxicity.1,6 MAO-A preferentially breaks down serotonin, making MAOi-A drugs more toxic than MAOi-B. Any combination of an MAOi with another serotonin drug is risky, but never combine an MAOi with another MAOi, an SSRI or an SNRI.3 Commonly recognized MAOis are antidepressants phenelzine, isocarboxazid and moclobemide, but watch out for uncommonly dispensed MAOis such as isoniazid (irreversible, nonselective) for tuberculosis and the antibiotic linezolid (reversible, nonselective).6-8 Metaxalone, a weak MAOi, is a skeletal muscle relaxant found in the United States that can cause serotonin toxicity when used with a serotonin reuptake inhibitor.9
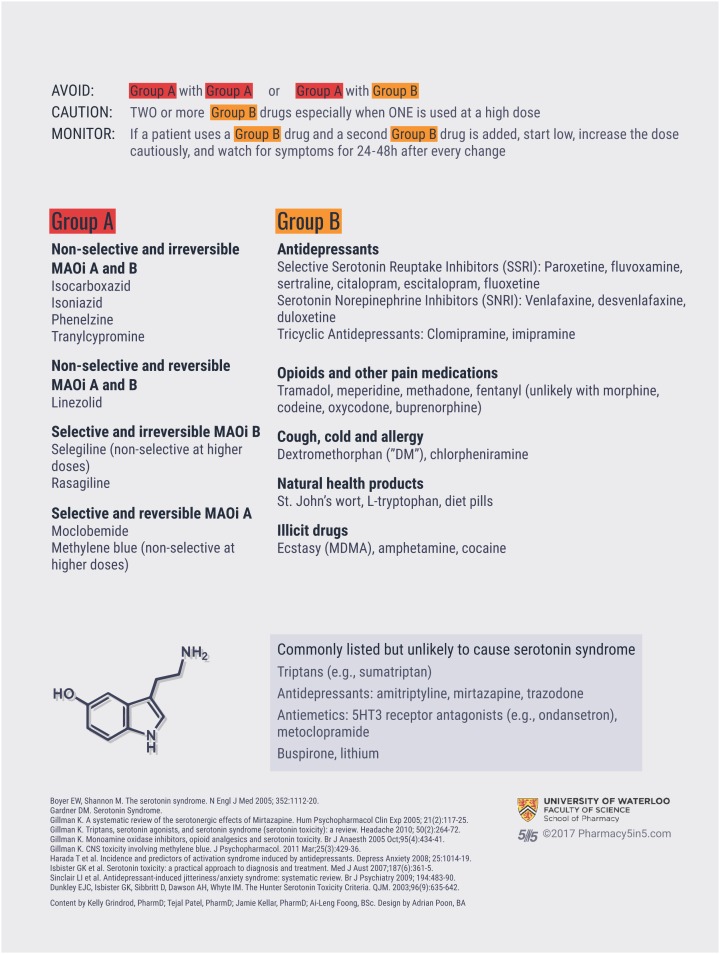
Serotonin reuptake inhibitors stop serotonin from being transported back to the presynaptic terminal to be degraded.6 Aside from MAOis, SNRIs and SSRIs are the most toxic serotonin-elevating drugs.1,2 Interestingly, the SNRI venlafaxine is more concerning than SSRIs; experts suspect that it increases serotonin by an additional, unknown mechanism.3
Certain pain medications are reuptake inhibitors. Tramadol, methadone, meperidine and fentanyl cause serotonin toxicity, but morphine analogues such as morphine, codeine, oxycodone and buprenorphine do not, as they are weaker inhibitors of the serotonin transporter.3,10
The potent tricyclic antidepressants (TCAs) cause toxicity—clomipramine and imipramine do, but amitriptyline and other TCAs do not since they are weaker inhibitors of the serotonin transporter.3,10 The herbal medication St. John’s wort is a reuptake inhibitor, as are the antihistamines chlorpheniramine and brompheniramine.5,10 Since dextromethorphan is also a reuptake inhibitor, be cautious with cough and cold preparations that combine dextromethorphan and chlorpheniramine.10
Serotonin releasers cause more serotonin to be released from the presynaptic terminal into the synapse.6 They include the often-overlooked illicit drug ecstasy (MDMA).4,10 Amphetamine is also a releaser, but methylphenidate is not.3
A drug that does not fit into these 3 categories is L-tryptophan, which can be used in various mood disorders.3 L-tryptophan can increase serotonin levels because serotonin is made from tryptophan, but the risk is low.
