Figure 2.
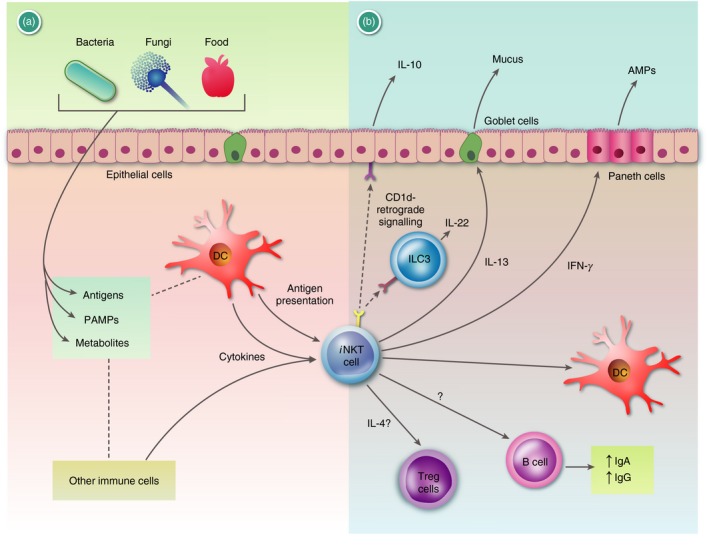
Graphic summary of the functions of invariant Natural Killer T (i NKT) cells at mucosal surfaces: (a) i NKT cells at mucosal surfaces can respond to many signals. Bacterium‐, fungus‐, and food‐derived products can influence the tissue‐resident cells of the mucosa and the local immune cells, via antigens, pathogen‐associated molecular patterns (PAMPs), and metabolites (Box 1). These can alter the frequency and function of various cells (not depicted). Antigens for i NKT cells can be either self‐antigens or antigens derived from the microbiota (Table 1). Some of the bacterially derived glycolipids binding to CD1d can also be inactive, competitive inhibitors. Furthermore, i NKT can respond to local cytokines either directly or synergistically with CD1d‐bound antigens. (b) Invariant NKT cells are known to influence the mucosal microenvironment and the microbial composition via (1) cytokines that they produce and (2) direct cell–cell contact. (1) Invariant NKT cell derived interferon‐γ (IFN‐γ) or interleukin‐13 (IL‐13) has been shown to activate Paneth cells or goblet cells to increase production of anti‐microbial peptides (AMPs) or mucus, respectively. Furthermore, i NKT cells have been shown to boost IgA and IgG production by B cells. Finally, CD1d−/− mice had a lower frequency of CD304+ regulatory T (Treg) cells in the mesenteric lymph nodes and i NKT cell‐derived IL‐4 was implicated.46 (2) Binding of i NKT cells to CD1d can induce, via a CD1d‐retrograde signal, IL‐10 or IL‐22 production by epithelial cells or innate lymphoid cells (ILC3s), respectively, which both support mucosal integrity. Please note that the figure does not attempt to represent a particular mucosal surface, but summarizes available data derived from various tissues and sides. For additional references we refer to the main text and Box 1. AMPs, anti‐microbial peptides; ECs, epithelial cells.
