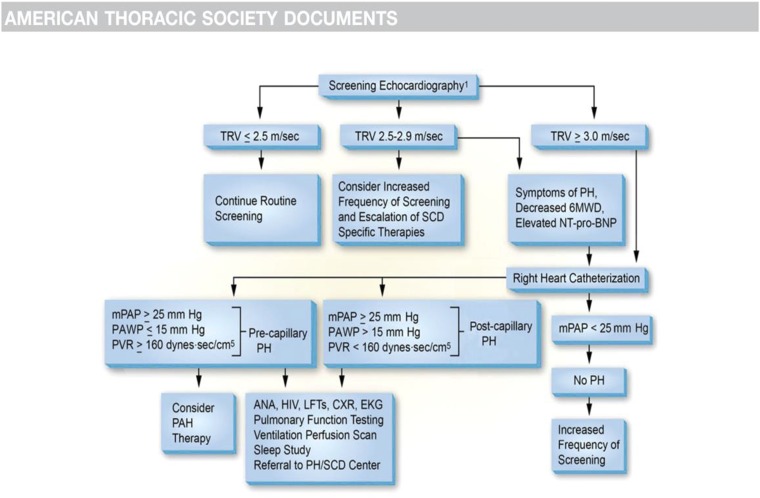
Figure 7.
Recent consensus guidelines for PH in SCD. Guidelines from the ATS, the American College of Chest Physicians, and the Pulmonary Hypertension Association have been published. Experts in pediatric and adult SCD, cardiology, and pulmonary medicine developed a recommended approach to screening and therapy for adult patients with SCD. The consensus statement argued for screening using Doppler echocardiography, plasma NNT-proBNP testing, and (if indicated) right heart catheterization to identify adult patients at the highest risk of death for additional diagnostic testing and potentially more aggressive therapies as indicated by the clinical scenario. For all patients with high TRV or NT-proBNP levels, the intensification of SCD-specific care is recommended with hydroxyurea, oxygen, iron chelation, or other interventions, as indicated. It is recommended that patients with borderline TRV values of 2.5 to 3.0 m/s undergo additional risk stratification with NT-proBNP and 6-minute walk testing. For this group with an NT-proBNP level >164 pg/mL and a 6-minute walk distance (6MWD) <333 m, or if TRV is ≥3.0 m/s, right heart catheterization is recommended to define group 1 vs group 2 hemodynamic parameters. The treatment of patients with PAH (group 1 hemodynamics) was limited to Level C evidence based on a lack of randomized placebo-controlled trials. However, until such evidence exists to change management, patients with PAH hemodynamic variables (pulmonary artery mean pressure ≥25 mm Hg and a pulmonary capillary wedge pressure ≤15 mm Hg, with pulmonary vascular resistance [PVR] >160 dyn·s/cm5) should be considered for PAH-specific therapy after fully maximizing underlying SCD-specific care. A number of case series have been published suggesting that phosphodiesterase-5 inhibitors, prostanoids, and endothelin receptor blockers may be effective in these patients.41-43 Reprinted with permission of the American Thoracic Society. Copyright © 2017 American Thoracic Society. Cite: Klings ES, Machado RF, Barst RJ, et al; American Thoracic Society Ad Hoc Committee on Pulmonary Hypertension of Sickle Cell Disease/2014/An official American Thoracic Society clinical practice guideline: diagnosis, risk stratification, and management of pulmonary hypertension of sickle cell disease./Am J Respir Crit Care Med./189/727-740. The American Journal of Respiratory and Critical Care Medicine is an official journal of the American Thoracic Society.