Drugs that do not cause serotonin toxicity
Publication of serotonin toxicity case reports in which further evaluation indicates that toxicity did not actually occur has resulted in confusion in the health care field about the implicated drugs.11,12 Adding to the confusion, the World Health Organization, Food and Drug Administration and Health Canada have stated that 5-HT3 antagonists (e.g., the antiemetic ondansetron) and triptans that are used for migraines can cause serotonin toxicity, although their pharmacological actions do not support the warnings.11-17 Serotonin toxicity is caused by activation of specific serotonin receptors, but these drugs either block the serotonin receptors or work on different receptors. Triptans activate serotonin receptors that are not involved in the mechanism of serotonin toxicity, while the 5HT3 antagonists used as antiemetics block a type of serotonin receptor that is also not involved in toxicity.4,11,14 Other drugs that are incorrectly thought to cause toxicity are olanzapine, mirtazapine, cyclobenzaprine, bupropion, trazodone, buspirone and lithium.1,3,4,11-14
In Canada, RxVigilance and First Databank are the main companies that house an updated database of drug information that is used in decision support tools for health care professionals, such as electronic medical records in physician offices and in pharmacy management systems. For example, the drug interaction checking software in Kroll, Ubik and Healthwatch use information from RxVigilance, and PharmaClik through McKesson uses First Databank (McKesson Canada Pharmacy Technology Solutions, phone call, August 14, 2017).18,19 Although RxVigilance and First Databank recognize the controversy surrounding certain implicated drugs, drug interaction checkers still flag combinations of drugs that are unlikely to cause serotonin syndrome, meaning that primary care providers and pharmacists might avoid prescribing or dispensing a medication that could be beneficial for a patient.
Rule out
The most important differential diagnoses for pharmacists are the symptoms that result from stopping or starting an antidepressant. After stopping an antidepressant, flulike symptoms, nausea, imbalance, sensory disturbances, hyperarousal and changes in mood, sleep and appetite are common.20 These symptoms start later than serotonin toxicity—within days of stopping or tapering a drug—and usually last 1 week. When starting an antidepressant or increasing a dose, anxiety, restlessness and irritability for 1 to 2 weeks is normal.21 Follow up with patients about side effects to differentiate normal jitteriness or discontinuation symptoms from serotonin toxicity. The time of symptom onset and the severity of symptoms in relation to the initiation or dose increase of a serotonergic drug will help differentiate these symptoms from those of serotonin toxicity.
Practice tips
Prevention of serotonin syndrome is key. Here are some points to remember:
Teach patients and their families/caregivers to recognize serotonin toxicity (symptoms, onset and progression) and tell them to call their prescriber or go to the hospital if they experience symptoms. If you suspect toxicity, refer them immediately since they can worsen quickly.
After recovery, recommend different drugs or lower doses. Follow up with prescribers and patients to ensure that this happens.
Ask patients about over-the-counter, herbal and illicit drug use. Remind patients to check with their prescriber or pharmacist before starting a new drug.
At annual medication reviews, check if a patient still needs a serotonin drug.
Recommend the lowest effective dose and avoid using 2 high-dose serotonin drugs at the same time.
Encourage patients to adhere carefully to taper schedules and wash-out periods. Note that drugs with long half-lives such as the SSRI fluoxetine can precipitate toxicity for 5 weeks after administration.
Follow up with patients a few days after starting a drug or increasing a dose. ■
Supplementary Material
Acknowledgments
We thank Adrian Poon who designed the infographic and serotonin physiology diagram. We thank Dr. David Gardner and Dr. Ken Gillman who provided comments on our manuscript and infographic. Dr. Gardner’s research and practice tools for antipsychotics and antidepressants can be found on his website Medication InfoShare (http://medicationinfoshare.com), and Dr. Gillman’s research on serotonin toxicity is compiled on his website PsychoTropicalResearch (www.psychotropical.info).
Footnotes
Author contributions:K. Grindrod conceived the project. All researchers were involved in drafting the manuscript and approving the final draft.
Declaration of Conflicting Interests:The authors have no conflicts of interest to declare.
Funding:No funding was received for this project.
