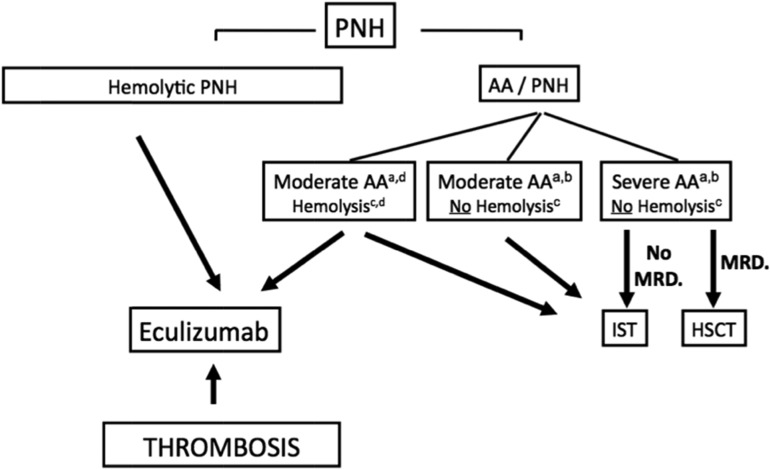
Figure 2.
Algorithm to manage patients with PNH. (a) Indications for treatment are severe AA (2 in 3 blood counts, including absolute neutrophil count <500/μL, absolute reticulocyte count <60 000/μL, and platelet count <20 000/μL) or in cases of moderate AA, where the patient needs transfusion support or has infectious complications because of a low neutrophil count. (b) The presence of a PNH clone in this setting highlights the underlying autoimmune-mediated process in favor of an idiopathic AA and not an inherited disorder, and should also make physicians think about thrombosis upon suggestive clinical signs, because PNH is a known predisposition to thrombosis complications. Clearly, complement inhibitory therapy has no effect on the BM-failure component of the disease and should not be used in this situation. (c) The level of hemolysis is indicated by lactate dehydrogenase (LDH). Significant hemolysis is considered >2 times LDH. (d) Exceptional cases of AA-PNH syndrome with significant intravascular hemolysis may require HSCT or IST treatment of BM failure and eculizumab for the hemolysis, and should be discussed on a case-by-case basis. AA, aplastic anemia; ATG, antithymocyte globulin; HSCT, hematopoietic stem cell transplantation; IST, immunosuppressive therapy; MRD, matched related donor; PNH, paroxysmal nocturnal hemoglobinuria.