References
- 1. Dunkley EJC, Isbister GK, Sibbritt D, Dawson AH, Whyte IM. The Hunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96(9):635-42. [DOI] [PubMed] [Google Scholar]
- 2. Boyer EW, Shannon M. The serotonin syndrome. N Engl J Med 2005;352(11):1112-20. [DOI] [PubMed] [Google Scholar]
- 3. Gillman PK. A review of serotonin toxicity data: implication for the mechanisms of antidepressant drug action. Biol Psychiatry 2006;59(11):1046-51. [DOI] [PubMed] [Google Scholar]
- 4. Ables AZ, Nagubilli R. Prevention, diagnosis and management of serotonin syndrome. Am Fam Physician 2010;81(9):1139-42. [PubMed] [Google Scholar]
- 5. Isbister GK, Buckley NA, Whyte IM. Serotonin toxicity: a practical approach to diagnosis and treatment. Med J Aust. 2007;187(6):361-5. [DOI] [PubMed] [Google Scholar]
- 6. Sanders-Bush E, Hazelwood L. 5-Hydroxytryptamine (serotonin) and dopamine. In: Brunton LL, Chabner BA, Knollmann BC. eds. Goodman & Gilman’s: The Pharmacological Basis of Therapeutics. 12th ed. New York (NY): McGraw-Hill; Available: http://accesspharmacy.mhmedical.com.proxy.lib.uwaterloo.ca/content.aspx?bookid=1613§ionid=102158475 (accessed Jul. 28, 2017). [Google Scholar]
- 7. Gillman PK. Advances pertaining to the pharmacology and interactions of irreversible nonselective monoamine oxidase inhibitors. J Clin Psychopharmacol. 2011;31(1):66-74. [DOI] [PubMed] [Google Scholar]
- 8. Woytowish MR, Maynor LM. Clinical relevance of linezolid-associated serotonin toxicity. Ann Pharmacother. 2013;47(3):388-97. [DOI] [PubMed] [Google Scholar]
- 9. Gillman PK. Metaxalone (Skelaxin) and serotonin toxicity (serotonin syndrome): warning of potential for fatalities if combined with serotonin re-uptake inhibitors. PsychoTropical Commentaries 2015;12:1-9. [Google Scholar]
- 10. Gillman PK. Monoamine oxidase inhibitors, opioid analgesics and serotonin toxicity. Br J Anaesth. 2005;95(4):434-41. [DOI] [PubMed] [Google Scholar]
- 11. Gillman PK. Triptans, serotonin agonists and serotonin syndrome (serotonin toxicity): a review. Headache. 2010;50(2):264-72. [DOI] [PubMed] [Google Scholar]
- 12. Gillman PK. Regulatory agencies (WHO, FDA) offer ill-conceived advice about serotonin toxicity (serotonin syndrome) with 5-HT3 antagonists: a worldwide problem. March 4, 2015. Available: http://psychotropical.info/serotonin-toxicity-and-5-ht3-antagonists (accessed Jul. 27, 2017).
- 13. World Health Organization. WHO pharmaceuticals newsletter. WHO Collaborating Centre for International Drug Monitoring. 2012. Available: www.who.int/medicines/publications/Newsletter_3_2012.pdf (accessed Jul. 27, 2017).
- 14. World Health Organization. WHO pharmaceuticals newsletter. WHO Collaborating Centre for International Drug Monitoring. 2014. Available: www.who.int/medicines/publications/PharmNewsNo4_2014.pdf (accessed Jul. 27, 2017).
- 15. U.S. Department of Health and Human Services. FDA drug safety communication: FDA warns about several safety issues with opioid pain medicines; requires label changes. March 22, 2016. Available: https://www.fda.gov/Drugs/DrugSafety/ucm489676.htm (accessed Jul. 27, 2017).
- 16. Health Canada. Summary safety review—serotonin blocking drugs (serotonin antagonists) ALOXI (palonosetron), ANZEMET (dolasetron), KYTRIP (granisetron) and generics and ZOFRAN (ondansetron) and generics—serotonin syndrome. May 14, 2014. Available: www.hc-sc.gc.ca/dhp-mps/medeff/reviews-examens/serotonin-eng.php (accessed Jul. 27, 2017).
- 17. Gillman PK. Is there sufficient evidence to suggest cyclobenzaprine might be implicated in causing serotonin toxicity? Am J Emerg Med 2009;27(4):509-10. [DOI] [PubMed] [Google Scholar]
- 18. Vigilance Santé. Drugs database and pharmaceutical software for health professionals and pharmacists. Available: www.vigilance.ca/ (accessed Aug. 14, 2017).
- 19. First Databank. Drug data drug database. Available: www.fdbhealth.com/ (accessed Aug. 14, 2017).
- 20. Kok RM, Reynolds CF., III Management of depression in older adults: a review. JAMA 2017;317(20):2114-22. [DOI] [PubMed] [Google Scholar]
- 21. Sinclair LI, Christmas DM, Hood SD, et al. Antidepressant-induced jitteriness/anxiety syndrome: systematic review. Br J Psychiatry 2009;194(6):483-90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


